Pain Neuroscience Education (PNE): Difference between revisions
Lynette Fox (talk | contribs) No edit summary |
No edit summary |
||
| Line 1: | Line 1: | ||
* What is Pain Neuroscience Education (PNE)? | |||
<br> | |||
*What does PNE consist of / involve? | |||
<br> | |||
*Rx to resolve? | |||
<br> | |||
*Indicators for the use of PNE | |||
Low Back Pain<br> <br>http://uconnmsi.uchc.edu/clinical_services/spine/back/index.html | |||
Low back pain (LBP) is currently considered to be the most common cause of disability and time off work in the over 45 age group, with it being reported that 84% people will experience LBP at some point during their life (Balagué et al., 2012). Whilst LBP is generally considered a self-limiting condition it can have severe implications to the patient’s psychological and physical health. Results from a UK survey, analysing the consultation prevalence for LBP showed that 417 per 10 000 registered patients sought medical help for their LBP, with the highest numbers being seen in the 45- 64 age group (536 per 10 000) (Jordan et al., 2010). Furthermore an Australian cohort study discovered whilst most patient’s recovered 1/3 had not fully recovered after 1 year (Henschke et al., 2008). LBP is clearly a substantial problem for both the health system and the socioeconomic environment, thus effective management is critical.<br>Updated NICE guidelines for Chronic LBP states that information and self-care advice should be provided to patients to promote self-management by fostering a positive attitude and providing realistic expectations to patients. However the type, duration, frequency and content of this advice was not reported on (NICE, 2015). | |||
<br>Jordan KP, Kadam UT, Hayward R, Porcheret M, Young C, Croft P. (2010). Annual consultation prevalence of regional musculoskeletal problems in primary care: an observational study. BMC Musculoskeletal disorders. 11 (144).<br>Balagué F, Mannion AF, Pellisé F, Cedraschi C. (2012). Non-specific low back pain. The Lancet. 4 (379), 482-91.<br>Henschke N, Maher CG, Refshauge KM, Herbert RD, Cumming RG, Bleasel J, York J, Das A, McAuley JH. (2008). Prognosis in patients with recent onset low back pain in Australian primary care: inception cohort study. BMJ. 337 (a171).<br>National Institute for Health and Clinical Excellence (2015) Back pain - low (without radiculopathy). Clinical Knowledge Summary. London: NICE. <br><br> | |||
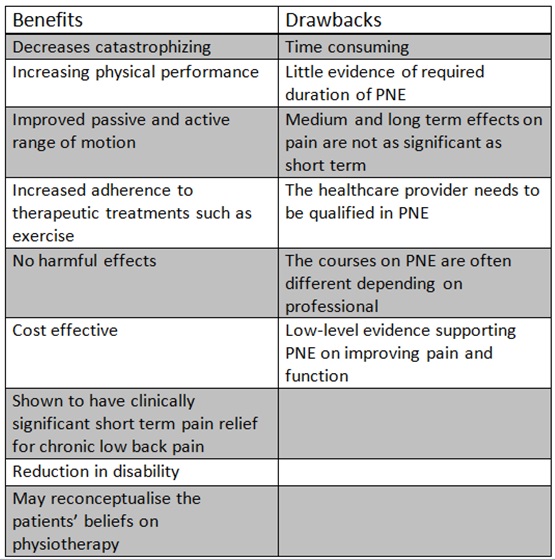
*The benefits and drawbacks of PNE | |||
[[Image:Benefits_and_drawbacks3.jpg]]<br> | |||
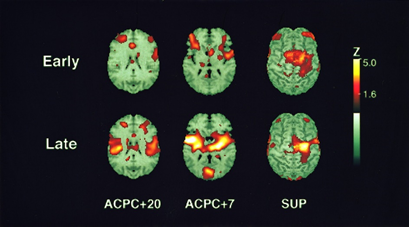
*Clinical imaging of benefits | |||
• Positron Emission Tomography (PET) | |||
[[Image:PET_scan_brain.png]] | |||
• Magnetic Resonance Spectroscopy (MRS) | |||
*<br> | |||
*Which patients groups it works best for | |||
<br> | |||
*Training / education of therapists to use it | |||
<br> | |||
*What is the history and where has it been developed from? | |||
<br> | |||
*Developed from theory of pain = tissue damage (cathartic) | |||
<br> | |||
*Brain scans of perceptions of LBP | |||
<br> | |||
*Section 1 – Scenarios to aid learning and clinical relevance: | |||
<br> | |||
*Becky’s Boss interviewed showing an experience of now chronic LBP that was managed by medication only | |||
<br> | |||
*Limited education given and ? low knowledge of pain mechanisms etc. | |||
<br> | |||
*Diagram of alarm systems (can be a hand drawn and in a simple video format with narration or just images with text) | |||
<br> | |||
*Interview (video or transcript) with Leanne @ NUH (to email 06/01/2016) | |||
<br> | |||
*Her experiences / beliefs | |||
<br> | |||
*What is PNE | |||
<br> | |||
*How does she use it? | |||
<br> | |||
*What are the outcomes like for her patients? | |||
<br> | |||
*Section 3 – Evidence | |||
#Paper 1 (with link) | |||
#Paper 2 (with link) | |||
#Paper 3 (with link) | |||
#Paper 4 (with link) | |||
#NICE Guidelines | |||
<br> | |||
*Comment and clinical bottom line of evidence collectively. | |||
<br> | |||
*Summary: | |||
<br> | |||
*Concise summary or key points of the page. | |||
<br> | |||
*Resources and useful links: | |||
#Podcasts | |||
#Youtube videos | |||
#Books | |||
#Research | |||
#Website | |||
<br> | |||
*Conclusion of entire page. | |||
<br> | |||
*Resources<br> | |||
*References:<br> | |||
Revision as of 16:27, 13 January 2016
- What is Pain Neuroscience Education (PNE)?
