Patellofemoral Pain Syndrome
Original Editor - Kristin Zumo, Quentin Desantoine
Lead Editors - Your name will be added here if you are a lead editor on this page. Read more.
Search Strategy[edit | edit source]
Key words: Patellofemoral Pain Syndrome (PFPS), Patellofemoral Stress Syndrome (PFSP), miserable malalignment syndrome and Anterior Knee Pain. It’s also popularly called Runner’s Knee.
Information found at the university’s library (books and scientific journals) and websites: Pudmed, Web of Knowledge and google (scholarly articles). Quality of evidence was verified using PEDro.
Definition/Description[edit | edit source]
Patellofemoral Pain Syndrome (PFPS) is an inflammation/irritation or overuse of the patella-femoral joint capsule that can result in anterior knee pain and discomfort localized in the patellofemoral joint.
Be aware that PFPS is sometimes confused with chondromalacia patellae (which is a cartilage problem) and patellar tendonitis. Patients will (in general) complain about the same symptoms but the cause is different and so is the treatment. (See the concerning pages about these diseases for more explanation.)
Clinically Relevant Anatomy [edit | edit source]
The knee (art. Genus) consists of two major joints, the tibiofemoral joint and the patellofemoral joint. In this case, the problem will be localized in the patellofemoral joint:
The patella sits within the femoral groove; the fascies articularis patellae (posterior side) is covered with cartilage that glides over the cartilage of the anterior part of the femoral condyles (femoral groove). In this synovial joint movement and gliding creates minimal resistance due to the synovial fluid which is present around the knee and produced by the membrane synovialis, the internal part of the joint capsule during movement. Several bursae also produce synovial fluid within the capsule. The knee capsule is attached all around the patella, so only the fascies articularis patellae and femoralis are in contact with the synovial fluid. The collateral ligaments are merged with the capsule and they contributed in joint stability. On the anterior side of the patella between the patellar tendon (which is attached to the patella) and the skin, there is an extra bursa (pre-patellaris) which is normally not in contact with the knee capsule and ensures a better gliding of the patellar tendon. There is a similar bursa (infrapatellaris) at the level of the tuberositas tibiae. When the knee is inflamed, these bursae can become hyperproductive (swollen). This is possible related to increase of anterior knee pain.
Although each ligament has its own responsibility in supporting and protecting the knee, ligaments also provide assistive support to other ligaments. But the two ligaments that are most associated with PFPS are the two collateral ligaments (lateral and medial), because they are merged with knee capsule.
Epicondylopatellar and meniscopattelar ligaments form the medial and lateral retinaculum patellare part of a ligamentous complex which provides for a medial and lateral attachment of the patellar tendon at the level of the patella.
Epidemiology /Etiology[edit | edit source]
PFPS can be due to a patellar trauma, but it is more often a combination of several factors (multifactorial causes): overuse and overload of the patellofemoral joint, anatomical or biomechanical abnormalities, muscular weakness, imbalance or dysfunction. It’s more likely that PFPS is worsened and resistive to treatment because of several of these factors.
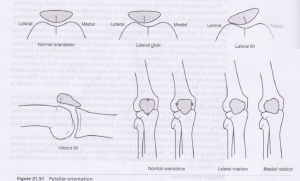
One of the main causes of PFPS is the patellar orientation and alignment. (fig.1) When the patella has a different orientation, it may glide more to one side of the facies patellaris (femur) and thus can cause overuse/overload (overpressure) on that part of the femur which can result in pain, discomfort or irritation. There are different causes that can provoke such deviations.
