Palliative Care Competence Framework for Physiotherapists: Difference between revisions
No edit summary |
No edit summary |
||
| Line 166: | Line 166: | ||
*Approximately 90% of people with lymphoedema are affected in their lower body, 9% are affected in the upper body and the remaining 1% are affected in the genital region (Greene 2015).<br> | *Approximately 90% of people with lymphoedema are affected in their lower body, 9% are affected in the upper body and the remaining 1% are affected in the genital region (Greene 2015).<br> | ||
*One third of females with damaged axillary nodes combined with radiation will develop lymphoedema (Greene 2015). A study looked at 744 patients who were treated for breast cancer in British Columbia. They found that 5% of those who had axillary surgery developed lymphoedema, but when radiotherapy was provided in addition to this surgery the percentage increased to 30% (Franks et al 2006).<br> | *One third of females with damaged axillary nodes combined with radiation will develop lymphoedema (Greene 2015). A study looked at 744 patients who were treated for breast cancer in British Columbia. They found that 5% of those who had axillary surgery developed lymphoedema, but when radiotherapy was provided in addition to this surgery the percentage increased to 30% (Franks et al 2006).<br> | ||
*Undergoing surgery as part of breast cancer treatment is one of the most frequent causes of developing secondary lymphoedema. | *Undergoing surgery as part of breast cancer treatment is one of the most frequent causes of developing secondary lymphoedema. 1 in 5 patients will develop this type of lymphoedema 6 months after receiving the surgery (Harmer 2009).<br> | ||
*Hamptom (2015) looked at a population of 600,000 people over the age of 65 and concluded 1 in 200 people had chronic lymphoedema. 50% of these people had a reduced quality of life and hospital care cost the NHS £2300. | *Hamptom (2015) looked at a population of 600,000 people over the age of 65 and concluded 1 in 200 people had chronic lymphoedema. 50% of these people had a reduced quality of life and hospital care cost the NHS £2300. | ||
*Rockson and Rivera (2008) mention that 1.15 in 100,000 people under the age of 20 will acquire primary lymphoedema.<br> | *Rockson and Rivera (2008) mention that 1.15 in 100,000 people under the age of 20 will acquire primary lymphoedema.<br> | ||
Revision as of 22:52, 26 January 2016
Original Editor - Your name will be added here if you created the original content for this page.
Top Contributors - Charlotte Kay, Yasmin Natasha Milne, Emma Clare Sneddon, Sarah Brennan, Lauren Lopez, Kim Jackson, 127.0.0.1, Jane Hislop, Lucinda hampton, Admin and Evan Thomas
Introduction and Learning Outcomes[edit | edit source]
Welcome to this online learning resource focussing on “The role of the Physiotherapist in Palliative Care for people with Lymphoedema”. This has been designed by a group of fourth year Physiotherapy students from Queen Margaret University as part of the “Contemporary and Emerging Issues in Physiotherapy” module.
This learning resource is for indivudal study, aimed at final year Physiotherapy students and new graduates to prepare them for work in the health service. From our own experience and discussing with expert clinicians, the role of a physiotherapist in lymphoedema and palliative care is rarely covered throughout univerisity. Furthermore, only a select few students will gain palliative care experience during their placements. Hence this learning resource is designed to provide students with essential information that they can use throughout their final year and beyond.
Overall the resource should take 10 hours to complete. The learning resource will cover a range of topics including:
- Overview of palliative care (1.5 hours)
- Overview of lymphoedema (1.5 hours)
- Lymphoedema - treatment and management (3.5 hours)
- Physiotherapist's role (2.5 hours)
- Physiotherapy competencies (1 hour)
Throughout the resource there will be a variety of learning activities, including reflections, quizes, additional reading and videos.
Aims
The aim of this wiki is to present a learning resource for final year physiotherapy students and new graduates to develop their knowledge and understanding of:
- The role of a physiotherapist in the management of people with lymphoedema
- The implications for physiotherapy practice when managing people with lymphoedema in a palliative care setting
Learning Outcomes
Learning outcomes are set in relation to Blooms Taxonomy (ref)- as this learning resource is designed for final year students and new graduates, the outcomes are mostly set appropriately at higher levels of the taxonomy.
By the end of this wiki you should be able to:
- Discuss the background of lymphoedema and describe the key presenting symptoms
- Summarise the history of palliative care and explain how this care is provided
- Critically evaluate the role of the physiotherapist in the treatment of lymphoedema with reference to current literature
- Critically appraise the role of a physiotherapist treating lymphoedema in a palliative care setting compared to a non-palliative setting
Overview of Palliative Care[edit | edit source]
Definition and history
[edit | edit source]
When you hear the term palliative care, what does it mean to you? Take a moment to think about this and take note of your answer.
Definition:
The WHO defines palliative care as “an approach that improves the quality of life of patients and their families facing the problem associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial and spiritual” (WHO 2015).
A more general description may define palliative care as any care that helps to alleviate symptoms whether or not there is hope for a cure.
Aims of palliative care:
- To maintain quality of life until death
- Provide relief from pain or other symptoms which may cause distress
- Help patients to live as actively as possible
- Help family members to cope during a patient’s illness and during their own bereavement
- Integrate spiritual and psychological aspects into a patient’s care
- Be applied early and in conjunction with other therapies (NHS 2004)
History:
Hospices in the UK and Ireland have been around since the 1900s, however, they were few in number and run by religious foundations to provide care to the poor.
During the 1950s, there was considerable professional and public interest in cancer but the main focus was on curative treatment. Patients who were considered terminal and were dying from cancer were overlooked and were told to go home as there was nothing that could be done or were scattered in various hospital wards, abandoned by doctors.
In the postwar years, a shift began to emerge in the published work with new studies showing both the clinical and social aspects of care for patients who were dying from cancer. This work in oncology helped to shape the worldwide development of palliative care (Clark 2007).
Cicely Saunders may be recognized as the founder of the palliative care movement around the 1970’s.
Having trained as a nurse and then a social worker, in 1959, Saunders qualified in medicine and began working in St. Thomas’s Hospital in London (Baines 2011).
In 1960, Saunders focused her attention on patients who were in the final stages of cancer, especially those patients with complex problems from the point of view of pain and general distress. Her research and writings were built on the individual experiences of her patients and by 1967 she had collected data for 1100 cases, where she described the physical and mental suffering of each patient (Clark 2007). Saunders inspired the concept of total pain which includes physical, emotional, social, mental and spiritual components and believed in constant pain management to relieve suffering.
In 1967, Cicely Saunders opened St. Christopher’s Hospice in London which was the world’s first modern hospice. Here, she brought together large numbers of patients with terminal illness and staff to take care of them (Baines 2011). The hospice quickly became an inspiration and established itself as a centre of excellence, giving equal importance to clinical care, education and research. Research was done on pain control and the administration of strong opiates. These clinical and organizational studies would go on to play a major role in the advancement on palliative care (Clark 2007).
The success of St. Christopher’s Hospice soon became a catalyst for the development of hospices in the UK. During the 1980s, about 10 new hospices were opened a year, some were funded by the NHS and others were privately or charity funded.
There was also a development among hospitals and in 1976 a terminal care team was established in St. Thomas’s Hospital, London. Between 1982 and 1996 the number of hospitals with a multidisciplinary palliative care team or a specialist nurse more than quadrupled to 275 from 5.
During this time, two well known UK charities also assisted in influencing change. The first of these charities was the Macmillan organization which was founded in 1911. During the 1970s the organisation went through a period of phenomenal expansion. The organisation became more involved in palliative care and supporting specialist professional posts, academic positions and service development.
The second charity is the Marie Curie Memorial Foundation, established in 1948. This foundation was involved in creating a domiciliary nursing service for patients with cancer. It created nursing homes and ran a laboratory-based research programme. During the 1980s when new hospices were opening across the UK, the Marie Curie nursing homes evolved into specialist palliative care centres and the charity supported more research and educational activities in palliative care (Clark 2007).
By the 1990s there were over 1000 specialist Macmillan nurses and 5000 Marie Curie nurses working across the UK in palliative care.
By 1987, palliative medicine was established as a subspecialty of general medicine and in 1995 the specialty of palliative care was formally approved (Clark 2007).
Causes of death[edit | edit source]
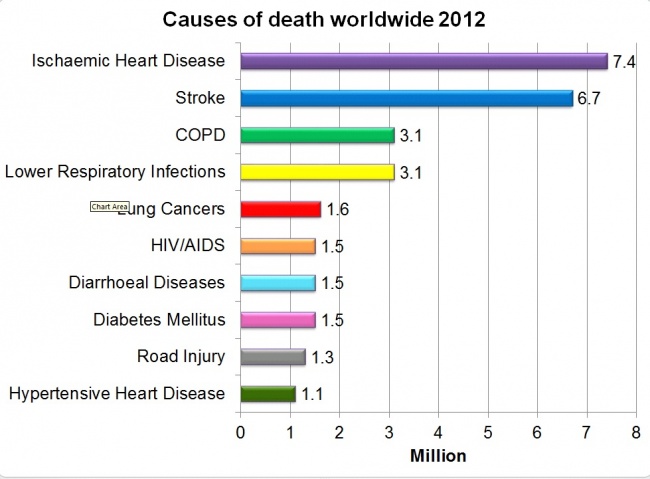
When looking at who needs palliative care and who should provide it, we need to look at epidemiology and the causes of death across the world. Epidemiology is important when planning health services as it can provide information about disease and symptom occurrence to guide healthcare needs. Life expectancies vary worldwide. Variations are associated with certain demographic characteristics such as political, occupational, cultural and lifestyle risks while also including gender, ethnicity and genetics. Low-income countries may have lower life expectancy then developed countries. In 2012, life expectancy was estimated globally at 66yrs for men and 71yrs for women. However, in more developed countries, life expectancy is estimated at 76.9years for both sexes and 58.4years in the least developed countries.
This is only a broad reflection of the figures as reported causes vary among countries at different levels of economic development.
Future projections – mortality projections may aid the planning of health services and the knowledge and skills clinicians will require in order to meet the needs of future populations
Service delivery[edit | edit source]
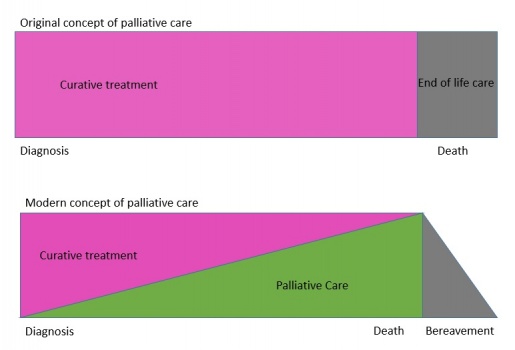
Since the inception of the modern hospice and palliative care movement led by Cicely Saunders, palliative care has continued to evolve, has developed into a medical specialty and is now integrated into mainstream medicine in many countries. Palliative care was originally seen as something only concerned with the end of life but has now been incorporated with other services offered throughout the entire disease trajectory.
Palliative care is now a more seamless process through the disease trajectory, either from the point of diagnosis or at any point in the disease compared to the original concept where care was offered once curative treatment had failed and patients were seen at an end of life stage.
