Physical Inactivity in Children with Asthma: A Resource for Physiotherapists
Contributors: Amy Murray, Chrisostomos Koutsos-Grantham, David Cowan, Rui Ling Lee, Shuen Wen Lim and Tommy Flanagan.
Introduction[edit | edit source]
Welcome to this online Physiopedia resource on Physical inactivity in children with Asthma: A Resource for Physiotherapists. This page has been designed by a group of 4th Year Physiotherapy students from Queen Margaret University in Edinburgh, as part of the Contemporary and Emerging Issues in Physiotherapy module.
Why is there a need for this resource?
Currently there are numerous learning resources for adults with asthma and for physiotherapists aimed to treat adult patients. However, there is a lack of paediatric patient focused resource which correlates to the lack of literature in paediatric asthma. This learning resource is therefore target for final year physiotherapy students and newly-qualified physiotherapists to enhance their familiarity and confidence regarding childhood asthma. As referred down in the Physiopedia page later, childhood asthma in increased in prevalance, and the added pressure that has been placed in acute care services has highlighted the importance of better asthma management in children to minimise hospital admissions. Physiotherapists can play a vital role in education, symptom management and participation roles for children of all ages with asthma.
This online resource will take approximately 10 hours to complete and may be used for self-study or continuing professional development (CPD), however, this should be viewed as a rough guide due to the diverse learning styles and preferences people possess. In order to facilitate this, the resource has been split into several sections, which enables the user to undertake the learning and activities as and when required. Users can choose to complete the resource on their own, with fellow work colleagues and managers or as a group with feedback given on the appropriate section. Within the ten hours spent to complete this online resource, all five learning outcomes listed below should be achieved.
This learning resource has been designed to be informative, interactive and engaging for the user, with maximum benefit gained when full cooperation and application is shown. The user will be required to undertake in-depth reading, critical reflective practice, quizzes, watch videos and complete short clinical case studies to enhance and facilitate a deeper learning.<br>As mentioned above, peoples learning styles vary considerably and due to life being multimodal there are seldom instances where one mode is used, or is sufficient, therefore a diverse range of material has been incorporated to address the different learning styles. Prior to beginning this resource it may be beneficial to undertake the VARK learning styles questionnaire in order to correctly identify your preferred learning style (LINK).
Included in the learning resource will be three different types of action boxes, which all have a different colour and require a different action. They are key points (red), activity (blue) and reflection (green), and will look as follows:
Aims[edit | edit source]
This interactive online resource targeted at final year physiotherapy students and newly qualified physiotherapists aims to:
1) Develop and expand their clinical knowledge on childhood asthma
2) Understand the impacts of physical inactivity via analysis of evidence-based research, theory, policy documents and elements of interactive learning
3) Encourage reflection to highlight physiotherapist attitudes and skills to managing asthma in children
Although this online resource highlights in detail many of the skills and resources needed when managing physical inactivity in children with asthma, further guidance and training may be required for application within clinical practice.
Learning Outcomes[edit | edit source]
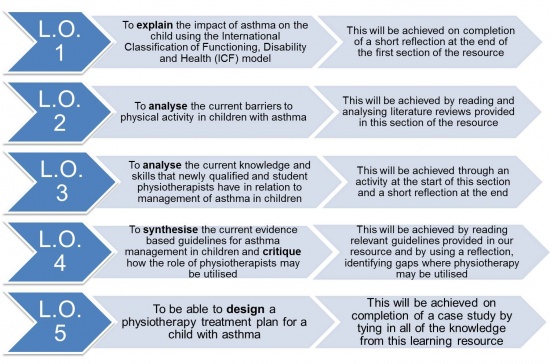
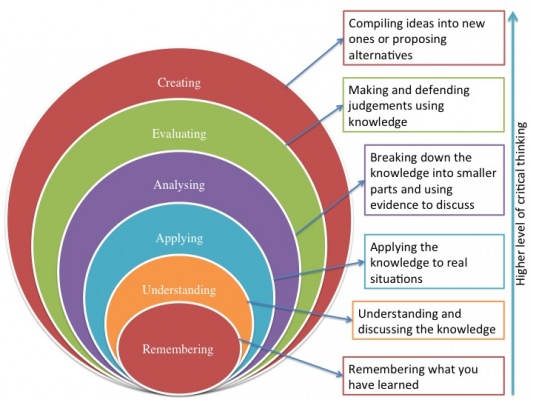
The learning outcomes outlined in Figure 1. below have been formulated using Blooms Taxonomy (reference) in order to establish the appropriate level of proficiency which is expected of newly qualified band 5 physiotherapists with particular reference to the Knowledge and Skills Framework (KSF) LINK.