The patellar orientation varies from one patient to another; it can also be different from
the left to right knee in the same individual and can be a result of anatomical malalignments. A little deviation of the patella can cause muscular imbalances, biomechanical abnormalities … which can possibly result in PFPS. Conversely, muscular imbalances or biomechanical abnormality can cause a patellar deviation and also provoke PFPS. For example:
When the Vastus Medialis Obliquus isn’t strong enough, the Vastus Lateralis can exert a higher force and can cause a lateral glide, lateral tilt or lateral rotation of the patella which can cause an overuse of the lateral side of the facies patellaris and result in pain or discomfort. The opposite is possible but a medial glide, tilt or rotation is rare. Another muscle and ligament that can cause a patellar deviation is the iliotibial band or the lateral retinaculum in case there is an imbalance or weakness in one of these structures. (see table1)
PFPS can also be due to knee hyperextension, lateral tibial torsion, genu valgum or varus, increased Q-angle [1], tightness in the iliotibial band, hamstrings or gastrocnemius.
Sometimes the pain and discomfort is localized in the knee, but the source of the problem is somewhere else. A pes planus (pronation) or a Pes Cavus (supination) can provoke PFPS. Foot pronation (which is more common with PFPS) causes a compensatory internal rotation of the tibia or femur that upsets the patellofemoral mechanism. Foot supination provides less cushioning for the leg when it strikes the ground so more stress is placed on the patellofemoral mechanism. [2]
The hip kinematics can also influence the knee and provoke PFPS. A study has shown that patients with PFPS displayed weaker hip abductor muscles that were associated with an increase in hip adduction during running. [3]
Table 1
| Muscular etiologies of PFPS | |
| Etiology | Pathophysiology |
| Weakness in the quadriceps |
It may adversly affect the PF mechanism. Strengthening is often recommended. |
| Weakness in the medial quadriceps |
It allows the patella to track too far laterally. Strengthening of the VMO is often recommended. |
| Tight iliotibial band |
It places excessive lateral force on the patella and can also externally rotate the tibia, upsetting the balance of the PF mechanism. This can lead to excessive lateral tracking of the patella. |
| Tight hamstrings muscles |
It places more posterior force on the knee, causing pressure between the patella and the femur to increase. |
| Weakness of tightness in the hip muscles |
Dysfunction of the hip external rotators results in compensatory foot pronation. |
| Tight calf muscles |
It can lead to compensatory foot pronation and can increase the posterior force on the knee. |
References Table1 [4]
Characteristics/Clinical Presentation[edit | edit source]
Patient's usually present with compliant of anterior knee pain that is aggravated by activities that increase patellofemoral compressive forces such as: ascending/descending stairs, sitting with knees bent, kneeling, and squatting.
Differential Diagnosis[edit | edit source]
Different disaese can provoke anterior knee pain, without being PFPS:
- Osteoarthritis in the knee
- Chondral lesions
- medial overload syndrome
- Popliteal Cysts (Baker's cysts)
- ACL (anterior cruciate ligament) tear
Diagnostic Procedures[edit | edit source]
It is recommended that the diagnostic procedure to identify PFPS should involve first ruling out other pathologies that may cause anterior knee symptoms. [5] You can use the International Knee Documentation Committee (IKDC), which contains 18 items designed to measure symptoms associated with pain, stiffness, swelling, joint locking, and joint instability, whereas other items designed to measure knee function assess the ability to perform activities of daily living. [6][7]
Outcome Measures[edit | edit source]
add links to outcome measures here (also see Outcome Measures Database)
Lower Extremity Functional Scale (http://academic.regis.edu/clinicaleducation/pdf's/Knee_Pain_LEFS.pdf)
http://academic.regis.edu/clinicaleducation/pdf's/Knee%20Outcome%20Survey.doc
Examination[edit | edit source]
add text here related to physical examination and assessment
Medical Management
[edit | edit source]
add text here
Physical Therapy Management
[edit | edit source]
Physical Therapy (Exercises):
- Strengthening of the Quadriceps is a key in the rehabilitation program(1)
Pain-free exercises are very important when treating PFPS. Isometric exercises while the knee is fully extended (patella has no contact with condyles) can be used at the beginning of the therapy, because it minimizes stress on the patellofemoral-joint while reinforcing the M. Quadriceps (Q-ceps).
