Multiple System Atrophy: A Case Study
Client Characteristics[edit | edit source]
Mr. L is a 62-year-old retired NASA astronaut. He is currently living in California with his husband of 20 years, who is also retired. Mr. L first presented to his family physician three years ago with issues of erectile dysfunction, in which his doctor believed to be result of aging. Over the next year, Mr. L began developing other symptoms seemingly unrelated to his previous health history. He presented with noted difficulty balancing, asymmetric postural tremor (right side), bradykinesia, rigidity, urinary incontinence, and minor slurring of speech – warranting a probable diagnosis of Parkinson’s disease. Mr. L was prescribed oral Levodopa (250 milligrams, four times a day). This medication eased his symptoms for four months, but gradually, he began noticing the return of his symptoms – warranting a reassessment. Despite increasing his medication dosage, Mr. L’s chief complaints were perpetuated. Additionally, he began experiencing gait ataxia with cerebellar dysarthria, action myoclonus, and cold hands and feet. After conducting a thorough physical assessment, it was noted that Mr. L presents with orthostatic hypertension (dropping from 120/94 mmHg in a recumbent position, to 90/68 mmHg, after prolonged standing). Based on the presenting factors, a diagnosis of Multiple System Atrophy-Parkinsonism (MSA-P) was established. The physician referred Mr. L to physiotherapy for gait and mobility training, pelvic floor training, and education on symptom management.
Examination Findings[edit | edit source]
Subjective[edit | edit source]
| Patient Profile | 62 y/o male |
| History of Present Illness | Diagnosis of probable MSA-P three weeks ago, right-sided postural tremor, difficulty balancing, bradykinesia, rigidity, urinary incontinence, slurred speech, cerebellar dysarthria, cold hands and feet, action myoclonus, and orthostatic hypotension. |
| Past Medical History | N/A |
| Medications |
|
| Health Habits | Non-smoker, non-drinker, formerly very active (prior to symptom onset) |
| Family Health History | No family history of progressive neurological disorders |
| Psychosocial | Patient is experiencing marital issues due to the progressive nature of the disease. Patient also expresses concerns of loneliness, isolation, and depression due to fatality of the diagnosis. Mr. L also worries about burdening his partner and family as the disease progresses and he becomes less independent. Having been previously very active, Mr. L is having trouble coping with his new sedentary lifestyle. Previously, Mr. L volunteered weekly at his local YMCA, running a space exploration program for young children – bringing joy to his life. Due to cerebellar dysarthria, he is having trouble effectively communicating with others. Lastly, he used to really enjoy dancing with his husband but has not been able to do so recently because of his condition. |
| Living Environment | Two-story home with 14 stairs to the second floor. Bedroom located on second floor. Half bathroom on first floor, full bathroom on second floor. Second floor bathroom equipped with a spacious walk-in shower. Hardwood flooring throughout the home. |
| Functional History | Prior to probable MSA-P diagnosis: very active, running 15km a week and walking everywhere within the city. Drove when needed. Able to independently maintain his property and home chores. Able to complete all activities of daily living independently. |
| Current Functional Status | After probable MSA-P diagnosis: able to ambulate 200m independently, but very slowly and unsteadily. Beyond 200m, requires a rollator walker or assist X1. Requires assistance from his husband for ADLs (cooking, cleaning, bathing, shopping, etc.). Trouble controlling urination and bowel movements (requires protective underwear). Able to ascend and descend one flight of stairs with assist X1. Unable to drive. Fine motor activity is limited due to action myoclonus (unable to type). Trouble communicating due to dysarthria. |
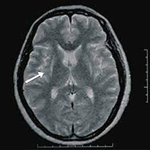
| Imaging | MRI
T2 weighted MRI revealed a hyperintense putaminal slit sign bilaterally |
| Precautions/Contraindications | Depression, lack of social interaction (decreased involvement with community), and trouble communicating due to dysarthria (no difficulties with comprehension). Otherwise, no contraindications to a physiotherapy program. |
Objective[edit | edit source]
| General | Minor hypomimia, postural AP tremor, action tremor | ||||||||||||||||||||||||||||||||
| Posture | Standing
Rounded shoulders, right shoulder depression, forward head posture, forward lean, wide base stance | ||||||||||||||||||||||||||||||||
| Seated
Rounded shoulders, right shoulder depression, posterior pelvic tilt | |||||||||||||||||||||||||||||||||
| Gait | Festination, shuffling (short stride) wide base gait, bradykinetic ambulation, reduced arm swing bilaterally, action myoclonus more prominent during ambulation | ||||||||||||||||||||||||||||||||
| Tone | High tone on right side of body in comparison to the left | ||||||||||||||||||||||||||||||||
| AROM | Upper Extremity
| ||||||||||||||||||||||||||||||||
Trunk
| |||||||||||||||||||||||||||||||||
Lower Extremity
| |||||||||||||||||||||||||||||||||
| PROM | PROM limited by muscle rigidity and contracture | ||||||||||||||||||||||||||||||||
| Strength | Respiratory
| ||||||||||||||||||||||||||||||||
| Musculoskeletal
Manual muscle testing revealed global muscle weakness (4/5) | |||||||||||||||||||||||||||||||||
| Sensation | WNL | ||||||||||||||||||||||||||||||||
| Neurological Testing | Upper Motor Neuron Testing
| ||||||||||||||||||||||||||||||||
Lower Motor Neuron Testing
| |||||||||||||||||||||||||||||||||
Myotomes and Dermatomes
| |||||||||||||||||||||||||||||||||
| Self Reported Outcome Measures | Activities-Specific Balance Confidence Scale (ABC) – assesses balance (vestibular and non-vestibular, functional mobility)
| ||||||||||||||||||||||||||||||||
Short Form – 36 (SF36) - general assessment of overall health function and psychosocial quality of life
| |||||||||||||||||||||||||||||||||
| Outcome Measures | Unified Multiple System Atrophy Rating Scale (UMSARS)
| ||||||||||||||||||||||||||||||||
TUG
| |||||||||||||||||||||||||||||||||
Performance-Oriented Mobility Assessment (POMA)
| |||||||||||||||||||||||||||||||||
Functional Reach
| |||||||||||||||||||||||||||||||||
Single Limb Stance (SLS)
|