Figure 1. Learning Outcomes
Figure 2. Bloom's Taxonomy
How much do you know about Asthma?[edit | edit source]
According to the Global asthma report which was produced in 2014 by the Global Asthma Network (GAN) the most recent revised estimate is said to be approximately 334 million people that suffer from asthma worldwide and therefore the burden of disability is extremely high. This figure is inclusive of both adults and children. GAN is part of a worldwide collaboration that includes over half of the world's countries in order to statistically analyze asthma and its potential difficulties it can cause, in order to provide data required by the World Health Organisation (Global Asthma Network, 2014. Asher and Pearce, 2014).
So how much do you know about Asthma?
Please click here to access the quiz!
Section 1: Background of Childhood Asthma[edit | edit source]
Activity: Please spend a few minutes watching this Youtube video on Childhood asthma to familiarise yourself with symptoms, causes and available treatment options.
Definition, Incidence and Prevalence[edit | edit source]
Asthma is an inflammatory disorder of the airways characterised by “paroxysmal or persistent symptoms such as dyspnea, chest tightness, wheezing, sputum production and cough, associated with variable airflow limitation and a variable degree of hyperresponsiveness of airways to endogenous or exogenous stimuli” (Canadian Thoracic Society 2010).
Exercise-induced bronchoconstriction (EIB), defined as the transient narrowing of the lower airways following exercise, is common among adolescents (Johansson et al. 2016). In the UK, approximately one in every 11 children are currently receiving treatment for asthma (Asthma UK 2016).
Causes and Classification[edit | edit source]
(Asthma Institue of Michigan, 2017)
Statistics[edit | edit source]
In Scotland, 368,000 people (1 in 14) are currently receiving treatment for asthma. This includes 72,000 children and 296,000 adults (Asthma UK 2016).
Developed by Asthma UK, the SAS visual analytical data can pull together information from locations all over the UK to see the prevalance rates, hospital admissions and percentage of population in the UK that have asthma and actively seek treatment for this.
Please click on the following link to acces the Asthma Uk analytic tool: Asthma UK, SAS Visual Analytical Data
Physical Activity[edit | edit source]
Definition, Incidence and Prevalance[edit | edit source]
The World Health Organization (WHO) defines physical activity as “any bodily movement produced by skeletal muscles that requires energy expenditure” (WHO 2016).
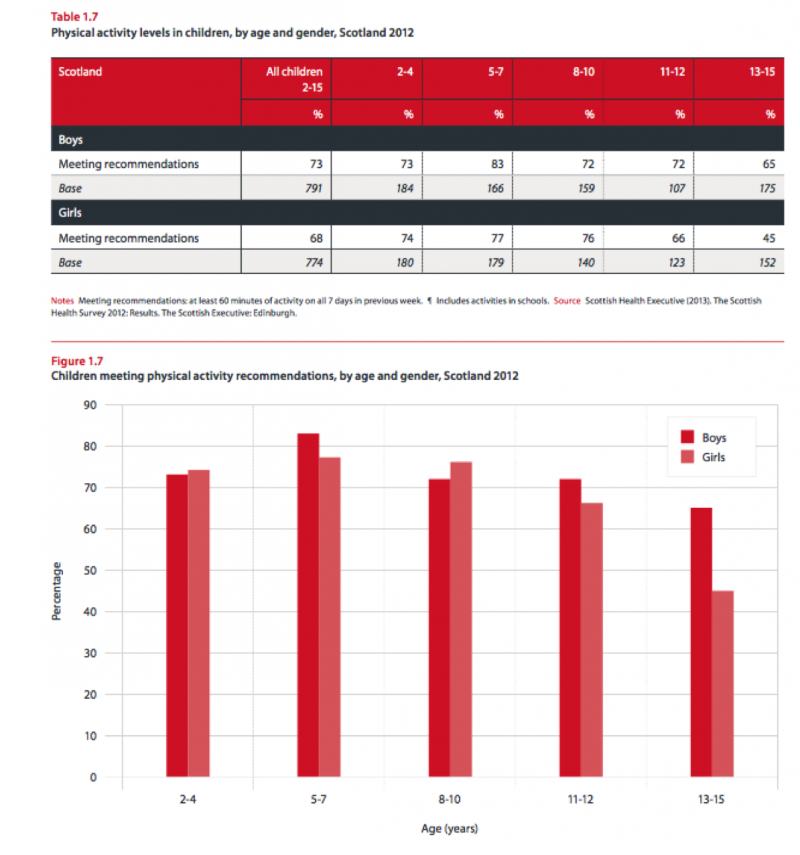
Children and adolescents aged 5-17 years old are recommended to do at least 60 minutes of moderate to vigorous-intensity physical activity daily, including muscle and bone strengthening activities at least 3 times a week. (WHO 2016). Even with the knowledge of the benefits of physical activity, participation rate is reported to be insufficient worldwide. Globally, for adolescents that are aged 11-17 years old, it has been found that 81% of them were insufficiently physically active in 2010 (WHO 2016). In Scotland, the Scottish Health Survey in 2015 established that 27% of children aged 2-15 years did not meet the physical activity recommendations, which included school-based activity (Scottish Government 2016).
Children with asthma are generally less active than their healthy peers (Williams et al. 2008). A study by Lang et al. found that children with asthma did an average daily physical activity of 116 minutes compared to that of healthy children of 146 minutes, and children with asthma only did less than 30 minutes of physical activity a day (Lang et al. 2004). Children with moderate-to-severe asthma were also found to have lower physical activity levels than children with mild asthma (Lam et al. 2016).
Statistics[edit | edit source]
- In Northern Ireland, 19% of adults watch television for more than four hours a day at the weekend.
*In Scotland, adults spend an average of more than five and a half hours a day sedentary.
*In England, 83% of 16 to 24 year olds meet physical activity recommendations; and only 30% of over 75's do.
*In Wales, 53% of primary schools and 15% of secondary schools have two hours of physical education per week. (BHF, 2015)
Sedentary Behaviour[edit | edit source]
Definition, Incidence and Prevalance[edit | edit source]
The Sedentary Behaviour Research Network (SBRN) defines sedentary behaviour as “any waking activity with an energy expenditure ≤ 1.5 metabolic equivalents and a sitting or reclining posture” (SBRN 2016). The American Academy of Pediatrics recommends children and adolescents to reduce their sedentary behaviour to less than 2 hours per day (American College of Sports Medicine 2014).
Statistics[edit | edit source]
Relationship Between Physical Activity, Sedentary Behaviour and Obesity in Children with Asthma[edit | edit source]
Physical activity is essential for the normal growth and development of children and adolescents (Hills et al. 2007; Hills et al. 2010; Hills et al. 2011). 60 minutes of physical activity a day has been shown to improve a child’s cardiovascular and bone health, improve their self-confidence and allow development of new social and motor skills (Department of Health 2011; Longmuir et al. 2014). It can reduce sedentary behaviour (Pearson et al. 2014), and is crucial in the prevention of becoming overweight and obese (Strong et al. 2005; Hills et al. 2011), and can contribute to present and future health and wellness by imprinting healthy behaviour habits, reducing risk of future chronic disease (Longmuir et al. 2014).
There is evidence to show that physical activity can improve the asthmatic child’s aerobic and anaerobic fitness (Strong et al. 2005). Physical activity engagement can also reduce school absenteeism, doctor consultations, reduce medication (Welsh et al. 2005), and improve the child’s ability to cope with asthma (van Veldhoven et al. 2001).
There is evidence to show that physical activity can improve the asthmatic child’s aerobic and anaerobic fitness (Strong et al. 2005). Physical activity engagement can also reduce school absenteeism, doctor consultations, reduce medication (Welsh et al. 2005), and improve the child’s ability to cope with asthma (van Veldhoven et al. 2001).
Impact of Asthma on Physical Activity[edit | edit source]
ICF Model[edit | edit source]
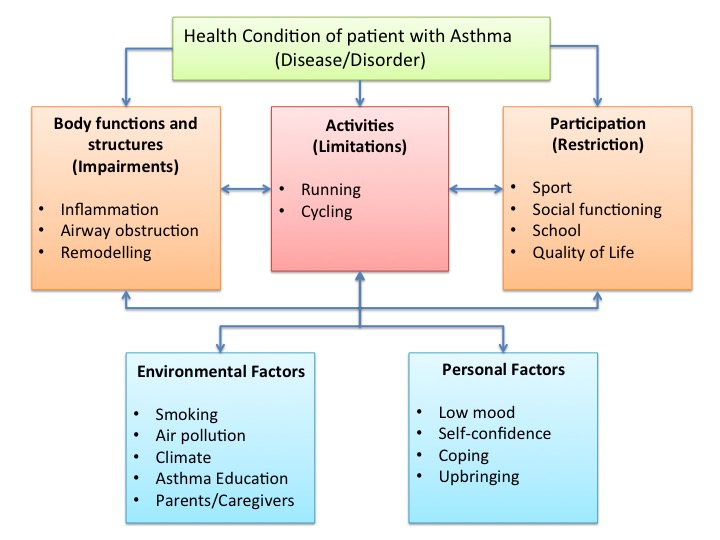
The International Classification of Functioning, Disability and Health (ICF) model is a classification of health and health-related domains and describes how people live with their health condition (WHO 2002). According to the ICF, asthma can influence participation of the child in areas such as sport, school activities, social impact and quality of life (van Gent et al. 2008). Personal and environmental factors such as their parents and asthma education can also play a role in how children with asthma function.
Challenges and Perceived Barriers to Physical Activity[edit | edit source]
There are 3 main barriers shown in figure( ) that are involved with the inability to undertake physical activity. These are:Parental support, Beliefs of the child and School environment.
Parental Support
Parental activity-related support has the ability to influence a child’s physical activity levels (Gustafson and Rhodes 2006). A study done in 2004 showed that about one in five parents agree that exercise is harmful for children with asthma, and one in four parents are afraid that exercise would cause their child to fall sick (Lang et al. 2004). Dantas et al established that 37% of mothers imposed restrictions to their children’s physical activity due to negative opinions about asthmatics doing physical activity, perception of children’s dyspnea after running on a treadmill, mother’s anxiety level and children’s asthma severity (Dantas et al. 2014).
Beliefs of the child
Many children with asthma believe that limitations on their activity are an inevitable part of having asthma (Callery et al. 2003). Williams et al. (2008), also suggested that the “desire to meet socially defined forms of normality or "ordinariness", thereby maintaining membership of a valued social group and avoiding stigma or social exclusion” appears to be an important factor affecting participation of physical activity in children with asthma. This may result in low levels of self-efficacy, especially when physical activity engagement is valued amongst their peers.
School environment
Studies have shown that a major problem for teachers were differentiating normal consequence of exertion from physical activity to breathlessness due to asthma (Williams et al. 2010). Children may more likely be asked to sit out of physical activity in school so as to reduce the risk of an asthma exacerbation, thereby encouraging children with asthma to not participate in physical activity. Hence, it is important for school teachers to learn to recognise the right signs and symptoms so as to better manage the child’s condition and not send the wrong message to the child with regards to their activity participation.
Addressing barriers: Asthma education is important in the child, parent and teachers. Asthma education for children can promote active involvement and facilitation of learning from other’s shared experiences, leading to improved confidence in their own strength and empowerment, as well as their sense of coherence (SOC) in managing their own condition (Trollvik et al. 2013). However, educating the child with asthma about the feasibility and benefits of physical activity will not be effective if the family and school contexts are not also persuaded to encourage and facilitate participation (Coleman et al. 2001; Williams et al. 2008). Parents and teachers also need to be educated on how and when children with asthma can participate in physical activity, how to adjust medication before and during periods of extended activity and how to differentiate between limitations at times of asthma exacerbation and overall limitations (Mansour et al. 2000).
</div>
=== Reflection: Learning Outcome 1 ===
Section 2: Medical Management and Current Policies[edit | edit source]
Asthma UK[edit | edit source]
Asthma UK is organisation whose goals are to raise awareness of asthma and to support children suffering with asthma. It’s ultimate objective is raise funding for asthma research to potentially find a cure for asthma and new innovations in the treatment of asthma.
Child having an asthma attack - Asthma UK guidelines outline that you are if any of the following happen:
- Your reliever (inhaler) isn't helping or lasting over four hours.
*Your symptoms are getting worse (cough, breathlessness, wheeze or tight chest)
*You're too breathless or it's difficult to speak, eat or sleep
*Your breathing is getting faster and it feels like you can't get your breath in properly.
Parents, teachers ,coaches and the child themselves are expected to know these signs and symptoms to facilitate early intervention and avoid panic. This is especially important when it comes to children with asthma participating in exercise as there is an increased risk of an asthma attack. The child themselves should have an asthma action plan which parents are also aware to help in these situations (Gibson 2004).
This is the asthma uk guidelines of what to do in case of an asthma attack:
- Sit up straight - don't lie down. Try to keep calm.
*Take one puff of your reliever inhaler (usually blue) every 30-60 seconds, up to a maximum of 10 puffs.
