Patella alta: Difference between revisions
No edit summary |
Neil De Bie (talk | contribs) No edit summary |
||
| Line 18: | Line 18: | ||
The knee joint consists of three bones, the femur, the tibia, the fibula and also the patella which is a sesamoid. | The knee joint consists of three bones, the femur, the tibia, the fibula and also the patella which is a sesamoid. | ||
The patellofemoral joint is the portion of the knee joint between the patella and the femoral condyles. The patellofemoral articulation totally depends on the function of the quadriceps. The quadriceps muscles are connected to the patella with a shared tendon. The quadriceps femoris is divided into four different muscles with the same insertion on the patella: the rectus femoris (RF), the vastus lateralis (VL), the vastus intermedius (VI) and the vastus medialis (VM). There is also a tendon that connects the bottom of the patella to the tibia, called the patellar tendon. This tendon is extremely strong and allows the quadriceps muscle group to straighten the leg. | The patellofemoral joint is the portion of the knee joint between the patella and the femoral condyles. The patellofemoral articulation totally depends on the function of the quadriceps. The quadriceps muscles are connected to the patella with a shared tendon. The quadriceps femoris is divided into four different muscles with the same insertion on the patella: the rectus femoris (RF), the vastus lateralis (VL), the vastus intermedius (VI) and the vastus medialis (VM). There is also a tendon that connects the bottom of the patella to the tibia, called the patellar tendon. This tendon is extremely strong and allows the quadriceps muscle group to straighten the leg.<br><br>The knee joint is one of the largest and most complex joints in the body. It is constructed by 4 bones and an extensive network of ligaments and muscles.[1]<br><br>The thigh bone (Femur), the shin bone (Tibia) and the kneecap (Patella) articulate through tibiofemoral and patellofemoral joints. These three bones are covered in articular cartilage which is an extremely hard, smooth substance designed to decrease the friction forces. The patella lies in an indentation of the femur known as the intercondylar groove.[1]<br><br>The smaller shin bone that runs alongside the tibia (Fibula) and is attached via the superior tibiofibular joint is not directly involved in the knee joint, but provides a surface for important muscles and ligaments to attach to.[2][1]<br><br>The distal aspect of the femur forms the proximal articulating surface for the knee, which is composed of 2 large condyles. The medial and the lateral. These two condyles are separated inferiorly by the intercondylar notch although they are connected anteriorly by a small shallow groove which is known as either the femoral sulcus or the patella groove or patella surface. This engages the patella in early flexion. <br><br>The tibia (shin bone) also has 2 asymmetrical condyles (medial and lateral) of which are relatively flat, These are also known as the tibial plateau. The medial tibial plateau is much longer than the lateral anteroposteriorly, and the diameter of the proximal tibia is much greater than the shaft posteriorly which is sloped at approximately 7 to 10 degrees to facilitate flexion of the femoral condyles on the tibia.<br><br>The two tibial condyles are separated by the intercondylar tubercles, these are two boney spines which are roughened and their role lies within knee extension. They become lodged in the intercondylar notch of the femur, adding to the stability of the joint. Overall the tibiofemoral joint is a relatively unstable joint as the plateau's are slightly convex anteriorly and posteriorly. This emphasises the importance of the other structures of the knee such as the menisci.<br> | ||
== Etiology == | == Etiology == | ||
Revision as of 19:53, 16 January 2017
Original Editors - Fitim Cami
Top Contributors - Neil De Bie, Fitim Cami, Laura Ritchie, Joris De Pot, Kim Jackson, Admin, Simisola Ajeyalemi, WikiSysop and Naomi O'Reilly
Search Strategy[edit | edit source]
The following databases have been used to find information about "Patella alta": Pubmed, Medscape, Google scholar, Pedro, Online database of the VUB
Words that have been used: Patella alta, Conservative treatment AND patella alta, Patella alta AND physical therapy, Patellar dislocation & Etiology
Definition/Description[edit | edit source]
Patella alta or high-riding patella refers to an abnormally high patella in relation to the femur. The patella sits high on the femur where the groove is very shallow. Here the sides of the femoral groove provide only a small barrier to keep the high-riding patella in place. A strong contraction of the quadriceps muscle can easily pull the patella over the edge and out of the groove, leading to a patellar dislocation. This condition has been associated clinically with patellofemoral dysfunction and is considered a predisposing factor for the development of patellofemoral pain (PFP). Patella alta is also characterized as instability of the Patella[1][2][3]
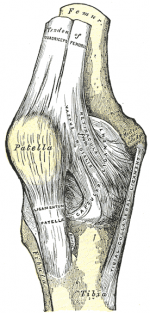
Clinically Relevant Anatomy [4] [5][edit | edit source]
The knee joint consists of three bones, the femur, the tibia, the fibula and also the patella which is a sesamoid.