- What does PNE consist of / involve?
- Rx to resolve?
- Indicators for the use of PNE
Low Back Pain
http://uconnmsi.uchc.edu/clinical_services/spine/back/index.html
Low back pain (LBP) is currently considered to be the most common cause of disability and time off work in the over 45 age group, with it being reported that 84% people will experience LBP at some point during their life (Balagué et al., 2012). Whilst LBP is generally considered a self-limiting condition it can have severe implications to the patient’s psychological and physical health. Results from a UK survey, analysing the consultation prevalence for LBP showed that 417 per 10 000 registered patients sought medical help for their LBP, with the highest numbers being seen in the 45- 64 age group (536 per 10 000) (Jordan et al., 2010). Furthermore an Australian cohort study discovered whilst most patient’s recovered 1/3 had not fully recovered after 1 year (Henschke et al., 2008). LBP is clearly a substantial problem for both the health system and the socioeconomic environment, thus effective management is critical.
Updated NICE guidelines for Chronic LBP states that information and self-care advice should be provided to patients to promote self-management by fostering a positive attitude and providing realistic expectations to patients. However the type, duration, frequency and content of this advice was not reported on (NICE, 2015).
Jordan KP, Kadam UT, Hayward R, Porcheret M, Young C, Croft P. (2010). Annual consultation prevalence of regional musculoskeletal problems in primary care: an observational study. BMC Musculoskeletal disorders. 11 (144).
Balagué F, Mannion AF, Pellisé F, Cedraschi C. (2012). Non-specific low back pain. The Lancet. 4 (379), 482-91.
Henschke N, Maher CG, Refshauge KM, Herbert RD, Cumming RG, Bleasel J, York J, Das A, McAuley JH. (2008). Prognosis in patients with recent onset low back pain in Australian primary care: inception cohort study. BMJ. 337 (a171).
National Institute for Health and Clinical Excellence (2015) Back pain - low (without radiculopathy). Clinical Knowledge Summary. London: NICE.
- The benefits and drawbacks of PNE
- Clinical imaging of benefits
• Positron Emission Tomography (PET)
• Magnetic Resonance Spectroscopy (MRS)
- Which patients groups it works best for
- Training / education of therapists to use it
- What is the history and where has it been developed from?
- Developed from theory of pain = tissue damage (cathartic)
- Brain scans of perceptions of LBP
- Section 1 – Scenarios to aid learning and clinical relevance:
- Becky’s Boss interviewed showing an experience of now chronic LBP that was managed by medication only
- Limited education given and ? low knowledge of pain mechanisms etc.
- Diagram of alarm systems (can be a hand drawn and in a simple video format with narration or just images with text)
- Interview (video or transcript) with Leanne @ NUH (to email 06/01/2016)
- Her experiences / beliefs
- What is PNE
- How does she use it?
- What are the outcomes like for her patients?
- Section 3 – Evidence
- Paper 1 (with link)
- Paper 2 (with link)
- Paper 3 (with link)
- Paper 4 (with link)
- NICE Guidelines
- Comment and clinical bottom line of evidence collectively.
- Summary:
- Concise summary or key points of the page.
- Resources and useful links:
- Podcasts
- Youtube videos
- Books
- Research
- Website
- Conclusion of entire page.
- Resources
- References: