Patellar Fractures
This injury article requires improvement to meet Physiopedia's quality standards. The reasons have been specified below this alert box. Please help improve this page if you can. #qualityalert #qualityalert_injury
To edit: general formatting, completion of categories
Editors ---Marie Avau 09:32, 15 September 2015 (BST)Marie Avau ,Debby Decock ,Ellen Vandyck,Tamara Kindekens
Search Strategy
[edit | edit source]
We initiated our search about ‘patellar fractures’ by putting words like patella, fracture, symptoms and diagnosis in PubMed. Secondly we went to the library to borrow books about this topic, for example: ‘practical fracture treatment’ and ‘Algemene Anatomie en bewegingsapparaat’. After this search, some parts were still incomplete so we consulted scientific databases like Pedro, Medscape, Springer Link etc.. using keywords and combi-nations of keywords like: patella, patellar fracture, fractures in the knee, treatment and care of patellar fractures, etiology of patellar fractures, diagnosis of patellar fractures and especially physical therapy treatment of a patellar fracture, to complete everything.
Definition/Description[edit | edit source]
Patellar fracture is a very common knee injury. They can be divided into three types.
The first type is caused by direct violence and is called comminuted (this is a bone fracture that results in more than 2 separate bone components, the bone breaks into several pieces). These type of fractures are usually associated with a blow or a fall on a flexed knee.
The second type is caused by muscle violence and is called transverse. These type of frac-tures are usually associated with rupture of structures at the lateral site of the knee such as the collateral ligament.
Finally, the third type is a minor marginal fracture, which is usually caused by a fall on the knee. [10]
Approximately 1% of all skeletal injuries are patellar fractures. [1][2]
Thereby, fractures may be accompanied by a sprain or rupture of the ligaments or tendons that are attached to the patella. This injury can lead to stiffness, extension weakness, and patellofemoral arthritis.[11]
Clinically Relevant Anatomy[edit | edit source]
The patella is the largest sesamoïd bone in the body.
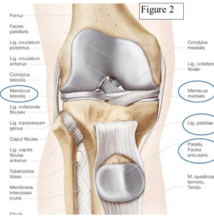
The patella is a triangular bone that is situated on the anterior surface of the knee at the distal end of the femur, it's a part of the articulatio patello-femoralis. In combination with the capsuloligamentar ligaments and the meniscus medialis and lateralis it forms the knee joint. .[17,13]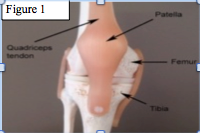
 On the anterior side of the patella we can find: facies anterior, basis patellae and apex patellae. On
On the anterior side of the patella we can find: facies anterior, basis patellae and apex patellae. On
the posterior side of the patella we have: facies articularis patellae, one lateral and one me-dial separated by a ridge. On The basis patellae is the insertion of the quadriceps tendon and the apex patellae is the origin of the patellar ligament. The patella has the thickest articular cartilage of the body, it may be as thick as 1 cm. The patella is surrounded by several structures going from muscles to menisci. The two muscles that control the move-ment of the patella are the vastus medialis and the vastus lateralis. [5]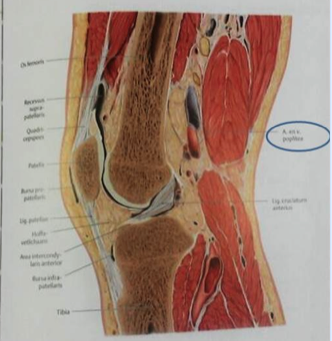
The blood supply in the patella is derived from two vessel systems, branched out of the geniculate arteries. Together, they supply the middle third and the apex of the patella. .[16,17]
Epidemiology /Etiology[edit | edit source]
Because of its subcutaneous location, the patella is very vulnerable to injury. Patellar frac-tures occur as a result of a compressive force, a sudden tensile force (as occurs with hyper flexion of the knee), or a combination of these two causes. [16,17,13]
These fractures can be caused by direct blows to the knee in sports injuries or accidents, or from indirect stresses caused by twisting actions or violent contractions in the muscles sur-rounding the knee.[10,12]
As a result of these forces, various fracture patterns result, which depend on the mechanism of the injury.
The most common pattern is often described as transverse or stellate. (in this case the prox-imal blood supply may be compromised leading to avascular necrosis of the proximal seg-ment.)[14,16]
Less common patterns include vertical, marginal, osteochondral, and sleeve fractures (exclu-sively seen in the pediatric population).
Causes of fractures:
A direct blow to the patella: most often results in a stellate fracture. The compressive forces applied to the patella result in a comminuted pattern. The energy of the blow is absorbed by the fracture and causes damage to the articular cartilage of both the patella and the femoral condyles.