Due to the aging population in developed countries, the burden of disease on healthcare will continue to increase, challenging the knowledge and skills of professionals. With the advances in treatments for cancer and other conditions, patients are living with more co-morbidities and palliative care services must be prepared to provide care over longer periods of time throughout the disease trajectory.
Where care is provided?[edit | edit source]
Palliative care takes place in many different settings.
Can you think of any settings where palliative may take place?
Hospices possibly being the most known setting. Hospices can be a ward or unit within a hospital or can be a stand-alone service. Hospices in the UK are generally stand-alone services with the aim of alleviating disease or therapy-related discomfort and stabilising the status of patient by offering psychological and social support. Cicely Saunders once said that hospices should be a welcoming environment and have a sense cheerfulness and peace.
Hospital palliative support teams – provide advice to patients, their family, carers and other clinical staff. The teams provide education and liaise with other services both in and out of hospital. An aim of the team is to alleviate multiple symptoms patients may have by sometime prescribing directly or will advise on the management of symptoms.
Home care teams – provide specialist direct care to patients in their home where they support families and carers. The team may provide specialist advice to GPs, nurses or other clinicians involved in the patient’s case. There is good evidence to show the benefits of home specialist palliative care compared with usual care.
Outpatient services – this service is available for patients who live at home but are able to attend clinics. These services may be offered from a hospital or inpatient palliative care unit. This service can help to introduce patients to the palliative care process earlier where advanced care planning can be put in place. There is little to no evidence on the effect of these services.
Day care centres – these are spaces in hospitals, hospices or the community which are specially designed to provide additional support to patients and their families. Usually patients who attend a day centre are already in the care of a home palliative care team. The nature of the service offered may vary depending on the patient’s needs, from medical/health orientated to more recreational or social services where complementary therapies may also be offered
Who provides care?[edit | edit source]
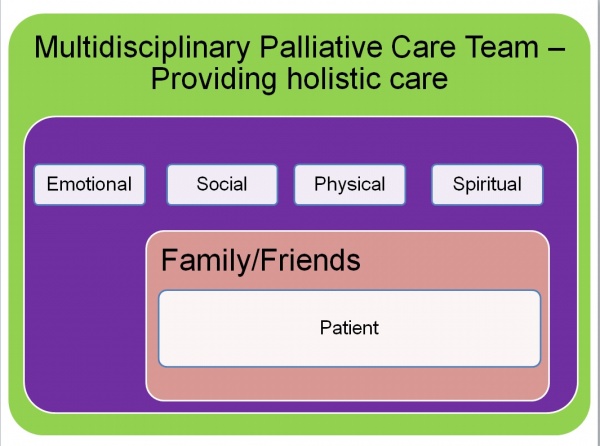
Palliative care uses a team approach to affirm life and help support patients to live as actively as possible until death by enhancing their quality of life. Care should be offered as patient needs develop and should be an integral part of care in any setting (WHO 2004). Care is focused on controlling pain and other symptoms based not on disease prognosis but on the needs of the patient and must be flexible to adapt to these needs (WHO 2004).
Professionals involved – multidisciplinary teams are the key to all palliative care services. Specialist palliative nurses or physicians are usually part of all services but other professionals may be involved depending on the service. Social workers, physiotherapists, occupational therapists, psychologists, pharmacists and religious officials may be part of a patient’s care.
Overview of Lymphoedema[edit | edit source]
Introduction[edit | edit source]
This section of the wiki will aim to provide an overview of:
- The pathophysiology of lymphoedema
- The two types of lymphoedema - primary and secondary
- The four stages of the condition
- Clinical features (physical and psychological) those with the condition may present
- Two of the main leading causes related to lymphoedema - cancer and infection
- Epidemiology regarding the condition
Epidemiology[edit | edit source]
Epidemiology focuses on why diseases or conditions develop in different societies and how common the occurnace is. The prevalance is the volume of people who are 'at risk' of having the condition at the same time. The incidence is the portion of new people that have acquired the condition over a specific period of time (Franks et al 2006).
The epidemiology regarding lymphoedema isn't widely reported because it isn't a notifiable disease (Foldi and Foldi 2006). However, the condition is becoming more common and the cost of healthcare required can put financial strain on the NHS. Therefore, it is important to understand the prevalance to help improve current and future healtcare and disease management (BMJ 2016).
- Lymphoedema occurs in approximately 240,000 people in the UK with older adults more susceptible than the younger population (Nazarko 2015).
- Cellulitis is a one of the leading causes in developing lymphoedema. In 2003-2004 there were 45,522 cellulitis admissions reported by the NHS Institue for Innovation and Improvement (MacMillan 2011).
- Approximately 90% of people with lymphoedema are affected in their lower body, 9% are affected in the upper body and the remaining 1% are affected in the genital region (Greene 2015).
- One third of females with damaged axillary nodes combined with radiation will develop lymphoedema (Greene 2015). A study looked at 744 patients who were treated for breast cancer in British Columbia. They found that 5% of those who had axillary surgery developed lymphoedema, but when radiotherapy was provided in addition to this surgery the percentage increased to 30% (Franks et al 2006).
- Undergoing surgery as part of breast cancer treatment is one of the most frequent causes of developing secondary lymphoedema. 1 in 5 patients will develop this type of lymphoedema 6 months after receiving the surgery (Harmer 2009).
- Hamptom (2015) looked at a population of 600,000 people over the age of 65 and concluded 1 in 200 people had chronic lymphoedema. 50% of these people had a reduced quality of life and hospital care cost the NHS £2300.
- Rockson and Rivera (2008) mention that 1.15 in 100,000 people under the age of 20 will acquire primary lymphoedema.
- A study surveyed 308 centres (2743 people) in Spain and found that 36.8% suffered from primary lymphoedema. Of the 36.8%, 2% had acquired it at birth, 30% during adolescence and 68% were older adults (Williams et al 2005).
- Ridner (2013) discussed the incidence rates of cancer survivors developing lymphoedema. It was reported that one study concluded from a total of 287 breast cancer survivors, 48% had upper limb swelling at least once and 34% had clinical symptoms of lymphoedema 6 years post treatment.
Lymphatic system[edit | edit source]
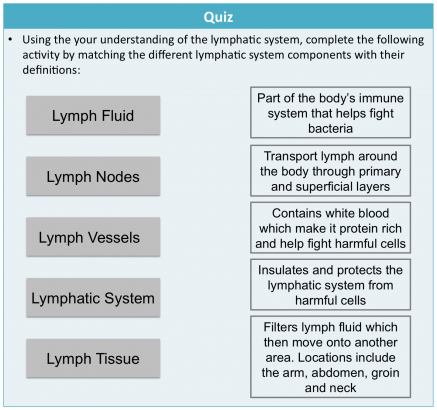
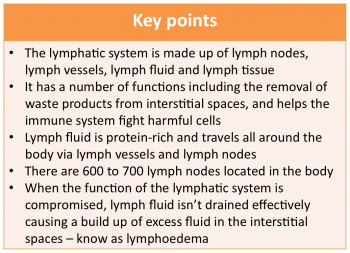
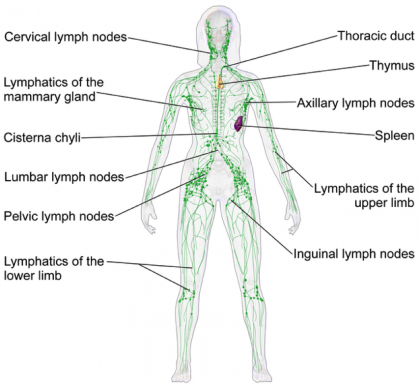
The lymphatic system is part of the body's immune system that plays a role in fighting harmful cells, for example, bacteria. It consists of lymph fluid, lymph nodes, lymph vessels and lymph tissue.
Lymph tissue insulates and protects the lymphatic system from damaging cells. Lymph fluid contains infection-fighting white blood cells. It circulates throughout the lymphatic system and is formed when interstitial fluid is collected through lymph channels (vessels, ducts and capillaries).
Lymph is primarily made up of a white watery substance:
PICTURE OF LYMPH COMPOSITION
The main lymphatic functions:
1. Helps immune system respond to the body
2. Redistribution of fluid in the body
3. Lymph carries proteins, solids, and liquids away from tissue space
a. Remove waste products from interstitial space (between all body tissue) (Seifter et al 2005)
b. Bacteria, toxins and foreign bodies are removed from tissues
4. Controls the flow of large molecules around the body (National Lymphoedema Network 2013)
5. Controls tissue fluid homeostatsis (Ridner 2013) to maintain the structure and functional aspects of tissue.
The flow of lymph fluid is unidirectional, towards the heart to provide cells with oxygen. It is protein-rich and fights abnormal cells due to its white cell content (Cancer Research UK 2014).
Lymph nodes tend to be found in clusters ingrained within adipose tissue (contains fat cells). Their shape and size varies depending on gender and where the nodes are located in the body (Foldi and Foldi 2006). There are approximately 600 to 700 lymph nodes located around the body, specifically under the arm, in the abdomen, groin and neck. (Hampton 2015). Their role involves receiving lymph fluid via afferent vessels and transporting it around the body via efferernt vessels using specific lymph channels located on left and right sides. The fluid then passes through superficial primary lymph vessels (that drain the skin) and is emptied into deep secondary lymph vessels (which also contains drainage from internal organs). Adequate flow of lymph fluid is dependant on muscle contractions and an efficient respiratory system, for example, exercise (Kerchner et al 2008).
Examples of lymph nodes located in the upper body include: axillary; lateral; subscapular; pectoral; upper and lower; central; infraclavicular; subpectoral and interpectoral nodes. Some of the lymph nodes located in the lower extremities include: inguinal; superficial inguinal and the intercalated nodes. As stated above, there are a number of lymph nodes located in the abdomin and pelvic areas, for example, iliac; lumbar; gastric; pancreaticosplenic; mesenteric; hepatic and rectal lymph nodes.
The lymphatic system can become blocked from localised fluid retention and tissue swelling within the body – known as Lymphoedema (a chronic inflammatory disease). It occurs when the function of the lymphatic system is compromised in some way. Lymph pathways are unable to exchange nutrients effectively within the interstitial spaces, causing a build up of excess fluid. Upper and lower extremities are affected depending on which area of the body is damaged. The cause of onset determines whether the affected person has either primary or secondary lymphoedema.
Types of lymphoedema[edit | edit source]
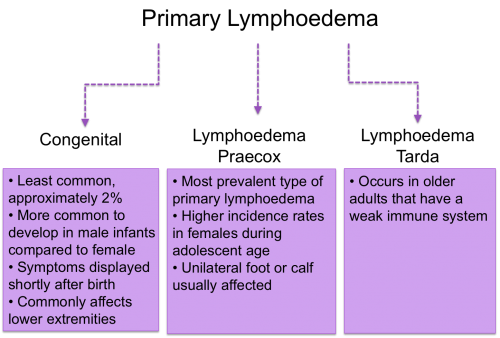
Primary
Approximetaly 1 in 6000 people develop primary lymphoedema. This form of lymphoedema isn’t inherited through family history and wouldn’t be passed onto future generations. However, people can develop primary lymphoedema in relation to other genetic and congenital abnormalities wehre the lymph nodes or lymph vessels don't develop properly (Foldi and Foldi 2006). Currently there isn't a large body of evidence regarding the causes of lymphoedema. Future research is required to further investigate developmental causes to ensure effective treatments are provided (Woods 2007).
