Oxalosis
Original Editors - Students from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Oscar Lewis, Shelby Kissel, Lucinda hampton, 127.0.0.1, Elaine Lonnemann, Tomer Yona, WikiSysop and Kim Jackson
Definition/Description[edit | edit source]
Oxalosis is a rare metabolic disorder in which the kidneys are unable to eliminate Calcium Oxalate Crystals through the urine. The excess crystals then collect in other parts of the body, accumulating first in the blood, then the eyes, bones, muscles, blood vessels, heart and other major organs. If untreated Oxalosis can lead to death.
Prevalence[edit | edit source]
add text here
Characteristics/Clinical Presentation[edit | edit source]
Oxalosis can present with a multitude of symptoms depending upon the severity and progression of the condition. Oxalate crystals can be formed in various bodily structures including the blood, eyes, bones, muscles, heart and other organs. Depending on where the excess accumulation of oxalate is located, patients are going to present differently. If excess oxalate accumulates in the bones, synovium, cartilage, or tendons, pain may present similarly to that of arthropathy (disease of a joint). When oxalate deposits in the synovium of joints, excessive inflammation can procure, often resembling arthralgias (joint pain). The most common joints often affected by systemic Ox
alosis are the proximal interphalangeal and metacarpophalangeal joints, knees, elbows and ankles. Excess oxalate crystals in the bones may also present as fractures, or just bone pain. Oxalosis affecting muscles could display as generalized aching or cramping of a muscle. A patient with Oxalosis can present with anemia or with skin ulcers. Due to the fact that the heart can be affected by Oxalosis and higher levels of calcium are circulating in the body, the function of the heart may be hindered. For instance patients with Oxalosis can present with cardiac arrhythmias or with cardiomyopathy. In some cases, oxalosis has been known to affect neural structures. When oxalate deposits around nerves, patients can report sensation abnormalities (tingling, numbness, shooting pain), as well as progressive strength deficits.
Hyperoxaluria, the primary cause of Oxalosis, may exhibit many different types of symptoms. Depending on the progression and severity, symptoms may first develop at birth or during adulthood. Although people will present differently depending upon the underlying mechanism for developing the condition, the first sign or symptom of Hyperoxaluria is often the presence of blood or pain during micturition. Other common symptoms that appear during the initial stages of the disease are an infection of the urinary tract or passing of a kidney stone. Although only reported in a minimal number of cases, the presence of the condition may first present as kidney failure. Also, others may not present with overwhelming symptoms initially and may be unaware until the third to fifth decades of life.
Associated Co-morbidities[edit | edit source]
add text here
Medications[edit | edit source]
Vitamins and minerals can help to reduce or prevent oxalate accumulation in the body. Vitamin B-6 can reduce oxalate excreted in the urine and oral preparations of phosphates and citrate can help prevent oxalate crystals from developing. Other medications (i.e thiazide diuretics) may be necessary contingent upon abnormalities in the urine .
For patients diagnosed with primary hyperoxaluria prescription doses of pyridoxine have been shown to decrease urine oxalate levels significantly in some cases. Urine oxalate levels in individuals on pyridoxine should be monitored monthly to assess individual patient responsiveness to this drug.
Symptoms due to oxalosis-induced oxalate arthritis have been shown to be alleviated through the utilization of NSAIDS, colchicine and steroids However, side effects have been noticed with the use of such medications. Some forms of these medications are not advised to use for certain patients, depending upon the primary cause and progression of the condition
Diagnostic Tests/Lab Tests/Lab Values[edit | edit source]
add text here
Etiology/Causes[edit | edit source]
Hyperoxaluria: Condition in which there is too much Oxalate in the urine. Excess oxalate can bind to calcium in the urine and cause kidney stones.
Primary Oxalosis:
- Primary Hyperoxaluria (PH): A rare, genetic disorder in which the liver can’t create the enzyme (or the enzyme doesn’t work properly) responsible for regulating the production of oxalate. An increase in the production of oxalate causes excessive amounts to be excreted in the urine. Oxalate can then combine with calcium in the urine and form salt or crystals that often results in lethal damage to the kidneys. The enzymes involved in this disorder are listed below.
- PH1: alanine-glyoxylate aminotransferase, or AGT
- PH2: glyoxylate/hydroxypyruvate reductase, or GR/H
- PH3: 4-hydroxy-2-oxoglutarate aldolase, or HOGA Hyperoxaluria
Secondary Oxalosis:
- Dietary Hyperoxaluria: Consuming foods high in oxalate content can increase levels of oxalate in the urine and increase the risk of kidney stones. Foods High in Oxalate
- Enteric Hyperoxaluria: Certain intestinal diseases (Crohn's_Disease and Short Bowel Syndrome) can cause an increase in absorption of oxalate from foods therefore increasing the oxalate excreted in the urine.
- Kidney failure due to reasons other than Hyperoxaluria in which oxalate can no longer be excreted from the body.
Systemic Involvement[edit | edit source]
Once the kidneys are no longer able to keep up with excreting oxalate, the crystals begin to accumulate in the blood. Once the oxalate crystals begin circulating in the blood stream, they are free to deposit into other structures of the body. Due to the vast structures that can be affected by oxalosis, the disease can become fatal when accumulation becomes excessive. Structures commonly affected by the disease are listed in the definition and clinical presentation sections above.
Medical Management (current best evidence)[edit | edit source]
Treatment will depend on the type, symptoms and severity of hyperoxaluria and how well you respond to treatment.
Reducing oxalate
- Medications: View Medications section above.
- High fluid intake: If kidney function has not been impaired, increasing your fluid intake will help to flush the kidneys, stop oxalate build up and prevent kidney stones.
- Dietary changes: If increased accumulation of oxalate is due to dietary causes, then changes in diet can be effective in decreasing the amount of oxalate excreted in the urine. Limiting and/or eliminating foods high in oxalate from the diet may be recommended by your doctor.
Kidney stone management:
Calcium Oxalate kidney stones occur commonly with hyperoxaluria, but do not always require treatment. If treatment is deemed necessary there are several minimally invasive options to eliminate kidney stones.
- Shock Wave Lithotripsy: A procedure completed by a urologist in which a lithotripter is used to break the kidney stone into small pieces
- Ureteroscopy: A procedure in which a ureteroscope is used to find and remove the stone or break up the stone with laser energy. Also performed by a urologist.
- Percutaneous Nephrolithotomy: A procedure in which a small incision is made in the patient’s back, and a nephroscope is used by the urologist to find and retrieve the stone.
All of the procedures listed above a performed under anesthesia and may or may not require a several day hospital stay.
Dialysis
Dialysis is a treatment that is used to compensate for kidney failure caused by Hyperoxaluria. It imitates kidney function by removing extra fluids and toxins from the blood. Dialysis is only a temporary solution while awaiting a kidney transplant because it cannot eliminate oxalate that accumulates elsewhere in the body and eventually oxalosis will result.
- Hemodialysis: A procedure that involves removing blood from the body and into a dialyzer that filters the blood to remove toxins. The newly cleansed blood is then returned to the body. This process takes 3-5 hours and is performed at least 3 times per week.
- Peritoneal Dialysis: A procedure that cleans your blood without removing it from your body. A sterile cleansing fluid called dialysate is inserted into the abdomen through a catheter. This solution helps to draw out waste and toxins that then drain in a collection bag outside the body. These treatments can be done at home or elsewhere.
Organ Transplant
Once the kidney fails a transplant may be needed. Based on the type and progression of the disease process a kidney transplant or kidney and liver transplant based on individual disease presentation may be required.
Physical Therapy Management (current best evidence)[edit | edit source]
Physical therapy is currently not recognized as a primary method of treatment for oxalosis. Current management of the condition is listed in sections above. However, physical therapy treatment may be indicated to address the functional limitations and impairments that a patient develops from excessive oxalate accumulation. As mentioned above, oxalosis may lead to excessive skeletal oxalate accumulation. If profound, these affected skeletal structures may be prone to fractures and demineralization. Physical therapy treatment would be needed to rehabilitate patients post surgical correction. For patients who suffer from oxalate arthritis, symptoms such as pain quite possibly may disappear once the cause of the oxalate production are addressed. However, some patients who are apprehensive to movement displaying reduced range of motion and strength deficits, would benefit from physical therapy to address such limitations. Besides addressing range of motion and strength, physical therapy treatment may focus on joint protection strategies, as well as energy conservation techniques. All other movement based dysfunctions that are the direct result of oxalosis, can be addressed through evidence based physical therapy treatment, as long as the cause of the primary condition is corrected.
Differential Diagnosis[edit | edit source]
- Arthralgias
- Osteoarthritis
- Rheumatoid_Arthritis
- Gout
- Bursitis
- Tenosynovitis
- Synovitis
- Spinal_Stenosis
- Myopathies
- Polyradiculoneuropathy
- Cardiac Abnormalities (arrhythmias, valvular abnormalities)
- Cardiopulmonary (palpitations, syncope, dyspnea)
- Gastrointestinal Disorders
- Hyperparathyroidism
Case Reports/ Case Studies[edit | edit source]
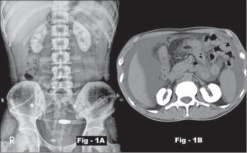
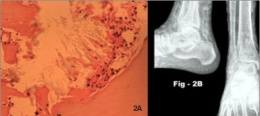
Horta-Baas G, Vargas-Gutiérrez C, Barile-Fabris L. Large Joint Destructive Arthropathy and Tumoral Calcinosis Associated to Primary Oxalosis: Case Report and Literature Review. Reumatologia Clinica [serial online]. May 2013;9(3):181-185. Available from: Academic Search Complete, Ipswich, MA. Accessed March 31, 2016.
Stepien K, Prinsloo P, Hitch T, McCulloch T, Sims R. Acute Renal Failure,Microangiopathic Haemolytic Anemia, and Secondary Oxalosis in a Young Female Patient. International Journal Of Nephrology [serial online]. January 2011;:1-5. Available from: Academic Search Complete, Ipswich, MA. Accessed March 31, 2016.
www.hindawi.com/journals/ijn/2011/679160/
Resources
[edit | edit source]
Mayo Clinic Hyperoxaluria Center:
Phone: 1-800-270-4637
Email: [email protected]
For additional information on the disease and the Hyperoxaluria Center:
Website:nephrology-rst/hyperoxaluriacenter.html
Facebook page: Primary Hyperoxaluria Disease-Mayo Clinic: Contains information and tips about kidney stones, kidney stone prevention and management, and hyperoxaluria, and notifications about upcoming meetings and conferences.
The Rare Kidney Stone Consortium: www.rarekidneystones.org
The Oxalosis and Hyperoxaluria Foundation: www.ohf.org
Recent Related Research (from Pubmed)[edit | edit source]
Failed to load RSS feed from http://www.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1-7FJ7kkHKrHcV3UxD_eVNjQTOMXES5Q2zdbBN8FacD9NT7YKI|charset=UTF-8|short|max=10: Error parsing XML for RSS
References[edit | edit source]
see adding references tutorial.