Myocardial Infarction
Original Editors - Jessica King & Melissa Tuemler from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Lead Editors - Your name will be added here if you are a lead editor on this page. Read more.
Definition/Description
[edit | edit source]
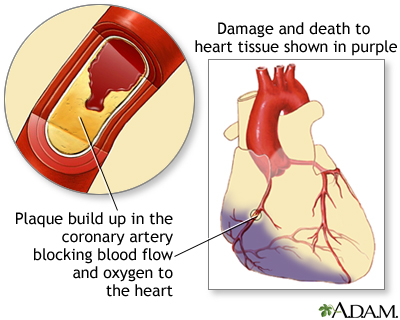
A Myocardial Infarction (MI) occurs when an area of the heart does not receive enough blood flow and is subsequently damaged or dies. An MI is commonly referred to as a heart attack and is always a medical emergency. Many times an MI occurs when one of the main arteries to the heart, specifically the coronary arteries, become blocked due a build up of plaque. Plaque build up occurs when cholesterol and other large cells attach to the arterial walls, and cause narrowing of the arterial canals. When the arteries becomes increasingly narrow due to plaque build up there is no longer adequate blood and oxygen control to the heart, and an MI occurs. Often times an MI can occur suddenly, and without warning signs. Some identified causes of an MI include sudden physical exertion, recent illness, and emotional stress.
Prevalence[edit | edit source]
Myocardial Infarctions are the leading cause of death in the industrialized nations of the world. In the United States, there are about 450,000 deaths due to MIs each year. Now 95% of patients hospitalized with an MI will survive due to improvements in emergency response time, and treatment techniques. The risk of having an MI increases with age, but 50% of MIs in the United States occur in people under the age of 65 years old.[1]
Characteristics/Clinical Presentation[edit | edit source]
According the American Heart Association (AHA), heart attacks can occur in a variety of fashions. Some begin suddenly with severe pain or other symptoms, while others have a slower onset with only mild pain or discomfort. Pain toward the center of the chest is the most common symptom experienced by patients. This pain is typically uncomfortable and resembles the feeling of squeezing or a pressure on the anterior chest. Patient's experiencing a MI may also experience pain in the jaw, shoulder, arms, stomach, neck, or back. The other common signs and symptoms of heart attack are listed below. [2]
Signs and symptoms of MI include:
- Chest pain lasting longer than a few minutes
- Anxiety
- Cough
- Fainting
- Lightheadedness/ Dizziness
- Nausea/ Vomiting
- Heart palpitations
- Shortness of air (SOA)
- Sweating
MI can also be "silent" in which there are no symptoms.
[3][edit | edit source]
Signs and symptoms vary based on gender. The most common symptom experienced by both genders is chest pain or discomfort. Women typically experience other symptoms such as SOA, nausea and vomiting, and nack or jaw pain.
[2][edit | edit source]
Associated Co-morbidities[edit | edit source]
Associated Co-morbidities for Myocardial Infarction include:
Hypertension
Coronary Artery Disease (CAD)
Congestive Heart Failure (CHF)
Arthritis
Diabetes
Medications[edit | edit source]
Following a MI, patients will most likely be prescribed some form of medication for the rest of their lives.
|
Anticoagulants (Warfarin) |
Blood thinner. Decreases clotting ability of the blood, but do not dissolve existing clots. |
| Antiplatelet agents (Aspirin) |
Keeps blood clots from forming by preventing blood platelets from sticking together. |
| ACE inhibitors (Benazepril, Captopril, Enalapril) |
Expands blood vessels and decreases resistance by lowering levels of angiotensin II. Allows blood to flow more easily and makes the heart's work easier or more efficient. |
| Angiotension II Receptor Blockers (Candesartan) |
Prevent angiotension II from having any effects on the heart and blood vessels. This keeps blood pressure from rising. |
| Beta Blockers (Acebutolol) |
Decreases the heart rate and cardiac output, which lowers blood pressure and makes the heart beat more slowly and with less force. |
| Calcium Channel Blockers (Amlodipine) |
Interrupts the movement of calcium into the cells of the heart and blood vessels. May decrease the heart's pumping strength and relax blood vessels. |
| Diuretics (Amiloride) |
Causes the body to rid itself of excess fluids and sodium through urination. Helps to relieve the heart's workload. Also decreases the buildup of fluid in the lungs and other parts of the body, such as the ankles and legs. Different diuretics remove fluid at varied rates and through different methods. |
| Vasodilators (Nitrates) |
Relaxes blood vessels and increases the supply of blood and oxygen to the heart while reducing its workload. Can come in pills to be swallowed, chewable tablets and as a topical application (cream). |
| Digitalis Preparations (Lanoxin) |
Increases the force of the heart's contractions, which can be beneficial in heart failure and for irregular heartbeats. |
| Statins |
Various medications can lower blood cholesterol levels. They may be prescribed individually or in combination with other drugs. They work in the body in different ways. Some affect the liver, some work in the intestines and some interrupt the formation of cholesterol from circulating in the blood. |
Diagnostic Tests/Lab Tests/Lab Values[edit | edit source]
The diagnosis of a heart attack can be completed with the following assessment tools:
1. Complete patient medical history
2. Physical exam
3. EKG
4. Blood testing to be sure there are no abnormal levels of enzymes in the blood
Diagnostic tests for determining if a patient has had an MI can be invasive or non-invasive.
