Patella alta: Difference between revisions
Neil De Bie (talk | contribs) No edit summary |
Neil De Bie (talk | contribs) No edit summary |
||
| Line 36: | Line 36: | ||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
It is not easy to diagnose patella alta. It is difficult to evaluate the correct height as well as the position of the patella in relation to the deeper knee structures. Just by looking and touching it is quite impossible to diagnose patella alta, this is why an x-ray is recommended. <br><br>A person that has a patella alta may feel instability in the knee. Patients normally have a swollen knee that is filled with water; this place where the water is localized in the knee may look like a bulging portion just like a camel back.<br><br>For confirmation, a lateral X-Ray is made with the knee bent at 90 degrees. This will confirm the patella alta, by measuring its height<ref>Bohn Stafleu van Loghum (Level of evidence: D)</ref><br> | |||
== Outcome Measures == | == Outcome Measures == | ||
Revision as of 20:01, 16 January 2017
Original Editors - Fitim Cami
Top Contributors - Neil De Bie, Fitim Cami, Laura Ritchie, Joris De Pot, Admin, Kim Jackson, Simisola Ajeyalemi, WikiSysop and Naomi O'Reilly
Search Strategy[edit | edit source]
The following databases have been used to find information about "Patella alta": Pubmed, Medscape, Google scholar, Pedro, Online database of the VUB
Words that have been used: Patella alta, Conservative treatment AND patella alta, Patella alta AND physical therapy, Patellar dislocation & Etiology
Definition/Description[edit | edit source]
Patella alta or high-riding patella refers to an abnormally high patella in relation to the femur. The patella sits high on the femur where the groove is very shallow. Here the sides of the femoral groove provide only a small barrier to keep the high-riding patella in place. A strong contraction of the quadriceps muscle can easily pull the patella over the edge and out of the groove, leading to a patellar dislocation. This condition has been associated clinically with patellofemoral dysfunction and is considered a predisposing factor for the development of patellofemoral pain (PFP). Patella alta is also characterized as instability of the Patella[1][2][3]
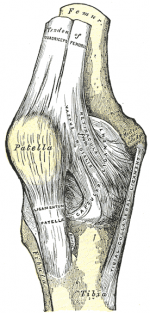
Clinically Relevant Anatomy [4] [5][edit | edit source]
The knee joint consists of three bones, the femur, the tibia, the fibula and also the patella which is a sesamoid.
The patellofemoral joint is the portion of the knee joint between the patella and the femoral condyles. The patellofemoral articulation totally depends on the function of the quadriceps. The quadriceps muscles are connected to the patella with a shared tendon. The quadriceps femoris is divided into four different muscles with the same insertion on the patella: the rectus femoris (RF), the vastus lateralis (VL), the vastus intermedius (VI) and the vastus medialis (VM). There is also a tendon that connects the bottom of the patella to the tibia, called the patellar tendon. This tendon is extremely strong and allows the quadriceps muscle group to straighten the leg.
The knee joint is one of the largest and most complex joints in the body. It is constructed by 4 bones and an extensive network of ligaments and muscles.[11]
The thigh bone (Femur), the shin bone (Tibia) and the kneecap (Patella) articulate through tibiofemoral and patellofemoral joints. These three bones are covered in articular cartilage which is an extremely hard, smooth substance designed to decrease the friction forces. The patella lies in an indentation of the femur known as the intercondylar groove.[11]
The smaller shin bone that runs alongside the tibia (Fibula) and is attached via the superior tibiofibular joint is not directly involved in the knee joint, but provides a surface for important muscles and ligaments to attach to.[12][11]
The distal aspect of the femur forms the proximal articulating surface for the knee, which is composed of 2 large condyles. The medial and the lateral. These two condyles are separated inferiorly by the intercondylar notch although they are connected anteriorly by a small shallow groove which is known as either the femoral sulcus or the patella groove or patella surface. This engages the patella in early flexion.
The tibia (shin bone) also has 2 asymmetrical condyles (medial and lateral) of which are relatively flat, These are also known as the tibial plateau. The medial tibial plateau is much longer than the lateral anteroposteriorly, and the diameter of the proximal tibia is much greater than the shaft posteriorly which is sloped at approximately 7 to 10 degrees to facilitate flexion of the femoral condyles on the tibia.
The two tibial condyles are separated by the intercondylar tubercles, these are two boney spines which are roughened and their role lies within knee extension. They become lodged in the intercondylar notch of the femur, adding to the stability of the joint. Overall the tibiofemoral joint is a relatively unstable joint as the plateau's are slightly convex anteriorly and posteriorly. This emphasises the importance of the other structures of the knee such as the menisci.