The patellofemoral joint is the portion of the knee joint between the patella and the femoral condyles. The patellofemoral articulation totally depends on the function of the quadriceps. The quadriceps muscles are connected to the patella with a shared tendon. The quadriceps femoris is divided into four different muscles with the same insertion on the patella: the rectus femoris (RF), the vastus lateralis (VL), the vastus intermedius (VI) and the vastus medialis (VM). There is also a tendon that connects the bottom of the patella to the tibia, called the patellar tendon. This tendon is extremely strong and allows the quadriceps muscle group to straighten the leg.
The knee joint is one of the largest and most complex joints in the body. It is constructed by 4 bones and an extensive network of ligaments and muscles.[1]
The thigh bone (Femur), the shin bone (Tibia) and the kneecap (Patella) articulate through tibiofemoral and patellofemoral joints. These three bones are covered in articular cartilage which is an extremely hard, smooth substance designed to decrease the friction forces. The patella lies in an indentation of the femur known as the intercondylar groove.[1]
The smaller shin bone that runs alongside the tibia (Fibula) and is attached via the superior tibiofibular joint is not directly involved in the knee joint, but provides a surface for important muscles and ligaments to attach to.[2][1]
The distal aspect of the femur forms the proximal articulating surface for the knee, which is composed of 2 large condyles. The medial and the lateral. These two condyles are separated inferiorly by the intercondylar notch although they are connected anteriorly by a small shallow groove which is known as either the femoral sulcus or the patella groove or patella surface. This engages the patella in early flexion.
The tibia (shin bone) also has 2 asymmetrical condyles (medial and lateral) of which are relatively flat, These are also known as the tibial plateau. The medial tibial plateau is much longer than the lateral anteroposteriorly, and the diameter of the proximal tibia is much greater than the shaft posteriorly which is sloped at approximately 7 to 10 degrees to facilitate flexion of the femoral condyles on the tibia.
The two tibial condyles are separated by the intercondylar tubercles, these are two boney spines which are roughened and their role lies within knee extension. They become lodged in the intercondylar notch of the femur, adding to the stability of the joint. Overall the tibiofemoral joint is a relatively unstable joint as the plateau's are slightly convex anteriorly and posteriorly. This emphasises the importance of the other structures of the knee such as the menisci.
Etiology[edit | edit source]
Patella Alta can occur as the result of a sports injury, though the large majority of the time it is a congenital/developmental condition that is unrelated to trauma. Its pathophysiology is not completely clear, but it is hypothesized that one of the causes of Patella Alta, are abnormally long patellar tendons (>52 mm). [6] [7]
Characteristics/Clinical Presentation[edit | edit source]
add text here
Differential Diagnosis[edit | edit source]
add text here
Diagnostic Procedures[edit | edit source]
For confirmation, a lateral X-Ray is made with the knee bent at 90 degrees. This will confirm the patella alta, by measuring its height[8]
Outcome Measures[edit | edit source]
Several methods are used to determine the presence of patella alta. Insall-Salvati were the first to describe a method of establishing patellar height on the basis of the ratio of the length of the patellar tendon to the diagonal length of the patella on lateral radiographs. Various techniques, including those by Blackburne and Peel, Caton et al., and de Carvalho et al., have since been developed in the attempt to classify patellar position.