*If you feel worse at any point while you're using your inhaler or you don't feel better after 10 puffs or you're worried at any time, call 999 for an ambulance.
*If the ambulance is taking longer than 15 minutes you can repeat step 2.
Asthma UK advocate the benefits of exercise in children with asthma and recommend they spend at least one hour a day doing some kind of physical activity. They feel as long as the child is managing their asthma well and keeing a good routine with taken their medication exercise will benefit them and improve their confidence about their asthma.
While asthma UK have clear guidelines on what to do in case of an asthma attack and how to handle it, they offer no clear guidance on the intensity or timing of exercise in children with asthma . This is an area of research which would greatly benefit physiotherapists in dealing with pediatric patients with asthma as will will allow use to design an exercise regime and treatment which is backed up by scientific evidence and is shown to be safe. This is an area in which the foundation could provide future research in especially as obesity in children becomes an increasing problem in Britain (Dehghan et al. 2005).
SIGN and NICE[edit | edit source]
While the SIGN guidelines provide similar information on what to do in case of an asthma attack ,there is little focus on addressing the efficacy and effectiveness of physical exercise in children with asthma. There is a larger emphasis placed on the medical aspect of asthma management and allergen avoidance. In the (SIGN guidelines, 2016) for management of asthma there is only a short mention of improving dietary intake and incorporating exercise based interventions, however this is in relation to weight loss in children and not as a health management strategy in unison with medical management regardless of the child's weight factors.
NICE (2016a) state that there is no specific exercise plan for children who have asthma, and offer no time frame or intensity on the amount of exercise a child should do .They say it is appropriate to advise these patients regarding the precautions of exercise induced asthma and how to manage this (NICE, 2016b). Again this is a area in which the NICE guidelines could seek to improve by developing guidelines on the recommended timing and intensity of exercise for children with asthma.
Asthma Control Test[edit | edit source]
The asthma control test(ACT) was developed as a tool to identify patients with poorly controlled asthma. It is a short, simple questionnaire that patients can do themselves to identify if their asthma may be poorly controlled. The questionnaire is age specific as they have a questionnaire with facial expressions aimed at kids 4 to 11 which makes it easier for them to identify their symptoms. Another asthma control test is aimed at children 12 years and older. A score of 19 or less identifies patients with poorly controlled asthma. The ACT has been shown to be reliable and responsive to changes in asthma management in patients (Kennedy and Jones 2007).
Section 3: The Role of Physiotherapy[edit | edit source]
Physiotherapists have a wide intervention scope for children with asthma however numerous newly-qualified physiotherapists are unaware of their extensive role for the management of respiratory conditions in children.
Prior to reading the description of the various roles of the physiotherapist in the management of children with asthma, complete the quiz presented below to understand your baseline knowledge:
<span style="font-size: 13.28px;" />
<span style="font-size: 13.28px;" />
<span style="font-size: 13.28px;" />
<span style="font-size: 13.28px;" />
<span style="font-size: 13.28px;" />
The SIGN guidelines for managing asthma in children are not effective at highlighting the role of a physiotherapist as a member of the asthma symptom management team.
Instead, this guideline in particular is focused almost entirely on the medical approach to managing symptoms. More specifically, in the section of the guideline concerning what a parent can do to help manage their child’s asthma, only the following three instructions are mentioned:
- making sure the child takes their asthma medication when they should,
*avoiding exposure of the child to cigarette smoke
*encouraging the child to lose weight IF necessary (SIGN 2014)
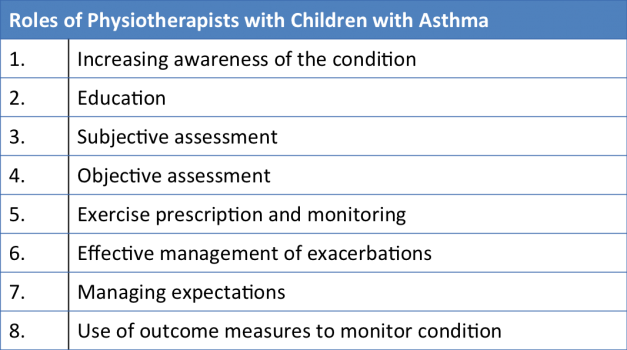
The desired shift from acute setting treatment to community setting treatment in an attempt to decrease the financial aspect of healthcare and reduce patient overpopulation in acute facilities (which can indirectly limit the quality of care patients receive) makes physiotherapists a valuable addition to a currently medical-based professional approach to managing asthma in children. The roles of the physiotherapist include:
1) Increasing awareness about the nature of the condition including pathophysiology, asthma triggers and the progression of the condition with/without effective management. Details about the condition and its progression have been outlined in the previous sections of the page however it is the physiotherapist’s responsibility to adapt the information delivered depending on the age of the child as well as parental anxiety so as to not overload with information but at the same time deliver enough useful information.