For example (exercise):
1. Straight-leg exercise
Patient (P.) lies on his back, one knee bent at +/- 90° (! pain-free if that knee is affected by PFPS) and foot flat on the ground. The other knee is fully extended. P. elevates extended leg and holds it for 10secs, before relaxing (concentric contraction and/or eccentric contraction is also possible, which makes it dynamic). Control that P. keeps a normal lumbar lordose and does not compensate with his basin.
2. Pillow squeeze exercise
P. sits comfortable with his trunk supported. Both knees extended. Place a pillow (or towel) under one knee (that knee might be slightly flexed). P. tries to push the pillow/towel in the table by extending his or her knee. (Q-ceps contraction).
Closed kinetic chain exercises (CKC) VS Open kinetic chain (OKC) exercises. (2) (3)
CKC are more functional than OKC and they provoke lower patellofemoral joint stress, particularly in the terminal ranges of full extension (0° to max 40° knee flexion). Therefore exercises should be practiced within this range and pain-free.
Example of exercise:
• Squats; be sure that the P.’s knee doesn’t come farther than his toes. Once his knee passes his toes, the stress on his patellofemoral-joint become too high and might provoke pain.
If P. is unable to tolerate CKC exercises, then OKC exercises might be a viable option because the load that will be used can be better controlled than in CKC, as long as the exercises are pain-free! When using OKC exercises, P. should stay in within a pain-free range of motion (ROM) between 40° to 90° knee flexion.
- Vastus medialis obliquus (VMO)(2)
Training of the VMO muscle can be accomplished in the beginning of the therapy, however too much focus on selective activation of the VMO muscle should be avoided. VMO-training can complement the rehabilitation program (see next topic: electrotherapy). No evidence based difference was found between general Q-ceps training and selective VMO-muscle training.
However, another study found a useful exercise to train Q-ceps, VMO and hip adductors while maintaining a correct patella tracking. (3) This exercise should be used when P. have an abnormal patella tracking, due to a disbalance between the VMO and the VL that causes a painful patella gliding;
“The double leg squat with isometric hip adduction exercise is useful in maintaining correct patella tracking and selectively strengthening VMO.” (3)
- Hip muscles training (4)(5)(6)
Rehabilitation program for PFPS should also incorporate strengthening exercises of the hip abductors and lateral rotators. It has been proven that the pain during daily activities was lower and functionality was greater when knee exercises are combined with hip exercises. (Table 1 and 2 + figure 2 show which exercises were used in the research and proved to be efficient. Exercises were performed during 4 weeks)
Another research study found that PFPS patients had decreased eccentric hip abduction compared with healthy people. Thus, it is recommended to use eccentric hip abduction strengthening exercises. (5)
- Proprioceptive training(7)(8)
It has been proven that the proprioceptive quality in the knee of patients with PFPS is decreased. Even with unilateral PFPS, the proprioception is decreased in both knees (pathologic and non-pathologic knee)! Therefore proprioceptive training (pain-free exercises!) of the knee should be part of the rehabilitation program.
Electrotherapy (9)
Some patients might suffer from PFPS because of a (neuromuscular) disbalance between the VMO and VL. The main cause is muscle atrophy of the VMO and excessive/abnormal lateral tracking of the patella, due to the remaining force of the VL. In case of neuromuscular disbalance between the VMO and VL, electrical stimulation of the VMO should be considered to complement the conservative (exercises) therapy, because it is selective and does not stress the patellofermoral joint.
An example of how you can accomplish the stimulation;
The patient sits with the trunk supported extended legs with slight knee flexion and lower limb muscles completely relaxed. Following parameters were used in research (isometric contraction of the VMO): (9)
- Electrode placing = 1 on the motor point and the other one next to it.