Another mechanism is a tensile force: this is sustained with hyper flexion of the knee, this is equal to an eccentric contraction of the quadriceps.
A combination of these two mechanisms: leads to a variety of other fracture patterns. A dis-placed transverse fracture can have “comminution”(see figure 3).[16,17,13
Characteristics/Clinical Presentation[edit | edit source]
Patellar fractures are classified in two groups: displaced or non-displaced, these 2 groups consist of several types.
Non- displaced fractures can be recognized when the broken bone is stable and has re-mained in place.
Displaced fractures, in which the pieces of broken bone have shifted out of position, logically these fractures are unstable.(transverse, vertical, comminuted or lower/upper pole)[10,15]
Differential Diagnosis[edit | edit source]
A doctor can diagnose a fracture of the patella by asking you about the details of your acci-dent and by examining you. He will inspect your knee, focusing on where it is tender, swol-len or misshapen. Then, he may also ask you to raise your leg or extend your knee, possibly after giving you a local anesthetic to eliminate pain. This helps the doctor to see if there are other injuries in and around your knee. [24]
Most of the times the individual reports pain during this examination of the affected knee.
Common causes that the patients may report for this pain are: an accident, a fall from height or a direct blow to the knee.[10]
The best way to exclude or include a patellar fracture is an X-ray, taken from several angles, to determine the extent of a fractured kneecap and to check for other injuries. If other inju-ries are suspected, a computer tomography (CT) or magnetic resonance imaging (MRI) scan may also be done. [24]
Diagnostic Procedures[edit | edit source]
A patellar fracture is suspected when there is a history of direct violence, when there are difficulties in standing or when there is a snapping sensation. In most cases there is straight leg raise inability and the inability to extend the knee.
Bruising and abrasion, the presence and site of tenderness, any palpable gap above or be-neath the patella as well as any obvious proximal displacement of the patella can indicate a patellar fracture.
Radiographs are necessary to clarify because there isn't some kind of specific test to identify a patellar fracture. Standard x-rays with special views of the patella are usually sufficient to diagnose a patellar fracture. However in more difficult cases where x-rays are not decisive, CT scan may be necessary. Associated injuries to nearby tendons and ligaments may need to be evaluated by MRI studies.[18,21,22,13]
Outcome Measures[edit | edit source]
The outcome depends primarily on the quality of articular restoration. Any intra-articular incongruities lead to the development of posttraumatic arthritis.
The prognosis of the injury depends on the amount of chondral damage at the time of injury. Functional outcome depends on the ability to achieve pain-free and stabile range of motion in an early stage.
Manipulation under anesthesia or the arthroscopic releasing of adhesions is required when athrofibrosis occurs.
Future treatment options may include osteochondral allograft reconstructions of the patella, for posttraumatic arthritis. Currently, several fixation methods of patellar fractures includes modified tension band wiring, Circumferential cerculage wires, and screw fixation and re-cently bioabsorbable fixation which may reduce the frequency of hardware symptoms.[18]
Examination[edit | edit source]
The clinical examination should include an inspection of the whole extremity. Clinical signs of a patellar fracture are swelling and pain in the knee joint. Wounds should be checked to con-firm whether the fracture is open or closed.
In displaced patellar fractures, a defect zone between the fragments may be palpable. Often there is a haemarthrosis of the knee. Flexion and extension in the knee joint is limited and painful. Active extension and lifting of the leg is usually impossible.
However, the ability to extend the knee does not rule out a patellar fracture, because the medial and lateral retinacula may be still intact.
Of course a check of the peripheral pulses, the compartments of the leg, and a neurological examination should always be performed. Special interest should be paid to potential ipsi-lateral concomitant injuries (e.g. acetabular fractures, femoral fractures or tibial fractures) which are signs of serious trauma.[19]
Medical Management
[edit | edit source]
Surgical treatment is usually performed in patients with a displaced fracture and is carried out on an emergency basis if the fracture is open or if an associated traumatic arthrotomy is present.Sometimes surgery is necessary because the strong M. Quadriceps can pull the broken pieces out of place and apart from each other so callus cannot form. When this occurs, healing with ossification is im-possible.
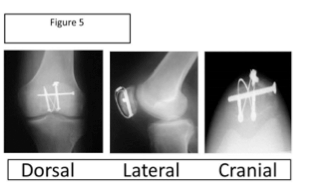
The therapy procedure variates with the characteristics of the patella fracture. If you have a transverse fracture If the fracture is transverse, the most common procedure is to use pins and wires and 'a figure of eight' to press the pieces together (AO tension band wiring). A comminuted fracture is usually associated with a blow or a fall on a flexed knee, and causes the patella to break in several pieces. In this case, the small crushed pieces of the patella will be re-moved.(partial patellectomy). In addition, there is also a procedure called ‘complete pallac-tomy’. In this case the whole patella is removed and the tendon of the M. Quadriceps is at-tached to the ligamentum patellae, to ensure the function of the extensor apparatus. But, this is a relatively old procedure and its effects are controversial. (Günal L. et al ) [24]
A break in the center of the kneecap can be fixed using wires and screws. Note that a patellec-tomy is the last treatment for a comminuted fracture.
Operative treatment aims to restore extensor function, align articular incongruities, and al-low early motion (Fourati M.K. Level 2b: levels of evidence, Mehling, I. et al, Scolaro, J. et al. level of evidence 5, Zhongguo Gu Shang et al. level 2b: levels of evidence, Strauss J. MD Lev-el 5 :levels of evidence) [22, 18, 19,20, 25]
Nonsurgical treatment (Orthopeadic) is indicated when the broken pieces of the patella aren't displaced. The patient needs a casts or splints to immobilize the fractured pieces, this is done in vertical and horizontal fractures. In horizontal fractures, radiographs are taken at weekly intervals to exclude late separation of the pieces. so callus formation can take place. In this way the callus can form. Crutches will be used during the 6 to 8 week healing process.[7][8]
Once radiographic evidence indicates union and clinical signs of healing (nontender to palpa-tion) are present, the patient is changed to a removable brace.( Mehling, I. et al )[18]
Physical Therapy Management
[edit | edit source]
Treatment with cold can be used to control pain and oedema. During the immobilization of the knee the patient is encouraged to train other leg muscles. After removing the cast or splint, and the fracture is considered healed, the therapy to regain range of motion starts.
There are instructions to prevent loss of motion and strength in adjacent joints. Ankle exer-cises are taught to promote circulation.
The range of motion, strengthening, and proprioceptive exercises of the involved joint should be initiated and progressed as indicated and tolerated by the individual. [9]
Treatment procedure Post-Operative :
Phase
I:
0-2
Weeks
Knee
Immobilizer:
Worn
at
all
times
(taken
off
only
for
physical
therapy
sessions
converted
to
hinged
knee)
brace is worn
at
first
post‐op
visit
- Weight bearing: with the knee locked in extension
- Range of Motion: 0‐30 degrees
- Therapeutic Exercises:
•
Isometric
quadriceps/hamstring/adductor/abductor
strengthening,
• Ankle
theraband exercises
Phase
II:
2-6
Weeks
Knee
Brace:
Worn
with
weight bearing
activities
still
locked
in
full
extension,
may
be
removed
at
night
- Weightbearing:
- Range of Motion: add 15 degrees of flexion each week –
- Goal is 90 degrees by post‐op week 6
- Therapeutic Exercises:
• Isometric
quadriceps/hamstring/adductor/abductor
strengthening,
• Ankle
theraband
exercises,
• Initiate
straight
leg
raises
Phase
III:
6-10
Weeks
Knee
Brace:
Unlocked,
worn
with
weight bearing
activities
- Weightbearing: Full
- Range of Motion: progress to full ROM by post‐operative week 10
- Therapeutic Exercises: Isometric quadriceps/hamstring/adductor/abductor strengthening, Ankle theraband exercises, Initiate straight leg raises
Phase
IV:
10-12
Weeks
Knee
Brace:
Discontinue
- Weightbearing: Full
- Range of Motion: Full
- Therapeutic Exercises: Isometric quadriceps/hamstring/adductor/abductor strengthening, Ankle theraband exercises, Initiate straight leg raises, Start stationary bicycle
Phase
V:
36
Months: return
to
full
activities
as
tolerated
(Strauss J. (MD)(level of evidence : 5), Elizabeth Arendt(MD) ( level of evidence: 5) )
Treatment procedure Non-Operative :
Phase
I:
0-6
Weeks
• Knee
Brace:
Brace locked in extension 2-3 weeks, controlled motion brace at 2-3 weeks
o Weightbearing:
• PWB in brace and on crutches.
• May stand tandem.
• Duration of crutches as per surgeon
o Range
of
Motion:
ROM as per surgeon
o Therapeutic
Exercises:
• Start open kinetic chain strengthening and ROM of knee at 3-4 weeks or per surgeon order.
• Quadriceps
• Hamstring
• Glutei sets
• SLR
Open and close kinetic chains hip strengthening exercises.
• Patellar mobilization
Examples of a knee braces after a patellar fracture:
Open kinetic chain strengthening and ROM of knee:
Phase II: 6-12 Weeks
• Knee Brace: Discharge per surgeon order
o Range of Motion: Progress toward full knee flexion, extension
o Therapeutic Exercises:
▪ Stationary biking with seat elevated and no resistance for ROM
▪ Progress close kinetic chain exercise: mini squats, step up, retro step, etc
▪ Progress resistance on hip exercise.
▪ Advance proprioceptive exercise
▪ Begin lunges 8-10 weeks
(Strauss J. (MD)(level of evidence : 5), Elizabeth Arendt(MD) ( level of evidence: 5), Kathryn E. Cramer, MD et al (level of evidence 5 )
Examples of exercices:
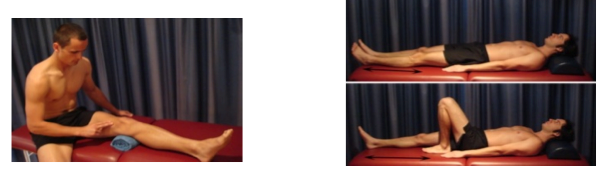
Quadriceps: The patient sits on the floor with his injured leg straight and his other leg bent. He presses the back of the knee of his injured leg against the floor by tightening the muscles on the top of his thigh. He has to hold this position 10 seconds and then re-lax, the patient does 2 sets of 15seconds. (Bhave A et al. (Level of evidence :5), Creighton AR et al. (level of evidence : 5))
SLR : The patient has to lie on his back with his legs straight. Then he has to bend the knee on his uninjured side and place his foot flat on the floor. Once this is done, he has to tighten the thigh muscle on his injured side and lift his leg about 8 inches off the floor. The patient keeps his leg straight and his thigh muscle tight and then he brings his leg slowly back down to the floor. This exercise is also done in 2 sets of 15 seconds. Bhave A et al. (Level of evidence :5), Creighton AR et al. (level of evidence : 5)
Patellar mobilisation :
o Patient sits with his injured leg in front of him. His leg should be completely straight and relaxed. Patient has to use his hands to move the patella sideways toward the inside of his leg. Then he has to move it sideways toward the inside of his leg. Each position has to be hold for 15 to 30 seconds.
Fourati M.K. (level of evidence:2b), Elizabeth Arendt(MD) (level of evidence: 5),Bhave A et al. (Level of evidence :5), Creighton AR et al. (level of evidence : 5)
o Patient has to use his hands to move his patella toward him and then away from him for 15 to 30 seconds in each direction. Then he has to compare the movement of the injur
ed patellla with the movement of the uninjured patella. The main goal is to have the same amount of movement for bouth kneekaps. [22,26,27,28]
Key Research[edit | edit source]
Key words:
- Patella
- Fracture
- Lower extremity
- Revalidation of the knee
- Treatment of patellar fractures
- Symptoms
- Diagnosis of patellar fracture
Resources
[edit | edit source]
http://www.physioroom.com/injuries/knee/patella_fracture_full.php
http://www.summitmedicalgroup.com/library/adult_health/smapatellarfractureexecises_references/
http://www.mdguidelines.com/fracture-patella
http://www.ncbi.nlm.nih.gov/pubmed/?term=patellar%20fracture
http://www.healthline.com/human-body-maps/knee
Recent Related Research (from Pubmed)
[edit | edit source]
New technique to treat a patellar fracture: El-Sayed and Ragab reported on arthroscopic-assisted reduction and fixation of displaced transverse fractures of the patella in 14 patients with displaced transverse fractures of the patella. Patients were treated by means of arthro-scopic-assisted closed reduction of the fracture with percutaneous screw fixation. Patella fractures were found to unite in a mean of 7 weeks. All 14 patients regained full extension of the knee, and full range of motion was achieved in 12 patients, with 2 patients experiencing a 10º loss of flexion. [29]
References
[edit | edit source]
1. M A A CROWTHER, A MANDAL, P P SARANGI, Propagation of stress fracture of the patella, Br J Sports Med, 2005;39
2. RODNEY SWEETNAM, Patellectomy, Postgrad Med J, 1964
3. expertorthopaedics, http://www.expertorthopaedics.com/surgery.html (accessed December 26, 2010)
4. Charles D. Newton,Textbook of small animal orthopaedics, fractures of small bones, chapter 33, http://cal.vet.upenn.edu/projects/saortho/index.html (accessed Decem-ber 26, 2010)
5. Orthopaedia, Collaborative Orthopaedic Knowledgebase, http://www.orthopaedia.com/display/Main/Patella+fractures (accessed November 10, 2010)
6. UGUR HAKLAR, BARIS KOCAOGLU, AREL GERELI, UFUK NALBANTOGLU, OSMAN GUVEN, Arthroscopic inspection after the surgical treatment of patella fractures, April 15, 2008
7. Duke Orthopaedics, Wheeless’ textbook of Orthopaedics, http://www.wheelessonline.com/ortho/fractures_of_the_patella (accessed Novem-ber 10, 2010)
8. AAOS, American Academy Of Orthopaedic Surgeons, http://orthoinfo.aaos.org/topic.cfm?topic=A00523 (accessed November 10, 2010)
9. Medical Disability Guidelines , http://www.mdguidelines.com/fracture-patella (ac-cessed December 26, 2010)
10. Melvin JS. Et al, “patellar fractures in adults”, The journal of the American academy of orthopaedic surgeons, 2011. ( level of evidence 3B)
11. Insall, “ Fractured kneecap: treatments”, Institute for Orthopaedics and sports medi-cine, 2007. (level of evidence 5)
12. Archdeacon, Michael T., and Roy W. Sanders. "Chapter 54 - Patella Fractures and Extensor Mechanism Injuries." Skeletal Trauma. Eds. Bruce D. Browner, et al. 4th ed. W.B. Saunders, 2008.