2) Delivering education to the affected child themselves, their family and their school especially in regards to participation in physical activity. Studies suggest that physical activity improves cardiopulmonary function without compromising lung function and does not have an adverse effect on wheeze for children with asthma (Ram et al. 2005). Respiratory education for the child includes secretion clearance techniques, strengthening of the respiratory muscles and specifically timed inspirations and expirations can act as exacerbation preventative therapy. Interestingly, through respiratory education, the oxygenation of the brain is enhanced which has been shown to translate into improved academic performance and improved quality of life (Valdivia 2009).
A common sign of poorly managed asthma in children is superficial/clavicular breathing. In this type of breathing, expansion of the chest only occurs around the height of the clavicles upon inspiration, the neck muscles pull the first 2 ribs in an upward direction and the diaphragm and abdomen hardly intervene. The inefficiency of this breathing pattern due to its high energy expenditure for minimal gaseous exchange makes it a perfect starting point for respiratory education to introduce lateral, deeper breathing.
3) Perform a subjective assessment including a description of the symptoms by the child and their family as well as gaining an insight into their baseline knowledge of the condition.
4) Perform an objective assessment including:
- observation of posture/work of breathing can indicate use of accessory muscles producing shallow breathing,
*palpation of neck muscles to determine extent of accessory muscle use,
*test breathlessness by assessing if the child can complete sentences in one breath,
*pulse rate measurement as tachycardia can suggest worsening asthma,
*performing auscultation and noticing the presence/absence of wheeze which can become biphasic or less apparent with increased airway obstruction,
*measuring oxygen saturation levels to determine if mobilizing or specific breathing exercises are appropriate to enhance SpO₂. (SIGN 2014)
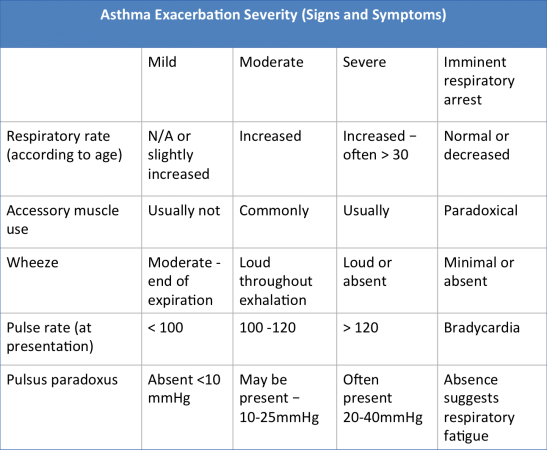
5) Management of exacerbations. Asthma exacerbations in children can be categorized depending on severity and the demonstration of specific signs. It can be useful for the physiotherapist to be informed about signs of previous exacerbations so as to monitor the progression of the child’s asthma. The table below is a useful guidance tool:
(Kumar, 2014)
6) Exercise prescription & monitoring. Studies suggests that cardiovascular endurance conditioning should be the key aspect of the physical activity a child with asthma receives (Villa et al. 2011). Respiratory exercises enhance exercise tolerance and help build resistance against muscle fatigue. Balloon blowing & cotton-wool straw football exercises are excellent examples of games which are fun for children and simultaneously increase lung volume and improve gaseous exchange to improve quality of life in a relatively controlled manner (Thomas et al. 2009).
7) Managing expectations, which refers to both the child’s expectations at the moment of the diagnosis and as they get older, but also the expectations of the child’s parents in respect to asthma progression, participation in physical activity and understanding their role in asthma management.
8) Using outcome measures to gain an insight into the progression/management of the condition. One example of an outcome measure for asthma control is the childhood asthma control test (C-ACT) for children aged between 4-12 years. One main advantage of this outcome measure is that it takes into consideration both the affected child and their caregivers.
