Overview of Cervical Spine Assessment: Difference between revisions
m (Add references to outcome measures) |
m (Add image from IFROMPT guidelines for physical examination) |
||
| Line 117: | Line 117: | ||
Symptoms of vertebral insufficiency include dizziness/vertigo, nausea/vomiting, inability to stand, blurred vision/diplopia, headache, facial parasthaesia/facial palsy/difficulty swallowing.<ref name=":1">Rushton A, Carlesso LC, Flynn T, Hing WA, Rubinstein SM, Vogel S, et al. International Framework for examination of the cervical region for potential of vascular pathologies of the neck prior to musculoskeletal intervention: International IFOMPT cervical framework. Journal of Orthopaedic &amp; Sports Physical Therapy. 2023;53(1):7–22. doi:10.2519/jospt.2022.11147</ref> | Symptoms of vertebral insufficiency include dizziness/vertigo, nausea/vomiting, inability to stand, blurred vision/diplopia, headache, facial parasthaesia/facial palsy/difficulty swallowing.<ref name=":1">Rushton A, Carlesso LC, Flynn T, Hing WA, Rubinstein SM, Vogel S, et al. International Framework for examination of the cervical region for potential of vascular pathologies of the neck prior to musculoskeletal intervention: International IFOMPT cervical framework. Journal of Orthopaedic &amp; Sports Physical Therapy. 2023;53(1):7–22. doi:10.2519/jospt.2022.11147</ref> | ||
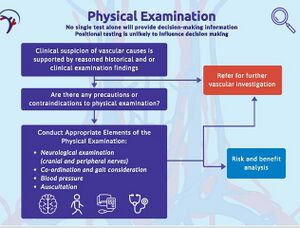
Following a thorough subjective assessment of the cervical spine, careful planning of the physical examination should be done together with consideration of any precautions and contraindications related to further examination of vertebral insufficiency. In addition to this the clinician should also reflect on their ability to perform certain tests and seek additional training if needed.<ref name=":1" /> | Following a thorough subjective assessment of the cervical spine, careful planning of the physical examination should be done together with consideration of any precautions and contraindications related to further examination of vertebral insufficiency. | ||
[[File:International Framework for Examination of the Cervical Region for Potential of Vascular Pathologies of the Neck Prior to Musculoskeletal Intervention International IFOMPT Cervical Framework Fig 5.jpeg|center|thumb|International Framework for Examination of the Cervical Region for Potential of Vascular Pathologies of the Neck Prior to Musculoskeletal Intervention International IFOMPT Cervical Framework - Physical Examination]] | |||
In addition to this the clinician should also reflect on their ability to perform certain tests and seek additional training if needed.<ref name=":1" /> | |||
The following tests can be included for the assessment of vertebral artery insufficiency:<ref>Cunningham, S. An Overview of Cervical Spine Assessment. Course. Plus. 2023.</ref> | The following tests can be included for the assessment of vertebral artery insufficiency:<ref>Cunningham, S. An Overview of Cervical Spine Assessment. Course. Plus. 2023.</ref> | ||
Revision as of 00:43, 28 November 2023
Top Contributors - Jacquie Kieck, Jess Bell and Kim Jackson
Introduction[edit | edit source]
A thorough assessment is vital for the effective management of any condition. The cervical spine is no different. In this course Shala Cunningham gives a step-by-step overview of the vital elements of a thorough assessment of the cervical spine. The assessment should broadly consist of a subjective assessment (history taking) and an objective assessment (observation and tests). A thorough assessment allows the clinician to classify the client's presentation. A classification system is discussed to guide the clinician for the successful management of the client's presentation.
Subjective Assessment[edit | edit source]
History[edit | edit source]
In this course the instructor suggests using the mnemonic L-M-N-O-P-Q-R-S-T to cover all the aspects of the history taking in the subjective assessment.
L: Location of symptoms and level of functional impairment
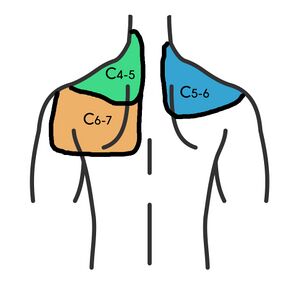
This table gives a summary of the likely source of symptoms based on the area of symptoms.
| Area of Symptoms | Possible Source of Symptoms |
|---|---|
| Head / occipital region | Upper cervical spine |
| Localised pain without radiation / referral |
|
| Radiating pain | Nerve root irritation |
M: Medical factors (medications) and mechanism of injury
In the assessment, be specific in finding out when and how the injury occurred, what forces were applied, and the position of the head at the time of the trauma. Also ask about neurological symptoms with the trauma. Red flags related to the mechanism of injury would be sudden onset of severe pain in the absence of an incident or accident.
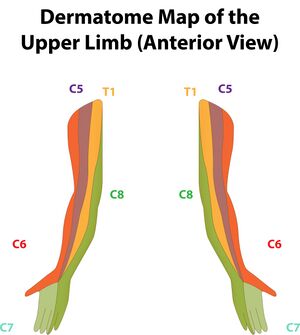
N: Neurological symptoms
Establish if there are symptoms of numbness, tingling, burning or electrifying. Be specific about the location of these symptoms i.e. is the distribution of these symptoms dermatomal? The clinician should also note if the symptoms are constant or intermittent, and if they are associated with the position of the head.
O: Occupation including limitations
P: Palliating and provocating symptoms
Establish what increases and decreases the symptoms. Also note how long it takes the symptoms to calm down once aggravated. A red flag would be constant/unrelenting pain independent of position or activity.
Q: Quality of symptoms/pain
This would cover the description of the symptoms for example, sharp, dull, stabbing, aching or electric/shock-like description of symptoms.
R: Radiation of symptoms
Be specific about where the symptoms radiate to, how long do the radiating symptoms last, and are they constant or position/activity related. A red flag would be if the radiating symptoms cover multiple dermatomes.
S: Severity of symptoms
Note how the symptoms impact function and activity.
T: Timing of symptoms
Ask about the sequence and progression of symptoms. Red flags would be if pain is interrupting sleep, or constant/unrelenting pain.
Be sure to inclde questions about age, past history of neck pain, constitutional symptoms, dizziness, drop attacks and vertigo, parasthesia, numbness, weakness, or stiffness.
Red Flags[edit | edit source]
Red flags are symptoms that suggest the presence serious pathology. International guidelines recommend using red flags to identify serious pathology[1]. Below are a list of red flags to screen for when assessing the cervical spine:
- Severe loss of range of motion (ROM) with sudden onset of symptoms
- Changes in balance/ gait
- Hypo/ hyper reflexia
- Constant pain
- Severe radiating pain
- Moderate to severe occipital headache
- Facial pain
- Psychological changes
- Cranial nerve symptoms
- Dizziness
- Horner syndrome
- Hemiparaesthesia
- Bowel and bladder change
- Ataxia
- Nystagmus
- Drop attacks
- Hemifacial parathaesia
- Dysphagia
The History Can Be Suggestive of Certain Conditions[edit | edit source]
History Suggesting Cervical Spondylosis[edit | edit source]
A history suggestive of cervical spondylosis would include a person over the age of 45 years with gradual, slow onset of symptoms (no specific incident). The pain is usually unilateral and radiates in a facet joint referral pattern. Pain usually increases with extension ('closing down' of the joint) and reduces with flexion ('opening' of the joint). The most commonly affected levels of the cervical spine are C5,C6, C7.
History Suggesting Disc Involvement[edit | edit source]
A history suggestive of cervical disc involvement would include a person under the age of 60 years, with sudden onset of symptoms (no specific incident). The pain is usually unilateral and radiates in a dermatomal referral pattern. Pain usually increases with flexion. The most commonly affected levels of the cervical spine are C5,C6.
Outcome Measures[edit | edit source]
Useful outcome measures in the assessment of the cervical spine:
- Neck Disability Index (NDI)[2]
- Patient Specific Functional Scale (PSFS)
- Fear-Avoidance Belief Questionnaire (FABQ)[3]
- Numeric Pain Rating Scale (NPRS)[2]
Objective Assessment[edit | edit source]
Observation[edit | edit source]
General observation of the posture, including the position of the head, neck, and shoulders should be done. Also observe for any signs of torticollis.
Instability Testing[edit | edit source]
The Sharp-Purser test is used to test the integrity of the transverse ligament, however there are concerns about the reliability, validity and safety of the test.[4]
Vertebral Artery Testing[edit | edit source]
Symptoms of vertebral insufficiency include dizziness/vertigo, nausea/vomiting, inability to stand, blurred vision/diplopia, headache, facial parasthaesia/facial palsy/difficulty swallowing.[5]
Following a thorough subjective assessment of the cervical spine, careful planning of the physical examination should be done together with consideration of any precautions and contraindications related to further examination of vertebral insufficiency.
In addition to this the clinician should also reflect on their ability to perform certain tests and seek additional training if needed.[5]
The following tests can be included for the assessment of vertebral artery insufficiency:[6]
- Hautant test
- Cervical quadrant test
- Pre-manipulative position test
Resources[edit | edit source]
- bulleted list
- x
or
- numbered list
- x
References[edit | edit source]
- ↑ Childs, J.D., Cleland, J.A., Elliott, J.M., Teyhen, D.S., Wainner, R.S., Whitman, J.M., Sopky, B.J., Godges, J.J., Flynn, T.W., Delitto, A. and Dyriw, G.M., 2008. Neck pain: clinical practice guidelines linked to the International Classification of Functioning, Disability, and Health from the Orthopaedic Section of the American Physical Therapy Association. Journal of Orthopaedic & Sports Physical Therapy, 38(9), pp.A1-A34.
- ↑ 2.0 2.1 Cleland JA, Childs JD, Whitman JM. Psychometric Properties of the neck disability index and numeric pain rating scale in patients with mechanical neck pain. Archives of Physical Medicine and Rehabilitation. 2008;89(1):69–74. doi:10.1016/j.apmr.2007.08.126
- ↑ Waddell G, Newton M, Henderson I, Somerville D, Main CJ. A fear-avoidance beliefs questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain. 1993;52(2):157–68. doi:10.1016/0304-3959(93)90127-b
- ↑ Mansfield CJ, Domnisch C, Iglar L, Boucher L, Onate J, Briggs M. Systematic review of the diagnostic accuracy, reliability, and safety of the sharp-purser test. Journal of Manual & Manipulative Therapy. 2019;28(2):72–81. doi:10.1080/10669817.2019.1667045
- ↑ 5.0 5.1 Rushton A, Carlesso LC, Flynn T, Hing WA, Rubinstein SM, Vogel S, et al. International Framework for examination of the cervical region for potential of vascular pathologies of the neck prior to musculoskeletal intervention: International IFOMPT cervical framework. Journal of Orthopaedic & Sports Physical Therapy. 2023;53(1):7–22. doi:10.2519/jospt.2022.11147
- ↑ Cunningham, S. An Overview of Cervical Spine Assessment. Course. Plus. 2023.