Examination[edit | edit source]
The patient sits on the edge of the examination table with the feet on the ground. The knees are bent at 90 degrees, and the thigh is horizontally positioned. The vertical position of the patella height is best observed from lateral. In Patella Alta it can be seen that the partially tilted patella protrudes above the level of the thigh. This is more remarkable In a unilateral Patella alta. A patella alta may be noticed during inspection thanks to a so-called Camel hump patella The knee has two striking bulges: one is the tibial tuberosity, the other one is the patella. The space distal to the patella and proximal to the fat body of Hoffa is characterized by a notch[9]
Medical Management
[edit | edit source]
add text here
Physical Therapy Management
[edit | edit source]
Manual gliding is performed to theoretically modify the resting height of the patella before knee extension, resulting in decreased pain in the knee. Correction of the positional fault of the patella by using tape, is a method to correct patellar alignment
Patients noted that they were having minimal difficulty with walking, Their average pain was reported to be a 1–2/10 on a VAS scale, and they noted decreased use of pain medication
Key Research[edit | edit source]
A study suggest that Patellar tendon tenodesis and tibial tubercle distalization result in normalization of patellar tendon length, a stable patellofemoral joint, and good long-term knee function in patients with patella alta. A perfect postoperative stability was found in 76.8% of patients[10]
Resources
[edit | edit source]
add appropriate resources here
Clinical Bottom Line[edit | edit source]
add text here
Recent Related Research (from Pubmed)[edit | edit source]
Failed to load RSS feed from http://www.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1f_dL1krf4HK1DEoRgEOYRNPuUbNvCT2DrzNdWf4-Wi8dcbQ4Z|charset=UTF-8|short|max=10: Error parsing XML for RSS
References
[edit | edit source]
- ↑ Ward SR, Powers CM; The influence of patella alta on patellofemoral joint stress during normal and fast walking; Clin Biomech (Bristol, Avon). 2004 Dec;19(10):1040-7 (Level of evidence: B)
- ↑ Stefanik JJ et al ; Quadriceps Weakness, Patella Alta, and Structural Features of Patellofemoral Osteoarthritis; Arthritis Care Res (Hoboken). 2011 Oct;63(10):1391-7 (Level of evidence: B)
- ↑ Syed A. Ali, Robert Helmer, Michael R. Terk; Patella Alta: Lack of Correlation Between Patellotrochlear Cartilage Congruence and Commonly Used Patellar Height Ratio; AJR November 2009 vol. 193 no. 5 1361-1366 (Level of evidence: B)
- ↑ Florence Peterson Kendall et al.; Spieren: tests en functies, Bohn Stafleu van Loghum, Nederland, 469p (383). Level of evidence D
- ↑ Human kinetics Publisher. Clinical anatomy of the patellofemoral joint. International sports medicine journal. 2001. Level of evidence D
- ↑ Florence Peterson Kendall et al.; Spieren: tests en functies, Bohn Stafleu van Loghum, Nederland, 469p (383). Level of evidence D
- ↑ Human kinetics Publisher. Clinical anatomy of the patellofemoral joint. International sports medicine journal. 2001. Level of evidence D
- ↑ Bohn Stafleu van Loghum (Level of evidence: D)
- ↑ Bohn Stafleu van Loghum (Level of evidence: D)
- ↑ Patellar tendon tenodesis in association with tibial tubercle distalization for the treatment of episodic patellar dislocation with patella alta.fckLRMayer C, Magnussen RA, Servien E, Demey G, Jacobi M, Neyret P, Lustig S. Department of Orthopedic Surgery, Hôpital de la Croix-Rousse, Centre Albert Trillat, Lyon, France (Level of evidence 4)