Subjective Assessment[edit | edit source]
Symptoms[edit | edit source]
What do patients and parents know about asthma?[edit | edit source]
Objective Assessment[edit | edit source]
Auscultation[edit | edit source]
The below link includes an audio file which allows you to hear what a characteristic wheeze sounds like during the auscultation phase of an objective assessment:
en.wikipedia.org/wiki/Asthma
Pulse Oximetry[edit | edit source]
Outcome Measures[edit | edit source]
Peadiatric Asthma Quality of Life Questionnaire[edit | edit source]
Lothian Breathlessness Scale[edit | edit source]
Canadian Questionnaire (PA)[edit | edit source]
Section 4: Physiotherapy Management[edit | edit source]
Education[edit | edit source]
Correct Inhaler Use[edit | edit source]
Proper inhaler use is vital to the good management of asthma in children. It is estimated that up to 25% of asthma sufferers use improper inhaler technique (Bernstein 2014). Improper inhaler uses has proven to correlate with poor asthma control and more frequent emergency hospital visits (AL-Jahdali et al. 2013). Poor technique is also associated with a lower quality of life and level of patient education is associated with poor inhaler technique (Hashmi et al. 2012). As a result, correct inhaler technique is vital in the management of children with asthma exercising and physiotherapists should be able to properly demonstrate inhaler techniques.
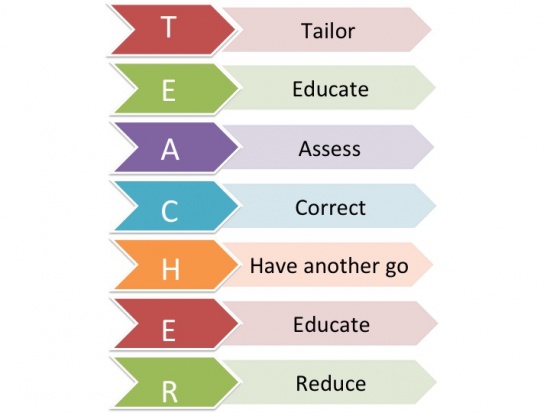
The T.E.A.C.H.E.R acronym is a great way to ensure children are in receipt of the correct care, and that their programme is tailored specifically to them. The figure below shows what the acronym stands for:
Tailor – Tailor the method of delivery to suit your patient. Many younger children especially ones younger than 5 years old have difficulty timing breathing with the inhaler and a spacer is often used to remedy this problem. Children who have shallow patterns of breathing my also find using an inhaler difficult and benefit from using a spacer
Educate - Educate the child in the correct timing of when to trigger the inhaler and how to take a deep breath. Explain to the child the importance of using the inhaler and why having correct technique is vital.
Assess – Assess the patients technique, allow them to attempt using the inhaler independently without prompts. Focus on the timing of triggering the inhaler with their breathing. Pay close attention to any mistakes.
Correct – After assessing the patients technique, correct the patient on any mistakes they may have made. Re enforce the areas in which their technique was successful and correct areas in which they need to improve.
Have Another go – Re assess the patients technique and see if it has improved after correction.
Evalute – Evaluate the childs technique and see it is of an adequate standard. If not correct and re assess again.
Reduce – Children are recommended to use their inhaler 15 minutes before physical activity and during in case of an attack. In general use a patient should be recommended to use the inhaler as conservatively as possible. Health care professionals should recommend reduction in inhaler usage if possible.
What is safe breathlessness?[edit | edit source]
Asthma Diary[edit | edit source]
Effective management of your asthma is not solely based on administering the correct medication at the correct times and dosage. This is of course one of the most important aspects in order to keep your asthma well controlled, but by no means the only option. Asthma is an extremely variable condition and no two people’s asthma is likely to be identical. This emphasises the importance of education being an integral aspect of all interactions between the health care professionals and patients, and relevant to asthma patient’s of all ages. Although the focus of education for young children will predominantly be on the caregivers and parents, children as young as 3 years old can be educated on simple asthma management skills and personal triggers. Research by (Shah et al. 2001. Trollvik et al. 2013) showed that although adolescents may have some degree of difficulty in adhering to asthma education, this could be enhanced through peer support group education with the added support of education given by the health care professional.
Management can be made easier by the application of an Asthma Diary, which can be made as simple or detailed as you require. However, the more detailed the information is the more beneficial it will be, not only for your child but also the asthma nurse or doctor, who can systematically tailor your treatment to your needs. Identification of what triggers your child’s asthma can sometimes be easily identifiable, however at times it can be complex, therefore keeping a daily asthma diary could help.
http://www.allermates.com/wp-content/themes/allermates/files/AsthmaDiary.pdf
The asthma diary (shown above) will include a record of:
• Symptoms
This would be beneficial to keep a record, so you can monitor whether your symptoms get better or worse over time. Recording the time when symptoms are worse and what triggered them would be of great benefit so measures can be undertaken to address these issues.