Primary lymphoedema can be either idiopathic, intrinsic or spontaneous. Idiopathic means there is no know cause, intrinsic results from an abnormal lymphatic system and sponanetous means the condition has developed on its own without any interference (Woods 2007).
There are three classifications depending on the onset of symptoms:
(Greene 2015)
Secondary
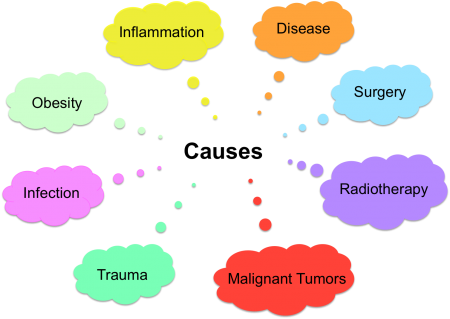
Secondary lymphoedema is more common than the primary form. The lymphatic system is damaged due to an external cause compromising the function of the lymph nodes. Consequently, swelling accumulates in the affected part of the body.
Causes of secondary lymhoedema include (NHS Choices 2014):
- Malignant tumours - the presence of cancer tumours can block the flow of lymph fluid
- Surgery (cancer and non-cancer related) – increases the risk of disturbing the function of lymphatic pathways
- Radiotherapy - destroys cancerous tissue but can also damage healthly lymph nodes
- Infections – contributes to increased swelling in the affected area
- Inflammation – contributes to excess fluid build up in the affected area
- Obesity – increased the pressure on the lymphatic system that could ultimately damage lymph nodes
- Disease - for example, venous, joint, diabetes
- Trauma - lymphoedema can occur followng severe trauma, for example, compound fractures
In more developed countries malignancy and the treatments associated with the condition are the main root of cause for acquiring secondary lymphoedema (Kerchner 2008). Although the treatments have a number benefits, their outcomes can lead to disruption of the lymphatic system. If a patient receives radiation treatment in addition to cancer surgery, they are at a higher risk of aquiring lymphoedema.
In developing countries the most common cause of secondary lymphoedema is filiariasis, a parasitic infection with filarial worms (WHO 2016). It commonly occurs in areas of poverty where there is poor sanitation and diseased water (Woods 2007). An infected female mosquito bites the human and a parasite enters the lymph vessel causing lymph vessel paralysis. The condition occurs in appproximately 120 million people in the world (Foldi and Foldi 2006). The physical and psychological effects of filiariasis intensify poverty because those affected become socially isolated and unable to carry out daily activities.
Causes of upper limb lymphoedema include (The Lymphoedema Support Network year):
- Trauma or injury – removal of lymph nodes during breast cancer surgery, upper body radiotherapy, burns, and scarring
- Cancer that has spread to the upper body compromising the function of the lymph nodes
- Following deep vein thrombosis (DVT) or high doses of intravenous (IV) drugs
- Reduced upper limb mobility as a result of an illness, for example, multiple sclerosis or stroke
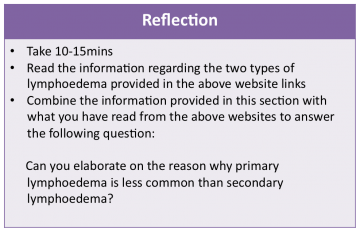
Activity
The following links will be used in the reflective activity:
- http://www.lymphoedemasupport.com/articles/focus-on-primary-lymphoedema
- http://www.lymphoedemasupport.com/articles/focus-secondary-lymphoedema
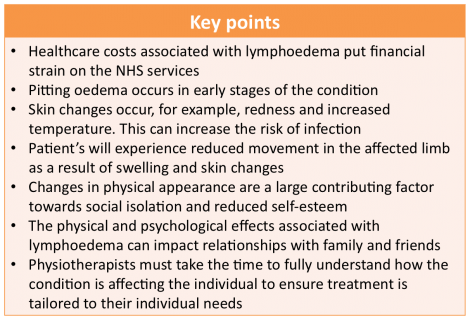
Clinical Features[edit | edit source]
There are both physical and psychological effective of the chronic condition. Early diagnosis is vital to ensure the correct treatment is chosen.
Physical changes
- In the early stages pitting oedema occurs where the skin is pressed leaving an indent in the swelling. Elevating the arm creates a draining effect to reduce swelling
- Limbs can feel heavy and achy
- There is altered sensation, for example, pins and needles
- Reduced mobility and range of movement of the affected limb/s
- Pain and joint discomfort
- Skin changes, for example redness and increased temperature
- Nail discoloration (Lyons and Modarai 2013)
- Hyperkeratosis (thickening of the skin) and lymphangiectasia (dilated superficial lymph vessels) (The Lymphoedema Support Network 2015)
(Cancer Research UK 2014; McCallin et al 2005)
When the condition affects the lower extremities, over time the affected person’s gait pattern is altered, leading to a higher risk of disability.



Psychological effects
There are psychological effects associated with the condition as a result of changes to body image.
- Swelling and weight gain impact physical appearance that can affect one’s perception of how they look, consequently decreasing their self-confidence (Harmer 2009; McCallin et al 2005)
- People commonly detach themselves from social events with family and friends leading to social isolation (Ridner 2009)
- Disturbed sleeping pattern
- Some people may feel they have a lack of support
- Financial concerns as a consequence of treatment cost and potential job loss/change (Ridner 2009)
- Some cancer survivors that have aquired secondary lymphoedema feel that it can be a constant reminder of previously having cancer (Greene 2015)
- For those that experience unilaterael lymphoedema, commonly different sizes of garmets have to be worn on each side of the body and oversized clothes have to be worn because items such as jeans dont fit the limbs (Greene 2015). Psychologically this can largely impact the person because they may not feel comfortable with the way they look and therefore exclude themselves from public situaitons
Mason et al (2008) conducted a systematic review of literature that looked at the psychosocial aspects related lymphoedema. It was found that people with the condition experience anger, depression, anxiety and relationship issues. People can feel embarrassed having to wear different clothes due to compression bandaging, swelling and weight gain. Ultimately, there is an overall decrease in quality of life (QoL) from reduced social and leisure activities. The study concluded more research is required that focuses on improving specific psychosocial issues rather targeting QoL to reslove issues such as anger and depression.
Another study looked at the incidence, cost of treatment and complications of lymphoedema following breast cancer treatment. It concluded that 10% of the 1877 participant showed signs of lymphoedema 2 years after breast cancer treatment. A complication of the condition was the high medical costs for treatment. This lead to increased length of stay in hospital and ultimately reduced the patient’s quality of life (Ridner 2009).
It is important for health professionals to recognise and fully understand the psychological and psychosocial implications for each individual patient to ensure person-centred care is provided. Communication and appropriate referrals to other health professionals is important in overall management of the condition, for example social workers and psychologists.
Below is a summary of the key points to remember from this section:
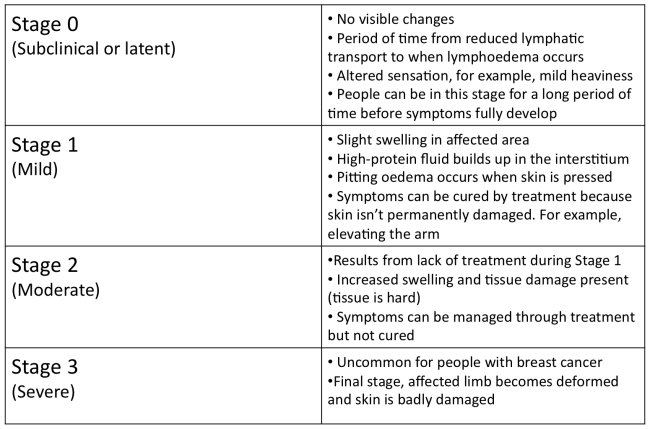
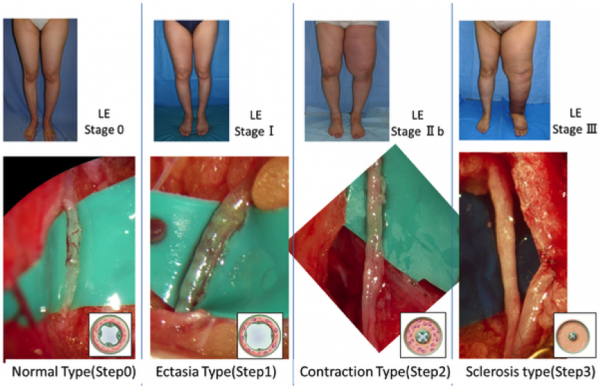
Stages of lymphoedema[edit | edit source]
(breastcancer.org 2015)
There are 4 Stages of lymphoedema:
Lymphoedema is a chronic and incurable condition so treatment strategies focus on reducing disease progression, for example, swelling management and infection prevention.
Leading causes[edit | edit source]
Cancer
Lymphoedema following breast cancer surgery is the highest overlooked cause of secondary lymphoedema. Harmer (2009) states approximately 20% of people will acquire lymphoedema after receiving this treatment. The procedure involves removing one or more lymph nodes located under the arm, leaving fewer lymph nodes to drain all the lymph. Continually working under high pressures eventually causes the remaining lymph nodes to become damaged and lymph leaks into the lymph vessels. Consequently excess fluid builds up in the affected area (breastcancer.org 2015).
Cancer Research UK (2014) discusses the vicious cycle between cancer and the body’s immune system. Cancerous cells are destroyed by the immune system and treatments for cancer. However, the condition can weaken the immune system if lymph nodes are blocked by cancerous tissue and unable to function properly.
A combination of surgery and radiotherapy treatment leads to a higher risk of acquiring secondary lymphoedema. Radiation therapy aims to stop cancer from coming back by using high-radiation energy to destroy cancerous cells (National Cancer Institute 2010). It either occurs before surgery to reduce the size of a tumour, or after surgery to abolish the remainder of the tumour. Lymphoedema can occur as a result of this treatment when the function of the lymphatic system has been comprised and fluid isn’t drained away (NHS Choices 2014).
Infection
Infection is a key issue commonly related to lymphoedema. It either results from swelling or causes it to develop (Hampton 2015). Lymph nodes help fight infections but when they are damaged infections can develop quicker. Infection usually develops follwing a break in the skin, for example a cut. It is important patients receive treatment quickly to prevent the infection becoming acute and spreading within the affected area, a common antibiotic used is penecilin (Greene 2015). The Lymphoedema Support Network (2010) defines cellulitis as “acute spreading inflammation of the skin and subcutaneous tissue”. It causes the skin to become warm, red, swollen and painful with onset either sudden or progressing over a few hours. If the lymph tissue is damaged there is added strain on the lymphatic system. In an infected limb, the inflammatory process cause attracts fluid causing an increase in swelling. Consequently, lymphoedema is exacerbated during this period of infection (McGilvray year).
75-90% of cellulitis occurs in the lower body and is caused by bacteria entering inflamed or broken skin. A study found that the condition was responsible for 3% of admissions in a UK hospital (Al-Niaimi and Cox, 2009). This common occurrence puts financial strain on the NHS; therefore, infection prevention is a large part of lymphoedema treatment. There is a strong link between leg cellulitis and lymphoedema, where progression of the condition can lead to ulceration and septicaemia. Each cellulitis episode exacerbates secondary lymphoedema, which in turn increases the risk for a further infection episode. A Cochrane review found that a quarter of lymphoedema patients would acquire cellulitis (Al-Niaimi and Cox, 2009).