Non-invasive tests:
1. EKG: records the electrical activity of the heart.
2. Ambulatory EKG and Holter Monitoring: records electrical activity of the heart during ADL’s.
3. Chest X-ray: photograph of the heart and lungs that helps determine if the heart is enlarged or if fluid is accumulating in the lungs.
4. Echocardiogram: hand held device placed over the chest that uses ultrasound to produce images of the heart.
5. CT or MRI
6. Exercise Stress Test: monitor with electrodes that are attached to chest and monitor the heart response while an individual walks on a treadmill.
Invasive tests:
1. Blood Tests: may include cardiac enzymes such as troponin and creatine kinase, C-reactive protein, fibrinogen, lipoproteins, triglycerides, BNP, and prothrombin
2. Cardiac Catheterization: examines the inside of the heart and blood vessels using an angiogram and dye. This can measure the blood pressure in side the heart, detect where a narrowing in the vessel is located, and evaluates overall heart function.
== [5] ==
Etiology/Causes[edit | edit source]
Heart disease has many risk factors, some that can be changed and others that cannot.
Risk factors that cannot be changed include:
- Age (Increased risk after age 65)
- Gender (Males at increased risk)
- Race/ethnicity (African Americans, Mexican Americans, American Indians, Hawaiians and Asian Americans at increased risk)
- Genetics/ Family History
Risk factors that can be changed:
- Smoking
- High cholesterol (diet, exercise, and medication)
- High blood pressure (diet, exercise, and medication)
- DM management
- Exercising at least 30 min/day
- Eating a healthy, nutritious diet
- Stress management
- Limiting alcohol consumption to 1 drink/day for women and 2 drinks/day for men
Systemic Involvement[edit | edit source]
Cardiovascular:
Damage to the heart can lead to some serious effects on the cardiovascular system including decreased peripheral blood flow, dangerous heart arrhythmias, congestive heart failure, and an increased risk for another MI.
Pulmonary:
The pulmonary system is also affected by an MI because there is a decrease level of oxygen saturation due to the damaged heart. Often times during an MI fluid can accumulate in the lungs which could result in damage or infection.
Endocrine:
Many times during an MI the insulin levels spike in individuals, even if they do not have diabetes. Treatment to control the increase in insulin is often required.
Medical Management (current best evidence)[edit | edit source]
| Tests | Surgeries | Implanted Medical Devices |
|---|---|---|
| Angioplasty | Left Ventricular Assist Device | |
| Artificial Heart Valve Surgery | Pacemaker | |
| Atheroectomy | Implantable Cardioverter Defibrillator | |
| Bypass Surgery | ||
| Cardiomyoplasty | ||
| Heart Transplant | ||
| Radiofrequency Ablation | ||
| Stent Placement | ||
| Transmyocardial Revascularization |
Tests
Surgeries
Implanted Medical Devices
- Left Ventricular Assist Device: battery operated, mechanical pump device that is surgerically implanted into the heart and is used to maintain the pumping ability of a heart that can't effectively work on its own. This device is typically implanted in patients who are on the waiting list for a heart transplant or suffering from end-stage heart failure.
- Pacemaker: device implanted into heart tissue that sends electrical impulses to help maintain a regular heart beat. This device is typically used when the hearts "natural pacemaker" becomes defective and causes the heart to beat at an irregular beat.
- Implantable Cardioverter Defibrillator:
Physical Therapy Management (current best evidence)[edit | edit source]
add text here
Alternative/Holistic Management (current best evidence)[edit | edit source]
add text here
Differential Diagnosis[edit | edit source]
add text here
Case Reports/ Case Studies[edit | edit source]
add links to case studies here (case studies should be added on new pages using the case study template)
Resources
[edit | edit source]
add appropriate resources here
Recent Related Research (from Pubmed)[edit | edit source]
see tutorial on Adding PubMed Feed
Failed to load RSS feed from http://www.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1RUQ50_F_fllPsjZ1eMyrz9qhwE-OPc8GgPzCFjLATMJPP15z-|charset=UTF-8|short|max=10: Error parsing XML for RSS
References[edit | edit source]
see adding references tutorial.
- ↑ Cleveland Clinic. Acute Myocardial Infarction. http://www.clevelandclinicmeded.com/medicalpubs/diseasemanagement/cardiology/acute-myocardial-infarction/#s0015 (12 Feb 2013)
- ↑ 2.0 2.1 American Heart Association. Warning signs of a Heart Attack. http://www.heart.org/HEARTORG/Conditions/HeartAttack/WarningSignsofaHeartAttack/Warning-Signs-of-a-Heart-Attack_UCM_002039_Article.jsp (accessed 10 Feb 2013).
- ↑ MedlinePlus. Heart Attack. http://www.nlm.nih.gov/medlineplus/ency/article/000195.htm (accessed 10 Feb 2013).
- ↑ American Heart Association. Cardiac Medications. http://www.heart.org/HEARTORG/Conditions/HeartAttack/PreventionTreatmentofHeartAttack/Cardiac-Medications_UCM_303937_Article.jsp (accessed 11 Feb 2013).
- ↑ American Heart Association. Symptoms and Diagnosis of Heart Attack. http://www.heart.org/HEARTORG/Conditions/HeartAttack/SymptomsDiagnosisofHeartAttack/Symptoms-and-Diagnosis-of-Heart-Attack_UCM_002041_Article.jsp (accessed 10 Feb 2013).