13. Everett, Lyn, et al. "Knee and Lower Leg." Rosen's Emergency Medicine: Concepts and Clinical Practice. Eds. J. A. Marx, et al. 6th ed. Philadelphia: Mosby Elsevier, 2006.
14. Lamoureux, Christine. "Patellar Fractures." eMedicine. Eds. David S. Levey, et al. 24 May. 2007. Medscape. 23 Dec. 2009 <http://emedicine.medscape.com/article/394270-overview>.
15. Whittle, Paige A. "Fractures of the Lower Extremity." Campbell's Operative Ortho-paedics. Eds. S. Terry Canale and James H. Beaty. 11th ed. Philadelphia: Mosby Else-vier, 2008.
16. Gary Shankman, OPA-C, PTA, ATC, CSCS, CWS, “Treating Patella Fracture”, Advanced health care network for physical therapy and rehab medicine, 1999. (level of evi-dence 5)
17. Schunke M. et al, Anatomische atlas Prometheus, algemene anatomie en bewegingsapparaat, Bohn Stafieu van Loghum, 2e druk (juli 2010), p. 390-401
18. Mehling, I. et al, « Comminuted patellar fractures », Current Orthopaedics, volume 20 p.397-404, 2006.
19. Scolaro, J. et al, « In brief : patellar fracture », For the association of bone and joint surgeons, 2010. (level of evidence 5)
20. Zhongguo Gu Shang et al, “patellar fractures treatment and management”, Unbound medline 2013 Jun;26(6):445-8. (level 2b: levels of evidence)
21. McRae et al, “Practical fracture treatment” , Churchill Livingstone/ Elsevier, Editie 2002. (level 2a: levels of evidence)
22. Fourati M.K., "reeducation du genou après fracture de la rotule", Ann. Kinésitherapie, 1986. (Level 2b: levels of evidence)
23. Cedars-Sinai, Fractured Kneecap, Cedars Sinai organisation, 2014.
24. Günal L. et al, Patellectomy : an overview with reconstructive procedures, Clinical Orthopeadics and Related Research, 2001.
25. Strauss J. (MD), ORIF Patella Fracture Post-Operative Rehabilitation Protocol, Hospi-tal for Joint Diseases, 2008 (Level 5 :levels of evidence)
26. Elizabeth Arendt(MD), Non-Operative Patellar Fracture: rehabilitation Protocol, Uni-versity of Minnesota: department of Orthopaedic Surgery. (Level 5 :levels of evi-dence)
27. Bhave A, Baker E. Prescribing quality patellofemoral rehabilitation before advocating operative care. Orthop Clin North Am. 2008 Jul;39(3):275-85. (level of evidence :5)
28. Creighton AR, Bach BR Jr. Arthrofibrosis: Evaluation, Prevention, and Treatment. Techniques in Knee Surgery. June 2012; 11(2):91–98. (level of evidence :5)
29. El-Sayed AM, Ragab RK.,‘Arthroscopic-assisted reduction and stabilization of trans-verse fractures of the patella.’, The Knee, Volume 16, Issue 1, Pages 54–57, January 2009. (level of evidence 1B)
30. Kathryn E. Cramer, MD et al, Patellar Fractures: Contemporary Approach to Treatment, J Am Acad Orthop Surg 1997;5:323-331 (level of evidence: 5)