Picture above: Cellulitis in a lower limb
Activity
Now it's time to get your thinking hat on...
By now you should have an understanding of the causes of lymphoedema and the presenting symtoms. Use the information provided in this section and in the link below to complete the following activity:
Activity[edit | edit source]
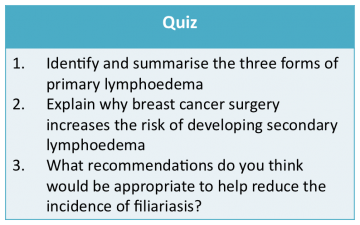
Well done, you have successfuly completed this section of the wiki module! Now it's time to test yourself and put your newfound knowledge into practice..
Take approximately 15 minutes to complete the following quiz. The aim of the quiz is to answer all the questions correctly before the time runs out, good luck!
Conclusion[edit | edit source]
The aim of this section is to provide an overview of lymphoedema. It’s important to understand the background of how lymphoedema develops and the presenting symptoms associated with the condition so that clinicians choose the most appropriate treatment strategy.
You should also feel comfortable discussing the following areas:
- Epidemiology
- Pathophysiology
- Types and Stages of lymphoedema
- Clinical features
- Leading causes
By now you should have achieved learning outcome 1:
Discuss the background of lymphoedema and describe the key presenting symptoms
The next section of the learning resource will focus on discussing the physiotherapist’s role in managing lymphoedema and critically analyses a range of available treatments. Before progressing onto this section, please ensure you have taken time to complete all the activities above.
Lymphoedema - Treatment and Management[edit | edit source]
Introduction[edit | edit source]
This section will discuss the treatment and management options for people with lymphoedema. By the end of this section you should have achieved learning outcome number 3 - "critically evaluate the role of the physiotherapist in the treatment of lymphoedema with reference to current literature".
Throughout the section a number of learning activities including reflections, quizzes and case studies will be used to help consolidate your learning. Additional reading links will also be provided throughout to expand on what is included in the resource.
The Chartered Society of Physiotherapy (CSP) produced a document outlining the background and treatment of lymphoedema[1]. This document states that patient's will undergo 3-4 weeks of intensive therapy, followed by lifelong monitoring, which includes self-management and 6 month reviews. The need for early access to specialist physiotherapy intervention in order to prevent serious complications is also highlighted.
Activity: Take 5 minutes to read through the document[1] and note down the key points (please note this document is only available for CSP members).
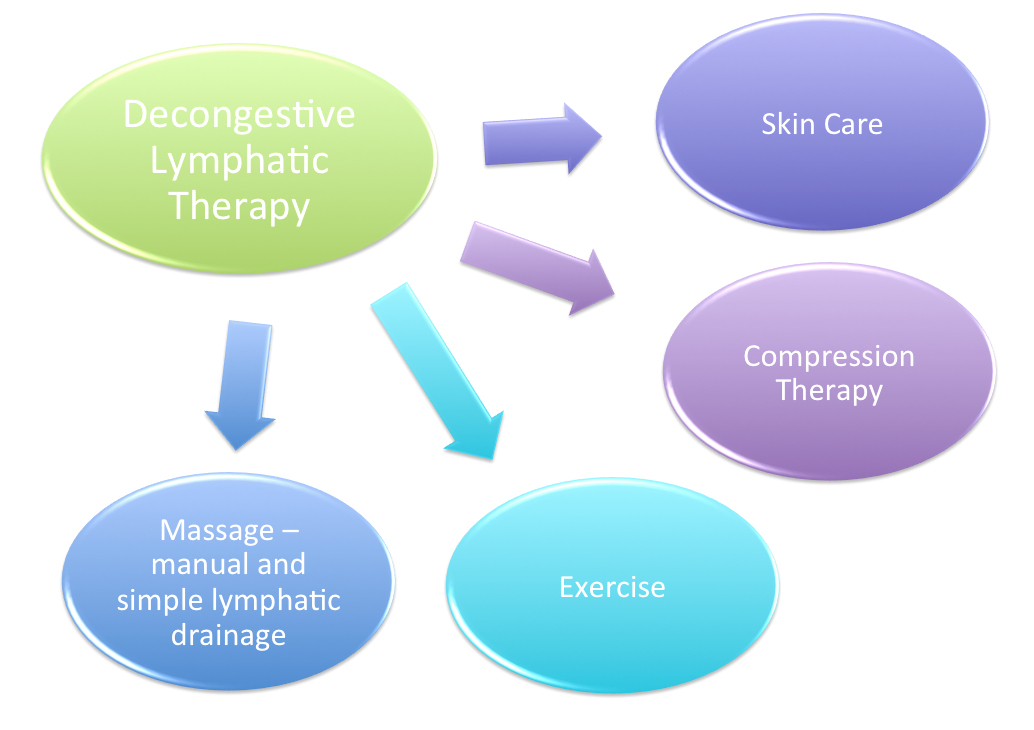
Decongestive lymphatic therapy (DLT) as discussed by the CSP is viewed as the gold standard of care for lymphoedema[2].This treatment approach is effective and significantly reduces the percentage excess limb volume as well as improving quality of life[3] .
Decongestive lymphatic therapy encompasses four main components[4];
The treatment of lymphoedema should be specifically tailored based on the site, severity and complexity as well as their psychosocial situation[4]. The success of treatment does not solely rest on the therapist; patients and carers must play an active role from an early stage.
Alongside the physical difficulties that people with lymphoedema face, emotional and social implications may also arise. Evidence has suggested that through specific management and targeting of the physical symptoms, the psychosocial issues can be reduced to enhance the individual’s quality of life[3].
As previously mentioned the management of lymphoedema is split into intensive and maintenance stages, both of which have very different approaches. The goals during the intensive stage of therapy are to reduce and control the swelling, maintain skin quality and educate the patient in order for them to reach a stage where they are ready to progress into the maintenance phase of treatment[5]. This is achieved through a number of approaches aiming to reduce the load and decongest the lymphatic system, stimulate the function and encourage drainage through various routes[4].
Once swelling is bought under control patients will progress to the maintenance stage. During this stage people with lymphoedema are educated to self manage their condition and will be reviewed less frequently by a specialist.
Over the next four sections of this learning resource you will learn about the different components of DLT with reference to the literature which supports their use.
Activity:
Prior to moving on, take 5 minutes to complete the following quiz (the answers can be found in the text and additional reading above).
Compression therapy[edit | edit source]
This section will discuss the first of the four elements of DLT.
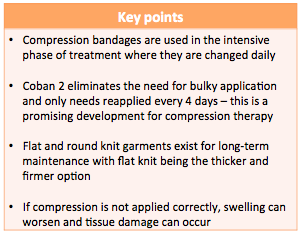
Compression therapy consists of two main methods – multilayer lymphoedema bandaging (MLLB) and compression garments. Overall, compression therapy increases lymphatic drainage, reduces capillary filtration, promotes fluid movement to less compressed areas of the body and improves the action of the venous pump[6]. Furthermore, bandaging aims to improve the shape of the limb, soften fibrosclerotic tissue, support and improve skin condition and manage symptoms[7].
Once no further benefit is being obtained from compression bandaging during the intensive phase, patients should be managed by compression garments for long-term maintenance[8]. MLLB may also be used as part of long-term management if compression garments are not suitable [7].
The combined treatment of bandaging followed by compression hosiery has been found to yield better results for reduction of moderate to severe lymphoedema, which was maintained for at least 6 months, compared with hosiery alone [9]. These results came from a relatively large randomised controlled parallel-group trial. Hence the International Consensus recommends this course of treatment for people with lymphoedema.
Compression bandaging
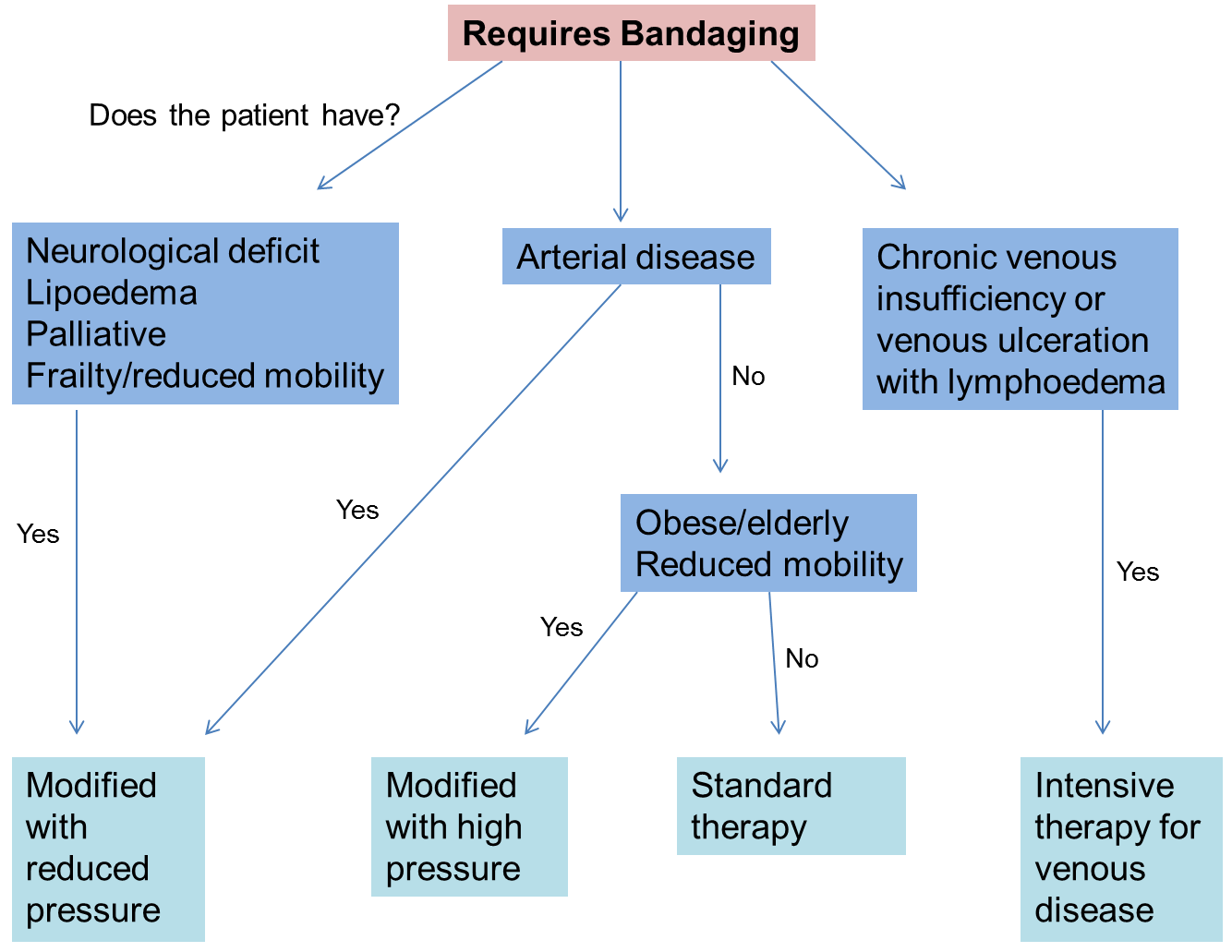
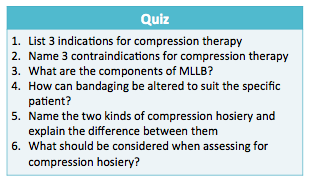
Indications for compression therapy as stated by the Lymphoedema Framework are[4]:
- Fragile, damaged or ulcerated skin
- Distorted limb shape
- Limb too large for compression garments
- Areas of tissue thickening
- Lymphorrhoea
- Lymphangiectasia
- Pronounced skin folds
There are a number of contraindications stated below[4]:
- Severe arterial insufficiency
- Uncontrolled heart failure
- Severe peripheral neuropathy
The following flow chart visualises the decision making process that clinicians undertake if compression bandaging is indicated. Based on the patient's presenting symptoms, condition and medical history, they may require slightly modified treatment.