Etiology[edit | edit source]
Patella Alta can occur as the result of a sports injury, though the large majority of the time it is a congenital/developmental condition that is unrelated to trauma. Its pathophysiology is not completely clear, but it is hypothesized that one of the causes of Patella Alta, are abnormally long patellar tendons (>52 mm). [6] [7]
The Multicenter Osteoarthritis (MOST) Study made in 2010 is a prospective cohort study of 3,026 individuals, aged 50 to 79 years, who either have or are at high risk of knee OA. Subjects were recruited from 2 communities in the United States: Birmingham, Alabama and Iowa City, Iowa. In the present study, we used a sample of 907 knees, one knee per subject, randomly selected from knees which underwent MRI at baseline and 30 months and whose MRIs were read for structural abnormalities as part of other completed studies. In all subjects, lateral radiographs were acquired at baseline. The institutional review boards at the University of Iowa, University of Alabama, Birmingham, University of California, San Francisco, and Boston University School of Medicine approved the study protocol.
For patella alta the ISR and ModISR were measured from the baseline lateral semi-flexed weight bearing radiograph (Figure 1). We used the weight bearing lateral radiograph as opposed to sagittal MRI because the patellar position can change with knee flexion. This procedure was standardized across all patients and study sites and yielded knee flexion angles of 20-50 degrees (median 39 degrees). All measurements were made using Osirix digital software (Version 3.2.2). The ISR was calculated by dividing the distance from the tibial tuberosity to the inferior pole of the patella by the length of the patella from the apex of the patella to the most posterior superior point. The ModISR was calculated by dividing the distance from the tibial tuberosity to the inferior margin of the articular surface of the patella by the length of the articular surface of the patella. We additionally calculated a ratio between the length of the patellar tendon and the subjects' height (LTH). The findings indicated that patella alta, measured by the ISR, was associated with an elevated prevalence of OA structural features in the medial and lateral PFJ. Additionally, compared to knees with low ISRs, knees with high ISRs had roughly twice the odds of worsening cartilage damage in the medial and lateral PFJ and BMLs in the lateral PFJ over 30 months. When adjusting for measures of PFJ alignment, there remained an independent association between the ISR and prevalence of structural damage on MRI.
Characteristics/Clinical Presentation
[edit | edit source]
Patella alta is a positional fault defined most simply as the superior displacement of the patella within the trochlear groove of the femur. Patella alta has been shown to be associated with chondromalacia on the articular surface of the patella and pain. Patella alta has also been implicated in patellar osteoarthritis. The prevalence of patella alta in individuals with patellar osteoarthritis was 6 times that of individuals with normal patellar articular cartilage. Additionally, both Leung et al (1996) and Kannus (1992) reported that subjects with anterior knee pain demonstrated a significantly more superior patellar position in the affected knee relative to healthy, control knees.(1)
A common symptom of patellar injury and dislocation is acute pain after direct contact or sudden change of direction. With sudden changes in direction, the femur medially rotates over the ground-stabilized tibia. Under these conditions, athletes commonly feel the knee giving way, which is the result of quadriceps inhibition from pain, a physiologic protective mechanism. Rapid swelling, intense knee pain, and difficulty with any knee flexion usually occur. Other dysfunctions with similar presentations and mechanism of injury are meniscal and ligamentous injuries, particularly injuries of the anterior cruciate ligament.
Symptoms may also manifest as a slowly progressive sensation of anterior knee pain with increased physical activity. Intense physical activity increases JRFs across the knee. Such activities include inclined ambulation, squatting, prolonged sitting, and going up and down stairs. Anterior knee pain aggravated by activity is typical of chondral pathology. Knee pain that improves during physical activity but returns after activity suggests tendinitis.
Differential Diagnosis[edit | edit source]
There are a lot of conditions that are know to be associated with patella alta. For example
• Patellofemoral instability
• Recurrent patellofemoral dislocation
• Neuromuscular diseases (poliomyelitis)
• spastic cerebral palsy
• Osgood Schlatter disease
• Sinding Larsen Johanssen disease
• Patella tendo-lateral femoral condyle friction syndrome
• Chondromalacia patella
Diagnostic Procedures[edit | edit source]
It is not easy to diagnose patella alta. It is difficult to evaluate the correct height as well as the position of the patella in relation to the deeper knee structures. Just by looking and touching it is quite impossible to diagnose patella alta, this is why an x-ray is recommended.