- Asymmetric bipolar current
- Pulse width = 0.5 milliseconds
- Pulse frequency = 50Hz
- Intensity = max. the patient can endure without pain
- Time = 7 minutes => 6 repetitions, on for 6seconds and off for twelve, and progressed to 30 minutes, 11 repetitions, on for 10sec and off for 12sec.
Evaluation;
You can use EMG feedback to capture EMG activity of the VMO and VL before and after the therapy. While your patient is performing the functional test of stair stepping using the limb affected by PFPS; patient faces the stairs in standing position. He begins the movement by flexing the limb with PFPS, placing it on the first step, and then extends it in unilateral stance. In a continuous movement, he places the non-affected limb on the second step and finishing the stair stepping with full knee extension. (9)
Be aware that stepping upon a stair can be very painful for PFPS patients. Only use this evaluation technique once the P. can perform this test pain-free. Start with a very low stair, so the P. doesn’t have to flex too much his knee, which mean there is lesser compression between the patella and the femur => it’s less pain provocativeis minimal.
The main differences you should find are increased energy consumed by the VMO muscle in order to perform the test. → Change in force-generating capacity of the muscle.
And faster (more accurate) activation of the VMO muscle after therapy.
Foot orthoses (10)(11)(12):
There are a few clinical predictors that can help decide if a P. is more likely to benefit from foot orthoses or not;
- Individuals with PFPS who wear less supportive footwear,
- those who report lower levels of pain,
- exhibit less ankle dorsiflexion range of motion,
- P. who reports an immediate reduction in pain with foot orthoses when performing a single-leg squat.
What kind of orthoses? In research prefabricated orthoses were used; made of ethylene-vinyl acetate of medium density (Shore A 55), containing built-in arch supports and 4-varus rearfoot wedging.(11)(12)
Prefabricated foot orthoses significantly enhanced functional performance in individuals with PFPS after 12 weeks, and these improvements were greater than those observed immediately after the foot orthoses were used. These improvements may be important to long term prognosis and prevention of osteoarthritis development for some individuals with PFPS (further research is needed). (12)
Kristin Zumo:
Common interventions for the treatment of PFPS are listed below:
- Manual Therapy
- Exercise (open vs. closed chain)
- Quadriceps strengthening
- Patellar Taping
- Orthotics
- Proximal Muscle strengthening
- Modalities
What treatments LACK support by current evidence?
- No significant difference was noted in open vs. closed chain exercises with respect to exercise type.
- Further evidence is needed to investigate the long term effects of patella taping, the mechanism of action and direction of force (medial, neutral, lateral). Clinical evidence for the success of this intervention is still unclear due to an insufficient amount of high level evidence, inconsistency of tape application techniques, in ability to identify the precise mechanism of aciton, and variance in measurements of specific outcome variables.
- No date is available regarding massage, thermotherapy, TENS, electrical stimulation, and biofeedback for treatment of PFPS.
What treatments are SUPPORTED by the best available evidence?
- Tyler et al noted the role of hip muscle function in the treatment of PFPS. A 93% success rate occurred with hip flexor strenght improvements and normalization of Ober (IT band/tensor fascia latae) and Thomas (hip flexor) tests.
- A case report by Mascal et al documented weakness of hip abductors, extensors and external rotators in testing of 2 patients with PFPS. Treatment consisted of recruitment and endurance training of the hip, pelvis, and trunk musculature which resulted in a significant reduction in pain, improved LS kinematics during dynamic testing and ability to return to original level of function.
- Whittingham et al investigated the effectiveness of daily patella taping and exercise on pain and function in individuals with PFPS. Results suggest that patella taping may be useful in conjunction with strengthening exercise to enhance speed of recovery.
- 2 articles were reviewed in regards to the effect of foot orthoses on PFPS. Both studies suggest that the use of orthotics in patient's who present with excessive pronation resulted in improved pain/stiffness (note: multiple interventions were used in these studies, including orthosis). Patients with patellofemoral pain may benefit from the use of foot orthosis if the patient demonstrates the following: excessive foot pronation and/or a LE alignment profile that includes excessive lower extremity internal rotation during weight bearing and increased Q-angle. Additional studies are needed to assess the treatment efficacy of foot orthosis for patients with PFPS.