Additional reading: refer to pages 6-7 of this document[7] to read more about how the modifications are made (approx. 10 minutes)
Bandages used are inelastic which result in high and low pressures exerted during movement and rest respectively[7]. Elastic bandages produce less variation of pressure; these may be indicated if patients are immobile, have venous ulceration, lymphatic or venous disease or if the expected time of application is longer than normal[4].
As with most treatments, MLLB can be adapted to suit the patient needs by either adjusting pressure, frequency of reapplication, bulk of bandage and type of bandage[4]. If pressure is not applied correctly venous and lymphatic flow can be compromised, therefore the proximal movement of fluid is reduced and swelling may present in the extremities[7]. When applied to the lower limb, care must be taken to ensure that the patient is still able to wear shoes during treatment as normal gait pattern is encouraged to maintain an effective calf and foot muscle pump[7].
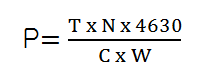
Pressure applied is calculated using Lapase's Law:
P = pressure under the bandage (in mmHg),
T = bandage tension (Kgf)
N = number of layers
C = limb circumference (cm)
W = bandage width (cm)
The following two videos show the application of MLLB to upper and lower limb lymphoedema. By watching these, you should gain a clearer idea of the appearance of MLLB and how it is applied by a specialist physiotherapist or other health care professional.
Bandaging a lymphoedema arm: (approx. 10 mins)
Bandaging a lymphoedema leg: (approx. 10 mins)
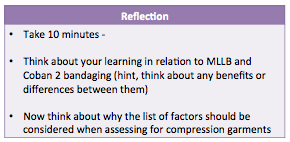
Inelastic and elastic bandages have been discussed, however more recently, a new bandaging system known as Coban 2 has been developed which can be used an alternative to MLLB. Coban 2 consists of a comfort layer and a compression layer that cohesively bond together[10]. MLLB consists of a thick padding layer covered with multiple compression layers. Coban 2 bandaging eliminates the need for this, resulting is a less bulky appearance and allowing the patient more mobility and freedom.
Lamprou and colleagues[10] conducted a prospective randomised controlled trial comparing Coban 2 with traditional bandaging methods in the treatment of lower limb lymphoedema. The results of this study found Coban 2 to be equally as effective in reducing limb volume.
Franks and colleagues[11] studied the use of Coban 2 in arm and leg lymphoedema. Again this study supported the use of Coban 2 in the effective management of lymphoedema with the lower limb showing a greater reduction in swelling.
Although both of the above studies had relatively small sample sizes (40 and 24 participants respectively) resulting in low statistical power, they both showed encouraging results for the use of the new bandaging system.
A multicentre randomised controlled trial with 82 participants investigating the frequency of application of Coban 2[12]. Results found constant therapeutic effect was maintained when bandages were reapplied every four days. Compared with MLLB, which requires reapplication daily at certain stages of treatment, the Coban 2 bandages allow patients to have more freedom and independence.
This next video shows the application of Coban 2 bandaging and explains some more information about this new system.
Activity: Take 5 minutes after watching this video to note down the differences between the two types of bandaging systems.
Coban 2 bandaging: (approx. 10 mins)
As discussed, a number of trials have evaluated the effects of compression bandaging for lymphoedema, which have found positive results. The development of Coban 2 bandages is encouraging, however this still requires larger scale trials to fully evaluate the efficacy.
Now that compression bandaging has been considered, this wiki will now move on to discuss the use of compression garments which are used for the long-term management of limb shape and swelling[4].
Compression Garments/Hosiery
Compression garments are hand made-to-measure. These will be considered once regular limb shape has been restored and the patient’s skin is fully intact and robust enough to tolerate the use of garments[13][14].
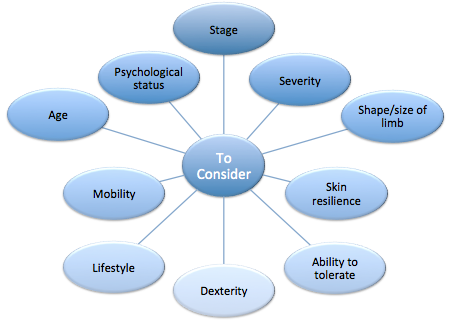
Although garments are important in the management of lymphoedema, patient and clinician must come to an informed decision regarding the appropriateness of this treatment modality.
Doherty et al.[13] explains a number of factors that should be considered when assessing for compression garments (see image below). Once these have been considered and the patient is deemed appropriate for compression garements, meaurements will be taken by a qualified health professional, which may be a physiotherapist.
Additional reading: Take 10 minutes to refer to the Best Practice for the Management of Lymphoedema[4] pages 40-41 where you will find more information about fitting and measuring for lymphoedema compression garments
Once the progression from bandages to garments has been made, swelling and other symptoms must be monitored. If swelling is not controlled within the first three months of wearing compression garments, clinician and patient should consider further intensive therapy using MLLB[7].
Garments are either constructed as a flat knit or a round knit. Flat knit knitted as a flat garment then joined at the seams, these are generally thicker and firmer. Round knitted garments are viewed as more aesthetically pleasing, as they are thinner than flat knit and are continuously knitted cylindrically without any seams[4].
Once measurement and construction of the garment is completed advice regarding the care at home will be provided in person and leaflets may also be given to the patient[4]. If garments are poorly fitted, the swelling may not be contained and damage can occur to the tissues. This could result in discomfort and reduced tolerance leading to patients being unwilling to use compression hosiery as a long-term management option[13].
As well as limb compression garments, if patients have trunk or breast lymphoedema garments or specialised bras can be provided[4].
Activity
Before progressing to the next section please take 15 minutes to check your knowledge:
By now you should have a clear understanding of the role of compression therapy in the management of lymphoedema and the evidence to support it. The additional reading and YouTube videos should have provided you with more knowledge about modifications, applying MLLB and Coban 2 bandages and measuring for compression.
Ensure you are able to answer the questions in the quiz above (all answers are provided throughout the text and additional reading).
Below is a summary of the key points to remember from this section.
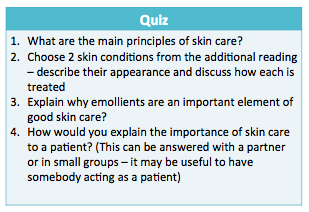
Skin care[edit | edit source]
This section will discuss the role of skin care in the treatment and management of lymphoedema.
As a consequence of swelling, large skin folds can appear where infections may develop [4]. Infections can also arise if the skin becomes damaged or broken, therefore adequate skin care to maintain the integrity and manage any problems that occur is fundamental in the care of people with lymphoedema[4][15].
At both intensive and maintenance stages, it is important to emphasise the need for a skin care regime to maintain the skin integrity.
The main principles of skin care are:[8][16] 
During assessment, health professionals must inspect the skin condition using palpation and observation to check for any changes or damage[16]. If changes have occurred these must be monitored and managed correctly.
Following assessment, the skin will be cleansed and emollients applied.
Washing removes dirt and bacteria from the skin, this is essential to prevent infection; however washing can remove the protective lipid layer that prevents water loss and protects the skin from infection. Therefore emollients are applied to re-establish this layer thus preventing any further water loss and maintaining the protective barrier[8]. Following cleansing of the skin, it is highly important to ensure skin, in particular the skin folds are dried properly.
Abrasive or scented soaps should be avoided and natural or pH neutral soaps are recommended[4][16]. This is because normal soaps contain detergents, are often scented and include preservatives, which can irritate or dry the skin.
Emollients are available in various forms including, moisturisers, soaps substitutes or bath oils. Moisturisers area also available in different forms including creams, lotions and ointments[16]. The Lymphoedema Framework[4] recommends the use of ointments, which contain little or no water; this hydrates the skin better than creams and lotions.
The body’s natural response to sunburn is to increase blood flow to the affected area. For people with lymphoedema this will increase the load on an already impaired lymphatic system and may increase swelling. Therefore it is advised that people with lymphoedema take extra care to avoid sunburn[16].
Despite the treatment offered infections may still occur that must be managed by thorough skin hygiene, ensuring skin is dried following washing and an anti-fungal powder or cream applied until the infection disappears[16].
Although skin care is an integral part of lymphoedema management, some patients experience barriers that prevent adequate skin care and result in infections. James[17] studied the perceived barriers to skin care, which included physical limitations, expense, poor understanding, anxiety and motivational issues. This indicates that health professionals play a large role in educating patients about the importance of skin care to facilitate self-management. Health professionals should be aware of these potential barriers and be able to overcome them through education and support to facilitate self-management
The main principles of skin care have been discussed for intact skin, however as discussed a number of skin conditions or infections can arise. Take 10 minutes to undertake this additional reading (from 'Intact Skin' on page 24, stopping before 'Cellulitis/Erysipelas' on page 27 of 'Best Practice Management of Lymphoedema'[4].). This reading will provide you with additional information about how different skin conditions are managed in practice. It will also provide you with a description and picture of how the stated condition appears. This is particularly useful as final year and new graduates – you may be involved in the assessment or treatment of this patient group, therefore it is important that you have the knowledge to identify these conditions.
You have now reached the end of this section, at this stage you should understand the main principles of skin care and how these are delivered in practice.
Activity – take 5 minutes to complete the following quiz to test your knowledge before progressing. All answers can be found in the text above or throughout the additional reading.
Below is a summary of the key points to remember from this section.
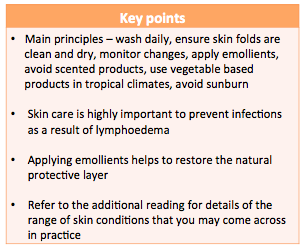
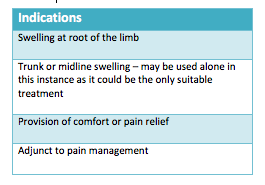
Exercise[edit | edit source]
This section will discuss exercise for people with lymphoedema. With new evidence, traditional beliefs about the effects of exercise on lymphoedema have been disproven.
MacMillan Cancer Support[18] state that many individuals experience reduced quality of life following cancer treatment due to secondary complications, which can include lymphoedema. Despite the general well known benefits of exercise including reduced risk of chronic diseases and the positive impact it can have on mental health[19], studies report that cancer survivors often fail to return to their pre-diagnosis levels of physical activity[20][21].
Traditionally strenuous exercise was discouraged in patients with lymphoedema based on the belief that it may exacerbate the condition[22]. However recent studies and systematic reviews contradict this statement.