If you notice any of the following symptoms such as:
• Frequent waking throughout the night suffering from excessive coughing, wheezing and shortness of breath.
• Administration of the reliever treatment at a much greater rate than normal, or if this doesn’t seem to be working in any way.
• Upon wakening in the morning, you suffer from shortness of breath.
• Finding it increasingly difficult to participate in your usual level of activity.
Then the most important thing is to phone your doctor who can administer the correct treatment, which can help you bring your child’s asthma back under control.
• Peak Flow Readings
The peak expiratory flow measurements are made using a peak flow meter (PEF), which can be important in the diagnosis and monitoring of asthma. Modern PEF meters are relatively inexpensive, portable, plastic and ideal for children to use in the home setting for day-to-day objective measurements of airflow limitation.
The PEF is a measure of the highest expiratory flow that can be generated following the child’s maximal inspiration. The reading will directly be influenced by airway diameter and can be a useful indication of the degree of bronchoconstriction in asthma sufferers (Main and Dehehy. 2016).
• Medication
This is extremely important to record both the various forms of medication the child takes and also the timeframe the medication was administered. This also includes any other types of medication they use, such as over the counter remedies.
This information will allow the doctor or practice nurse to monitor how well controlled the child’s asthma is and how effective the medication is in controlling the asthma symptoms. Therefore, clinical decisions can be made whether to change, increase or decrease the medication to gain or maintain control (Ludman et al. 2016).
The asthma diary would also benefit from the recording of the child’s participation in daily activities and the effect these have on asthma symptoms. For example, the child may feel their asthma is well controlled but notice some degree of difficulty when participating in certain exercise or even running for the school bus. Recording of this information will allow your doctor or asthma nurse to generate a written self-management action plan, which is tailored to your child’s needs. According to the SIGN (2016) guidelines on the management of asthma, all patients of all ages should be offered self-management education, which should also include the development of a personalised asthma action plan. Research has shown that symptom-based written plans for children are effective in reducing emergency consultations (Bhogal et al. 2006 and Zemek et al. 2008).
Bronchodilators: The Correct Use[edit | edit source]
Self-initiated Care[edit | edit source]
Health Promotion[edit | edit source]
Recommended Physical Activity Guidelines[edit | edit source]
Children with asthma should be encouraged to lead a healthy, active lifestyle. While it is well known that healthy children should perform at least 60 minutes of physical activity a day, the same physical activity recommendations also applies to children with asthma (Longmuir et al. 2014). Adjustments or restrictions however, to the frequency, intensity, duration, or type of physical activity permitted for each child should be appropriately done so to reduce the risk of a physical activity-related adverse event (Bar-Or and Rowland 2004). Children with asthma should use inhaled β-2 agonists 15-30 minutes prior to beginning exercise (Riner and Sellhorst 2013), and do adequate warm up exercises to reduce asthmatic symptoms especially during cold weather (Asthma UK 2016).
Considerations for Children with Asthma[edit | edit source]
Quiz 3: Learning Outcome 3[edit | edit source]
Reflection: Learning Outcome 4[edit | edit source]
Conclusion[edit | edit source]
Case Study: Learning Outcome 5[edit | edit source]
Respiro Initiative, Barcelona
The Respiro Initiative is a project that began in 2008 in Barcelona<ref name="Buddy2015">Buddy (2015. Blah blah blah.</ref>. The key features of the project are outlined below:
- Physiotherapists delivered a breathing exercise program for deprived children in unfavoured economic districts with limited previous access to community physiotherapists. The breathing exercises were adapted for participants of different age groups. Children under the age of 2 were treated with respiratory physiotherapy (including percussion, vibrations, manual AD holds). Children aged between 3-10 were taught breathing games which enhance the efficient use of respiratory musculature while children over the age of 10 were assigned conscious breathing control exercises.
*Numerous exercises involving deep breathing and controlled breathing were presented to children in a fun environment and an educational component involving awareness about safe physical activity and health promotion was also included for the children and their families (Shenfield et al. 2002).
*This initiative<ref name="Buddy2015" /> can be directly replicated in other countries and has the other main advantage of tackling the poor adherence demonstrated by children with asthma towards any form of symptom management intervention due to its play-based nature.
*As highlighted above, the physiotherapists role in current management of children with asthma is to enhance community based care while incorporating health promotion. This can be done on a relatively large scale through initiatives such as Respiro or on a smaller scale such as education at local schools.
References[edit | edit source]
<references />
</div>