A person that has a patella alta may feel instability in the knee. Patients normally have a swollen knee that is filled with water; this place where the water is localized in the knee may look like a bulging portion just like a camel back.
For confirmation, a lateral X-Ray is made with the knee bent at 90 degrees. This will confirm the patella alta, by measuring its height[8]
Outcome Measures[edit | edit source]
Several methods are used to determine the presence of patella alta. Insall-Salvati were the first to describe a method of establishing patellar height on the basis of the ratio of the length of the patellar tendon to the diagonal length of the patella on lateral radiographs. Various techniques, including those by Blackburne and Peel, Caton et al., and de Carvalho et al., have since been developed in the attempt to classify patellar position.
Examination[edit | edit source]
The patient sits on the edge of the examination table with the feet on the ground. The knees are bent at 90 degrees, and the thigh is horizontally positioned. The vertical position of the patella height is best observed from lateral. In Patella Alta it can be seen that the partially tilted patella protrudes above the level of the thigh. This is more remarkable In a unilateral Patella alta. A patella alta may be noticed during inspection thanks to a so-called Camel hump patella The knee has two striking bulges: one is the tibial tuberosity, the other one is the patella. The space distal to the patella and proximal to the fat body of Hoffa is characterized by a notch[9]
Medical Management
[edit | edit source]
add text here
Physical Therapy Management
[edit | edit source]
Manual gliding is performed to theoretically modify the resting height of the patella before knee extension, resulting in decreased pain in the knee. Correction of the positional fault of the patella by using tape, is a method to correct patellar alignment
Patients noted that they were having minimal difficulty with walking, Their average pain was reported to be a 1–2/10 on a VAS scale, and they noted decreased use of pain medication
Key Research[edit | edit source]
A study suggest that Patellar tendon tenodesis and tibial tubercle distalization result in normalization of patellar tendon length, a stable patellofemoral joint, and good long-term knee function in patients with patella alta. A perfect postoperative stability was found in 76.8% of patients[10]
Resources
[edit | edit source]
add appropriate resources here
Clinical Bottom Line[edit | edit source]
add text here
Recent Related Research (from Pubmed)[edit | edit source]
Failed to load RSS feed from http://www.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1f_dL1krf4HK1DEoRgEOYRNPuUbNvCT2DrzNdWf4-Wi8dcbQ4Z|charset=UTF-8|short|max=10: Error parsing XML for RSS
References
[edit | edit source]
- ↑ Ward SR, Powers CM; The influence of patella alta on patellofemoral joint stress during normal and fast walking; Clin Biomech (Bristol, Avon). 2004 Dec;19(10):1040-7 (Level of evidence: B)
- ↑ Stefanik JJ et al ; Quadriceps Weakness, Patella Alta, and Structural Features of Patellofemoral Osteoarthritis; Arthritis Care Res (Hoboken). 2011 Oct;63(10):1391-7 (Level of evidence: B)
- ↑ Syed A. Ali, Robert Helmer, Michael R. Terk; Patella Alta: Lack of Correlation Between Patellotrochlear Cartilage Congruence and Commonly Used Patellar Height Ratio; AJR November 2009 vol. 193 no. 5 1361-1366 (Level of evidence: B)
- ↑ Florence Peterson Kendall et al.; Spieren: tests en functies, Bohn Stafleu van Loghum, Nederland, 469p (383). Level of evidence D
- ↑ Human kinetics Publisher. Clinical anatomy of the patellofemoral joint. International sports medicine journal. 2001. Level of evidence D
- ↑ Florence Peterson Kendall et al.; Spieren: tests en functies, Bohn Stafleu van Loghum, Nederland, 469p (383). Level of evidence D
- ↑ Human kinetics Publisher. Clinical anatomy of the patellofemoral joint. International sports medicine journal. 2001. Level of evidence D
- ↑ Bohn Stafleu van Loghum (Level of evidence: D)
- ↑ Bohn Stafleu van Loghum (Level of evidence: D)
- ↑ Patellar tendon tenodesis in association with tibial tubercle distalization for the treatment of episodic patellar dislocation with patella alta.fckLRMayer C, Magnussen RA, Servien E, Demey G, Jacobi M, Neyret P, Lustig S. Department of Orthopedic Surgery, Hôpital de la Croix-Rousse, Centre Albert Trillat, Lyon, France (Level of evidence 4)