Cancer Rearch UK provides an informative section on their website for people with lymphoedema.
Before progressing take 10 minutes to read through this page[23]. By reading this information you will learn about how exercise influences lymphoedema and examples of exercises for different areas of the body. This is a useful resource as it is written in layman language, which is easy to understand by patients. This may also assist you as future clinicians to find ways to explain complex terms to your patients.
Now that you have read more about exercise and lymphoedema, the following table summarises some of the studies that have been conducted surrounding this topic.
| Study Title | Design | Participants | Intervention | Outcome Measures | Results |
|---|---|---|---|---|---|
| Effect of Upper Extremity Exercise on Secondary Lymphedema in Breast Cancer Patients: A Pilot Study[24] | Pilot study | 14 breast cancer survivors with unilateral upper limb lymphoedema | Progressive upper body exercise programme – 8 weeks vs. no intervention | Arm circumference and volume Medical Outcomes Trust Short From 36 – survey |
No changes in lymphoedema Physical, general and vitality components of QOL improved |
| Exercise and Secondary Lymphedema: Safety, Potential Benefits, and Research Issues[25] | RCT | 32 breast cancer survivors with lymphoedema | Mixed type exercise programme – 12 weeks vs. no intervention | Bioimpedence spectroscopy and perometry | No changes – did not exacerbate lymphoedema |
| Weight lifting in Women with Breast-Cancer-Related Lymphoedema[26] | RCT | 141 breast cancer survivors with stable arm lymphoedema | 2x weekly progressive weight lifting vs. no intervention | Severity of lymphoedema, number and Incidence of exacerbations and symptoms and muscle strength | No effect on limb swelling, reduced exacerbations and symptoms, increased muscle strength |
| Systematic Review and Meta-Analysis of the Effects of Exercise for Those With Cancer-Related Lymphoedema[27] | Systematic review and meta-analysis | Individuals with secondary lymphoedema 25 studies included |
Range of exercises | Lymphoedema and associated symptoms | No effect on lymphoedema or associated symptoms Insufficient evidence for use of compression during exercise |
| Exercise in patients with lymphedema: a systematic review of the contemporary literature[28] | Systematic review | Cancer patients with or at risk of lymphoedema 19 studies included |
Range of exercises | Lymphoedema development and exacerbations | No development or exacerbation of lymphoedema |
| Weight training is not harmful for women with breast cancer-related lymphoedema: a systematic review[29] | Systematic review and meta-analysis | Women with or at risk of developing breast cancer related lymphoedema 11 studies included |
Progressive weight training exercise | Severity and incidence of arm lymphoedema, upper limb muscle strength, BMI and QOL | Increased strength without affecting arm volume or incidence of lymphoedema No effect on BMI Potential to improve some elements of QOL |
There is little evidence to recommend the optimal mode of exercise for people with lymphoedema; therefore larger scale trials are required to evaluate this. However, the most recent systematic review discussed that by giving people a choice over their exercise method promoted adherence to the programme[29].
Singh et al.[27] also reviewed the use of compression garments during exercise. Unfortunately due to the range of effects that wearing compression can have during exercise, there was no definitive answer to whether compression garments should be worn or not. The authors suggest that this decision should be made on an individual basis considering factors such as stage, severity, and stability of lymphoedema and patient preference.
Evidence suggests that exercise supervised by a qualified professional i.e. a physiotherapist in the first instance to ensure correct technique and reduce injury risk[28].
It can be concluded from the body of evidence including large randomised controlled trials and recent systematic reviews that strenuous training, as previously thought does not lead to the development or worsening of lymphoedema. Despite showing little effect on lymphoedema, it is important to note the benefits that exercise has on individual’s strength, functioning and quality of life. These benefits outweigh any risks that were previously suggested.
To put this in relation to practice, physiotherapists and other health professionals should be encouraging patients with lymphoedema to undertake exercise programmes. Professionals should make individuals aware of the benefits that exercise can have on physical and mental wellbeing and reassure them that exercise will not worsen their lymphoedema.
Activity - take 10 minutes to think about the following case study. This can be discussed in groups if you would like to.
Case Study
Mrs. X. is a 34-year-old lady with (R) upper limb lymphoedema who completed her cancer treatment 11 months ago. She independently manages her lymphoedema with skin care; self massage and wears a compression garment. Prior to her diagnosis – Mrs. X. attended a range of gym classes including high intensity training and strength-based classes’ 3x a week, as well as running at weekends. Mrs. X. tells you she would like to return to her previous level of activity but is concerned that exercise may make her lymphoedema worse. She asks you for advice about what exercises are safe for her to do.
- What advice would you give her?
- Can you think of any exercises that she could do?
Have a think about this yourself at first. However, if you are struggling refer to the Cancer Research UK[23] document or this document[30] which provide advice about what and how exercise should be undertaken with lymphoedema.
You have reached the end of this section. By now you should have an understanding of how exericse is used in the treatment of lymphoedema and the evidence which supports this.
Below is a summary of the key points from this section.
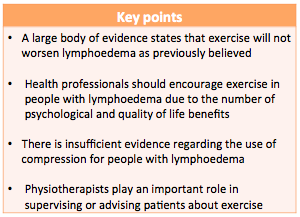
Manual and simple lymphatic drainage[edit | edit source]
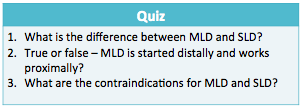
This section will discuss the final part of DLT known as manual and simple lymphatic drainage.
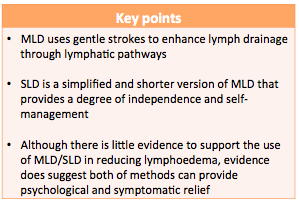
Emil Vodder came up with the method of manual lymphatic drainage (MLD) in 1936. He stated “MLD along with breathing and relaxation exercises and improved diet would play a key role in lymphatic disorders” [31]. This method of massage uses gentle strokes to enhance lymph drainage through lymphatic pathways[4]. The treatment is conducted by trained professionals and is used in combination with the other components of decongestive therapy, as it is not enough to be used alone[4].
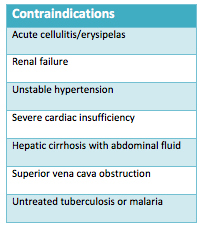
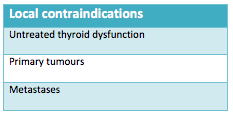
Below the tables show the indications, contraindications and local contraindications of MLD[4].
Principles and technique[4][31] :
• Slow repetitive movements
• Aims to increase lymph drainage without altering capillary function
• Alter interstitial pressures by varying hand movements
• Moves proximally to distally
• Incorporates breathing techniques (deep diaphragmatic breathing) to encourage drainage from deep abdominal lymph nodes and vessels
• Up to one hour daily
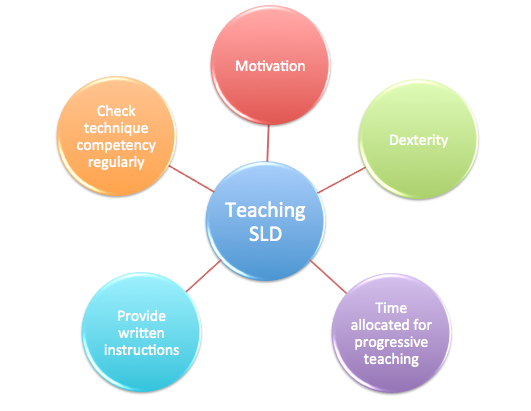
As well as MLD, another form of this treatment is Simple Lymphatic Drainage (SLD) - a simplified version of MLD that can be taught to people with lymphoedema or their carers to form part of a self-management programme. MLD can be performed for up to one hour daily, however SLD is performed for 10-20 minutes[32].
Prior to teaching SLD to individuals, health professionals must consider:
MLD has been found to reduce limb volume, improve quality of life and lymphoedema symptoms in people with cancer related lymphoedema[33]. However, this study had a number of flaws limiting its quality, indicating the need for further research in this area. When comparing MLD to SLD, Sitzia et al.[34] suggests MLD to be more beneficial at reducing limb swelling. However these results were from a small pilot study and did not reach statistical significance.
A more recent systematic review[35] evaluated the effects of MLD in preventing and treating breast cancer related lymphoedema. Overall the findings from this review were unable to support the use of MLD in the prevention or treatment of lymphoedema in this patient group.
Although the evidence discussed was unable to support the use of MLD and SLD to treat lymphoedema, the Lymphoedema Framework[4] still recommend it as one of the cornerstones of decongestive lymphatic therapy. The framework suggests that despite the efficacy not being proven, MLD and SLD both have clear psychological and symptomatic benefits. Pyke[32] discussed that massage can reduce fear and reassure patients that although their skin is painful and may be damaged it can still be touched.
Overall it can be condlued that further evidence is required to fully evaluate the benefits of MLD or SLD in the management of lymphoedema. The benefits may not reach statistical significance but the impact that MLD or SLD could have on an individual’s quality of life are important to consider. Furthermore SLD, although little evidence to support its use allows the patient some independence, as they are able to take some responsibility for the management of their condition.
You have reached the end of this section. You should now be able to discuss the role of MLD and SLD in the treatment of lymphoedema.
Activity - take 5 minutes to complete the following quiz. The answers are provided throughout the text above.
Below is a summary of the key points from this section.
Conclusion[edit | edit source]
This section has discussed the management options for people with lymphoedema, focussing on the 4 main cornerstones of decongestive lymphatic therapy.
The evidence base has been discussed along with the recommendations provided by the Best Practice for the Management of Lymphoedema Framework [4].
It is important to note that the treatments discussed are not stand alone therapies. Ideally, the treatment of lymphoedema should contain all components of DLT to manage symptoms and reduce complications[8].
Despite relatively sound evidence base supporting the use of DLT as a whole, when looking into the separate components the quality of trials is not as reliable. As discussed there is a need for larger scale trials to fully evaluate the use of specified treatments in the management of lymphoedema.
Before progressing onto the next section of this wiki, please ensure you have taken the time to answer all the quizzes at the end of each sub-section.
By now you should be able to –
Summarise and explain the physiotherapy management options for people with lymphoedema.
Physiotherapist Role[edit | edit source]
Introduction[edit | edit source]
Physiotherapists help people to maximise their potential and maintain or improve their quality of life. In palliative care, physiotherapists have many roles.
These include:
- Assessment
- Symptom management
- Education and communication
- Rehabilitation and function
- Some psychological aspects of care
Assessment[edit | edit source]
This section will detail what is involved in an assessment carried out by physiotherapist's when in a palliative setting and the different types of assessment and outcome measures available.
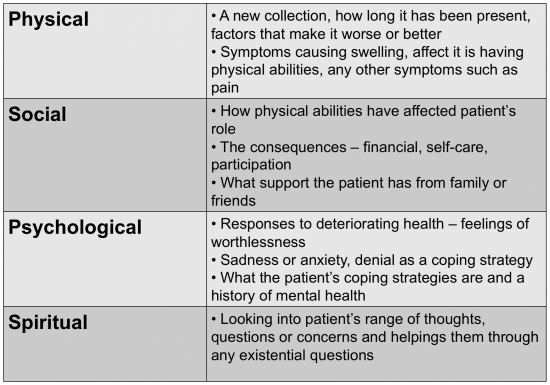
Palliative and specialised palliative care services offer a multidisciplinary team (MDT) approach. Key principles must be applied to the assessment such as considering the patient as a whole person, focusing on quality of life rather than quantity, management should be decided by the patient and there should be good communication for effective assessment and management (ILF 2010). The assessment should involve a patient-centred approach in order to elicit the physical, social and psychological needs of the patient (Todd 2009b).
The assessment should aim to:
- Understand the patient’s main concerns, goals and priorities
- Help the clinician understand the main cause of and the mechanisms behind the swelling
- Understand the underlying condition and how quickly it is progressing
Oedema is a direct result of multiple factors relating to a terminal illness. It can be distressing for patients and a management challenge for health professionals. It is estimated that 5-10% of new referrals to palliative care have oedema but this is also thought to be underestimated (ILF 2010). Heavy and swollen limbs can cause proximal pain while patients with active malignancy may experience neuropathic pain due to nerve compression. Up to 67% of patients experience pain as a result of oedema. For patients, lymphoedema may be seen as a constant reminder of their cancer or illness. The swollen limb is heavy and uncomfortable which leads to a reduction in mobility and function (Todd 2009a).
The assessment includes a full history of the oedema including the following areas:
All areas are combined with a history of the illness to understand the underlying causes better and a history of medication (ILF 2010).
An examination is then carried out and baseline measurements are taken. This helps to plan the programme of care, assess the response to treatment, identifies risks of complications and may show signs that confirm the cause of the oedema. However, the assessment is ongoing with constant reviewing as the disease progresses and patient priorities change (Todd 2009a). From the assessment, the priority will be to negotiate a care plan based on the patient’s problems and the best approach to alleviate these problems (Todd 2009b).
Hollistic Needs Assessment
A Holistic Needs Assessment (HNA) is an assessment tool that was specifically developed for cancer patients and should be used during every cancer patient’s care. It can make a large impact on a patient’s overall care experience and can greatly improve outcomes through recognising and resolving any problems quickly (National Cancer Survivorship Initiative 2013).
The assessment is a process of collecting and discussing information with the patient to develop a clear understanding of what the patient knows, understands and needs. This holistic assessment considers the whole person as their well-being is discussed along with all physical, emotional, spiritual, mental, social and environmental factors. The results from this assessment are all incorporated to create a specific care plan for the patient (National Cancer Action Team, 2013).
It has been shown that having a holistic needs assessment near the end of a patient’s treatment helps to identify the areas that need to be discussed with a healthcare professional. The information from this discussion will then be used to develop a care plan with the patient. The care plan is there to support the patient during and after their treatment and should include;
• Addressing any physical or everyday concerns
• Direction to local or national support groups
• Information about local Health and Wellbeing Clinics,educational events or self management courses available
• Referral to appropriate healthcare professionals for support
• Lifestyle advise/changes
• Information or referral to an appropriate physical activity programme
• Information or referral for advice on diet and nutrition
• Referral for psychological support
• Support related to work and finance concerns
• Support for spiritual needs
(National Cancer Survivorship Initiative 2013).
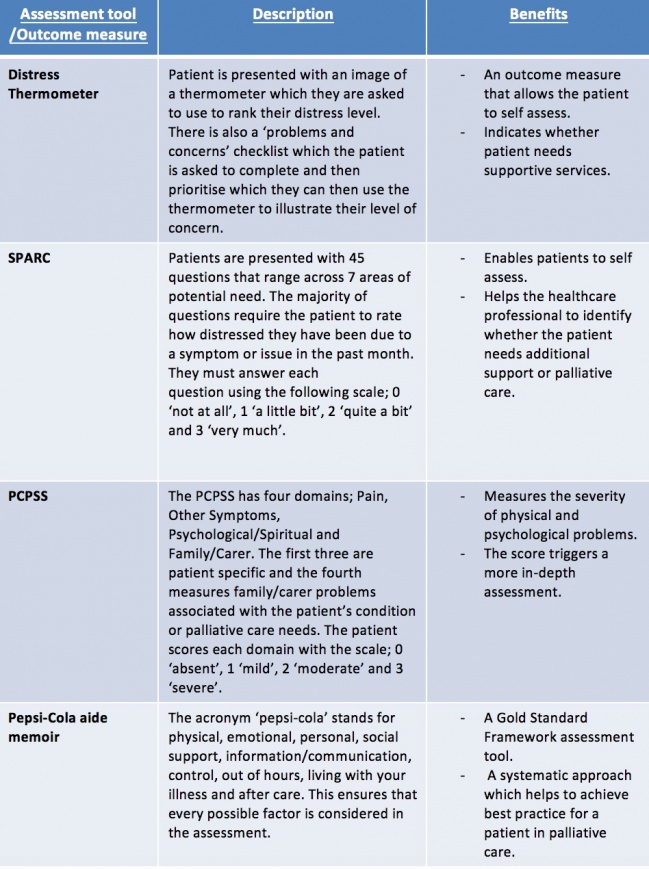
Outcome Measures
An outcome measure is a tool used to measure the quality of delivery of patient care and indicator of whether an intervention has had any positive effect or not (CSP 2016).
The use of an outcome measure as a tool can be very valuable during an assessment. The main benefits are:
• Ensures that the patient’s needs are the main focus
• When used effectively, it provides a structured assessment conversation allowing the patient’s worries to be prioritised
• Ensures that all areas of assessment are covered
• Patients become familiar with the tool and can be carried out by many different healthcare professionals involved in their care
(National Cancer Action Team 2013)
There are a vast amount of outcome measures and assessment tools available to physiotherapists. The most commonly used within a Palliative setting include:
• Distress Thermometer
• Sheffield Profile for Assessment and Referral for Care (SPARC)
• Palliative Care Problem Severity Score (PCPSS)
• The Pepsi-Cola aide-memoire
Treatment challenges [edit | edit source]
This section explains the challenges physiotherapist's face when treating and setting goals for palliative patients with lymphoedema.
The main aim of palliative rehabilitation is to set treatment goals that allow a patient to maintain or improve functions and delay the effects of their disease for as long as possible. To lose their functional ability can cause a patient to view themselves differently and lose their independence which can be very detrimental to a patient. Therefore, physiotherapists have a huge role in helping patients to maintain their independence and achieve other goals they may have (Frymark et al 2009).
Working as a physiotherapist within a palliative care setting can be very challenging as you must have a solid knowledge base about the disease your patient has as well as common physiotherapeutic treatment methods which you will have to adapt for a palliative patient as the treatment goal will be different. Goals need to be short-term and adaptable due to the changing nature of a palliative condition. Therefore, sometimes it is necessary to do a new assessment every time you see a patient due to how much their condition can vary (Frymark et al. 2009).
When it comes to specifically lymphoedema patients, physiotherapists usually work towards the goal of restoring ‘near normal’ limb shape and size. However, in a palliative setting this goal is often unrealistic, therefore, goal setting must be sensible and based on what the patient needs or wants. When goal setting the patient should; have close involvement with the physiotherapist and other health professionals involved in their care and be educated on how to self-manage symptoms. Acceptable palliative goals may include, slowing down the progression of swelling and reducing other symptoms associated with lymphoedema [4].
Patients may have dramatically reduced physical capacity. If their illness has compromised neurologic structures, they may be plegic or paretic, and therefore unable to self- bandage or perform remedial exercises. Further, they may be significantly limited by symptoms such as fatigue and dyspnoea due to marked deconditioning. The coordination, dexterity and strength requirements for bandaging and donning compression garments can elude even healthy patients; therefore, these potential difficulties should be considered when formulating a management plan for terminally ill patients [4].
Management[edit | edit source]
Traditionally Lymphoedema is managed with decongestive lymphatic therapy (DLT) and is based on four pillars of care: compression, massage, skin care and exercise (Todd 2009b). However, routine intensive management using decongestive lymphatic therapy may not be appropriate due to weakness and frailty so must be modified and adapted.
In a palliative setting, physiotherapists need to approach lymphoedema management with an understanding that disease processes are dynamic and may progress rapidly. In order to offer patients long-term relief, the chosen treatment plan must also have the ability to adapt quickly therefore treatment must be feasible and flexible. Therefore, DLT is modified to suit the needs of a palliative patient.
Modified DLT has the capacity to significantly benefit patients with far advanced disease who have lymphoedema or multi-factorial oedema. DLT can enhance patients’ function and comfort while preventing needless complications and enhancing psychological well-being (ILF 2010).
Here is a reminder of the components of DLT that were discussed in section 3:
• Compression (bandages or garments)
• Manual Lymphatic drainage
• Exercises
• Skin care
Modified Decongestive Lymphatic Therapy[edit | edit source]
This section will go on to discuss the modifications made to decongestive lymphatic therapy when working in a palliative setting.
Compression bandaging
Patients with mild swelling can be managed in compression garments either ready made or made to measure. Poorly fitted garments can damage the skin and push fluid to areas that have no compression applied, e.g. fingers. Palliative bandaging consists of layers of padding and short-stretch bandaging over a cotton liner and will include bandaging the digits. In palliative patients there is a risk of forcing fluid into adjacent areas, e.g. the genital or breast area. Expertise is required to judge the correct amount of pressure to apply to support the swollen limb but prevent truncal swelling. Any bandaging, therefore, should be carried out or supervised by a lymphoedema practitioner (Todd 2009).
Manual lymphatic drainage
Manual lymph drainage (MLD) is highly effective in the palliative setting. It has pain relieving properties and can significantly clear even tight, malignant oedema. MLD should avoid areas of dermal compromise, cancerous invasion, extensive fibrosis, or skin hypersensitivity. However, if MLD has been found to be effective over such areas, the treatment should be continued as the main aim of palliative care is to better a patient’s comfort and quality of life (ILF 2010).
Exercise
Normal use of the limb can be sufficient to assist lymphatic flow but even normal use may be restricted in palliative patients. Pain, weight of the limb, fatigue or neurological impairment will impact on limb mobility. Relatives and carers could assist in some passive exercises if tolerated. Elevation of the limb will help reduce the gravitational component of the swelling, e.g. supporting the arm on a pillow or cushion to prevent pooling at the elbow. (Todd 2009) Aerobic activities to stimulate lymphatic return should be encouraged to patient tolerance. Aerobic exercise minimises psychological distress and fatigue among cancer patients, even those with advanced and widely disseminated disease (ILF 2010).
Skin Care
In palliative patients, the skin can become very fragile and the aim is to prevent any damage. Care should be taken to wash and dry thoroughly, especially between the digits and any skin folds. Apply an unscented moisturiser to prevent drying of the skin. If compression hosiery is being applied care should be taken to prevent damage during application. Any breaks in the skin will cause lymphorrhoea – lymph fluid leaking onto the surface of the skin. The extent of the lymphorrhoea will depend on the size of the tear in the skin and whether the limb is dependent or not. The fluid causes maceration of the skin, soaking of clothing, footwear and bedding and can be very cold and distressing for the patient. Mild lymphorrhoea can be treated with an absorbent dressing and continuing with compression hosiery. In some cases, however, the management is purely palliative as bandaging may not stop the lymphorrhoea, especially if the patient is sitting in a chair for the majority of the time. Bed rest is occasionally the only cure for lymphorrhoea and this inevitably takes place as the patient gets closer to death (Todd 2009).