Take Home Message:Focus on identifying the root cause of the problem and always consider proximal and distal influences (regional interdependence). Based on the available evidence, exercise and manual therapy seem to be the most benefical in the managment of anterior knee pain. Addressing the strength and ROM deficits at the hip and pelvis has also shown to be effective in management of anterior knee pain.
Key Research[edit | edit source]
add links and reviews of high quality evidence here (case studies should be added on new pages using the case study template)
Resources
[edit | edit source]
Sites (RCT & evidence based):
The reliability and validity of assessing medio-lateral patellar position: a systematic review
http://www.sciencedirect.com.ezproxy.vub.ac.be:2048/science?_ob=ArticleURL&_udi=B6WN0-4TJ5YXG-3&_user=1011600&_coverDate=08%2F31%2F2009&_rdoc=1&_fmt=high&_orig=search&_origin=search&_sort=d&_docanchor=&view=c&_acct=C000050280&_version=1&_urlVersion=0&_userid=1011600&md5=444b59b90cf1cfc988098c64798b12f0&searchtype=a
patellofemoral pain syndrome a review and guidelines for treatment
http://www.hhfamilymedicine.com/hhfm/Orthopedics_files/Patellofemoral%20Pain%20Syndrome_%20A%20Review%20and%20Guidelines%20for%20Treatment%20-%20November%201,%201999%20-%20American%20Academy%20of%20Family%20Physicians.pdf
Books:
SANDRA J. SHULTZ – PEGGY A. HOUGLUM – DAVID H PERRIN – 2005 – Examination of musculoskeletal injuries (second edition) – Human Kinetics -17: 450, 470
PEGGY A. HOUGLUM – 2005 – Therapeutic Exercise for musculoskeletal injuries (second edition) – Human Kinetic – 21: 820-827; 871-879
D.L. EGMOND – R. SCHUTIMALS – 2006 – Extremiteiten: manuele therapie in enge en ruime zin – Bohn Safleu van Loghum – 11: 559-630
Anatomical Atlas (Promoteus) used as support.
Clinical Bottom Line[edit | edit source]
add text here
Recent Related Research (from Pubmed)[edit | edit source]
Failed to load RSS feed from http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1dq9VTyhitMWEiG-CS5f4g76sfbDmOa7_01R9pi6_7388h2ggk|charset=UTF-8|short|max=10: Error parsing XML for RSS
References[edit | edit source]
References will automatically be added here, see adding references tutorial.
- ↑ http://www.sciencedirect.com.ezproxy.vub.ac.be:2048/science?_ob=ArticleURL&_udi=B6T6F-4X24C13-1&_user=1011600&_coverDate=07%2F31%2F2010&_rdoc=1&_fmt=high&_orig=search&_origin=search&_sort=d&_docanchor=&view=c&_acct=C000050280&_version=1&_urlVersion=0&_userid=1011600&md5=9202d70cd66537e025ee264bc77cb8e3&searchtype=a
- ↑ http://www.jospt.org.ezproxy.vub.ac.be:2048/issues/articleID.2427,type.2/article_detail.asp
- ↑ http://www.jospt.org.ezproxy.vub.ac.be:2048/issues/articleID.1411,type.2/article_detail.asp
- ↑ http://www.hhfamilymedicine.com/hhfm/Orthopedics_files/Patellofemoral%20Pain%20Syndrome_%20A%20Review%20and%20Guidelines%20for%20Treatment%20-%20November%201,%201999%20-%20American%20Academy%20of%20Family%20Physicians.pdf
- ↑ http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2841549/?tool=pubmed
- ↑ http://www.ncbi.nlm.nih.gov/pubmed/17888709
- ↑ http://ajs.sagepub.com/content/34/1/128.abstract