Evidence
Research is limited in the area of modified decongestive lymphatic therapy. Much of the advice and literature available is based on expert opinion only (ILF 2010).
Generally it has been found that patients undergoing decongestive lymphatic therapy for the management of lymphoedema have improved outcome measures when participating in a therapist supervised exercise session as part of treatment compared to carrying out a therapist-taught home exercise programme (ACPOPC 2015).
Reducing the size of an oedematous extremity may dramatically enhance patients’ functionality. Many patients are significantly deconditioned therefore eliminating burdensome limb volume can maximise mobility thereby reducing their risk of immobility-associated problems. Limb volume reduction may be a key factor in allowing patients to remain independent in activities of daily living (ILF 2010).
More literature that details experience with palliative patients is needed. Randomised trials are difficult to conduct in this population therefore case study based trials would be valuable (Towers 2013).
Below is some additional reading that details the
Case study
[edit | edit source]
Competency Framework[edit | edit source]
Conclusion[edit | edit source]
Link to clinical practice and KSF[edit | edit source]
Overview of learning outcomes[edit | edit source]
References[edit | edit source]
References will automatically be added here, see adding references tutorial.
- ↑ 1.0 1.1 Chartered Society of Physiotherapy. Physiotherapy Works: Lymphoedema. http://www.csp.org.uk/publications/physiotherapy-works-lymphoedema (accessed 20 January 2016)
- ↑ Chang CJ, Corimer JN. Lymphoedema Interventions: Exercise, Surgery and Compression Devices. Seminars in Oncology Nursing 2013;29(1):28-40. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23375064 (accessed 15 January 2016).
- ↑ 3.0 3.1 Kim SJ, Park YD. Effects of complex decongestive physiotherapy on the oedema and the quality of life of lower unilateral lymphoedema following treatment for gynaecological cancer. European Journal of Cancer Care 2007;17:463-468. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18637114 (accessed 15 January 2016).
- ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 4.11 4.12 4.13 4.14 4.15 4.16 4.17 4.18 4.19 4.20 4.21 4.22 4.23 4.24 Lymphoedema Framework. Best Practice for the Management of Lymphoedema. International consensus. http://www.woundsinternational.com/media/issues/210/files/content_175.pdf (accessed 15 January 2016)
- ↑ Korpan ML, Crevenna R, Fialka-Moser V. Lympedema A Therapeutic Approach in the Treatment and Rehabilitation of Cancer Patients. American Journal of Physical Medicine and Rehabilitation 2011; 90(5):69-75. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21765266 (accessed 15 January 2016).
- ↑ Cooper G. Compression therapy in oedema and lymphoedema. British Journal of Cardiac Nursing 2015;8(11):547-551. Available from: http://www.magonlinelibrary.com/doi/10.12968/bjcn.2015.20.3.118 (accessed 15 January 2016).
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 7.6 European Wound Management Association. Lymphoedema bandaging in practice. http://ewma.org/fileadmin/user_upload/EWMA/pdf/Position_Documents/2005__Lymphoedema/English_focus_doc_05.pdf (accessed 16 January 2016)
- ↑ 8.0 8.1 8.2 8.3 Lymphoedema Framework. Best Practice for the Management of Lymphoedema – 2nd Edition. Compression Therapy: A position document on compression bandaging. http://www.lympho.org/mod_turbolead/upload/file/Resources/Compression%20bandaging%20-%20final.pdf (accessed 17 January 2016)
- ↑ Badger CMA, Peacock JL, Mortimer PS. A Randomised, Controlled, Parallel-Group Clinical Trial Comparing Multilayer Bandaging Followed by Hosiery versus Hosiery Alone in the Treatment of Patients with Lymphedema of the Limb. Cancer 2000;88(12):2832-2837. Available from: http://www.ncbi.nlm.nih.gov/pubmed/10870068 (accessed 15 January 2016).
- ↑ 10.0 10.1 Lamprou, DAA, Damstra RJ, Partsch H. Prospective, Randomised, Controlled Trial Comparing a New Two-Component Compression System with Inelastic Multicomponent Compression Bandages in the Treatment of Leg Lymphoedema. Dermatologic Surgery 2011;37(7):985-991. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22002586 (accessed 15 January 2016).
- ↑ Franks PJ, Moffatt CJ, Murray S, Reddick M, Tilley A, Schreiber A. Evaluation of the performance of a new compression system in patients with lymphoedema. International Wound Journal 2012;203-209. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22432947 (accessed 15 January 2016).
- ↑ Moffatt CJ, Franks PJ, Hardy D, Lewis M, Parker V, Feldman JL. A preliminary randomised controlled study to determine the application frequency of a new lymphoedema bandaging system. British Journal of Oncology 2012;166(3):624-632. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22059933 (accessed 20 January 2016)
- ↑ 13.0 13.1 13.2 Doherty D, Morgan P, Moffatt C. Hosiery in lower limb lymphoedema. Journal of Lymphoedema 2009;4(1):30-37. Available from: http://www.journaloflymphoedema.com/ (accessed 15 January 2016).
- ↑ Linnitt N, Davies R. Fundamentals of compression in the management of lymphoedema. British Journal of Nursing 2007;16(10):588-592. Available from: http://www.ncbi.nlm.nih.gov/pubmed/17577161 (accessed 15 January 2016).
- ↑ Wigg J, Lee N. Managing lymphoedema and chronic oedema. Nursing and Residential Care 2015;17(4):192-197. Available from: http://www.magonlinelibrary.com/doi/10.12968/nrec.2015.17.4.192 (accessed 15 January 2016).
- ↑ 16.0 16.1 16.2 16.3 16.4 16.5 Nowicki J, Siviour A. Best Practice skin care management in lymphoedema. Wound Practice and Research 2013;21(2):61-65. Available from: http://www.awma.com.au/journal/2102_03.pdf (accessed 15 January 2016).
- ↑ James S. What are the perceived barriers that prevent patients with lymphoedema from continuing optimal skin care? Wound Practice and Research 2011;19(3):152-158. Available from: http://www.awma.com.au/journal/1903_09.pdf (accessed 15 January 2016)
- ↑ MacMillan Cancer Support. Cured – but at what cost? http://www.macmillan.org.uk/Documents/AboutUs/Newsroom/Consequences_of_Treatment_June2013.pdf (accessed 16 January 2016)
- ↑ NHS Choices. Benefits of Exercise. http://www.nhs.uk/Livewell/fitness/Pages/Whybeactive.aspx (accessed 16 January 2016)
- ↑ Irwin ML, Crumley D, McTieran A, Bernstein L, Baumgartner R, Gilliand F, Kriska A, Ballard-Barbash R. Physical Activity Levels before and after a Diagnosis of Breast Carcinoma, The Health, Eating, Activity and Lifestyle (HEAL) Study. Cancer 2003;97(7):1746-1757. Available from: http://www.ncbi.nlm.nih.gov/pubmed/12655532 (accessed 15 January 2016).
- ↑ Harrison S, Hayes SC, Newman B. Level of physical activity and characteristics associated with change following breast cancer diagnosis and treatment. Psycho-Oncology 2009;18:387-394. Available from: http://onlinelibrary.wiley.com/doi/10.1002/pon.1504/references (accessed 15 January 2016).
- ↑ Cheifetz O, Haley L. Management of secondary lymphoedema related breast cancer. Canadian Family Physician 2010;56:1277-1284. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21375063 (accessed 15 January 2016).
- ↑ 23.0 23.1 Cancer Research UK. Exercise, positioning and lymphoedema. http://www.cancerresearchuk.org/about-cancer/coping-with-cancer/coping-physically/lymphoedema/treating-lymphoedema/exercise-positioning (accessed 21 January 2016)
- ↑ McKenzie DC, Kalda AL. Effect of Upper Extremity Exercise on Secondary Lymphedema in Breast Cancer Patients: A Pilot Study. Journal of Clinical Oncology 2003;21(3):463-466. Available from: http://www.ncbi.nlm.nih.gov/pubmed/12560436 (accessed 15 January 2016).
- ↑ Hayes SC, Reul-Hirche H, Turner J. Exercise and Secondary Lymphedema: Safety, Potential Benefits, and Research Issues. Medicine and Science in Sports and Exercise 2009;483-489. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19117320 (accessed 15 January 2016).
- ↑ Schmitz KH, Ahmed RL, Troxel A, Cheville A, Smith R, Lewis-Grant L, Bryan CJ, Williams-Smith CT, Greene QP. Weight lifting in Women with Breast-Cancer-Related Lymphoedema. The New England Journal of Medicine 2009;361:664-673. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19675330 (accessed 15 January 2016).
- ↑ 27.0 27.1 Singh B, Disipio T, Peake J, Hayes SC. Systematic Review and Meta-Analysis of the Effects of Exercise for Those With Cancer-Related Lymphoedema. Archives of Physical Medicine and Rehabilitation 2015;1-30 Available from: http://www.ncbi.nlm.nih.gov/pubmed/26440777 (accessed 15 January 2016).
- ↑ 28.0 28.1 Kwan M, Cohn JC, Armer JM, Stewart BR, Corimer N. Exercise in patients with lymphedema: a systematic review of the contemporary literature. Journal of Cancer Survivorship 2011;5:320-336. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22002586 (accessed 15 January 2016).
- ↑ 29.0 29.1 Paramanandam VS, Roberts D. Weight training is not harmful for women with breast cancer-related lymphoedema: a systematic review. Journal of Physiotherapy 2014;60:136-143. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25086730 (accessed 15 January 2016).
- ↑ The Lymphoedema Support Network. Recreational Exercise With Lymphoedema. http://www.nhs.uk/ipgmedia/national/lymphoedema%20support%20network/assets/recreationalexercise(lsn).pdf (accessed 25 January 2016)
- ↑ 31.0 31.1 Williams A. Manual lymphatic drainage: exploring the history and evidence base. British Journal of Community Nursing 2010;18-24. Available from: http://www.magonlinelibrary.com/doi/abs/10.12968/bjcn.2010.15.Sup3.47365 (accessed 15 January 2016).
- ↑ 32.0 32.1 Pyke C. Massage: a helping hand for people with chronic oedema and lymphoedema. Clinical Focus 2010:28-30. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20559174 (accessed 15 January 2016).
- ↑ Williams AF, Vadgama A, Franks PJ, Mortimer PS. A randomised controlled crossover study of manual lymphatic drainage therapy in women with breast cancer-related lymphodema. European Journal of Cancer Care. 2002;11(4):254-261. Available from: http://www.ncbi.nlm.nih.gov/pubmed/12492462 (accessed 18 January 2015)
- ↑ Sitzia J, Sobrido L, Harlow W. Manual lymphatic drainage compared with simple lymphatic drainage in the treatment of post-mastectomy lymphoedema: A pilot randomised trial. Physiotherapy 2002; 88(2):99-107. Available from: http://www.sciencedirect.com/science/article/pii/S0031940605609339 (accessed 15 January 2016).
- ↑ Huang TW, Tseng SH, Lin CC, Bai CH, Chen CS, Hung CS, Wu CH, Tam KW. Effects of manual lymphatic drainage on breast cancer-related lymphedema: a systematic review and meta-analysis of randomised controlled trials. World Journal of Surgical Oncology 2013;11(15). Available from: http://www.ncbi.nlm.nih.gov/pubmed/23347817 (accessed 15 January 2016).
.</div>