Multiple System Atrophy: A Case Study: Difference between revisions
No edit summary |
No edit summary |
||
| Line 9: | Line 9: | ||
This case study follows Mr. L through his rehabilitation journey, from initial assessment to current therapeutic interventions. These interventions include patient education, resistance training, range of motion exercises, balance and gait functional training, pelvic floor training, and dance therapy. | This case study follows Mr. L through his rehabilitation journey, from initial assessment to current therapeutic interventions. These interventions include patient education, resistance training, range of motion exercises, balance and gait functional training, pelvic floor training, and dance therapy. | ||
{{#ev: | {{#ev:youtube|mVqiCgaLSf4}} | ||
== CLIENT CHARACTERISTICS == | == CLIENT CHARACTERISTICS == | ||
Revision as of 02:45, 12 May 2021
ABSTRACT[edit | edit source]
This fictional case study involves an older adult male who is diagnosed with Multi System Atrophy-Parkinsonism (MSA-P), which is classified as probable. The purpose of this case study is to outline what the neurological disease MSA-P is, including its natural disease course, progressive nature, clinical presentation, as well as the difficulty of distinguishing it from its differential diagnoses (i.e. Parkinson’s Disease). Additionally, the intention was to highlight the impact that the disease had, not only on Mr. L’s physical state, but the impact on his personal relationships, and his mental health.
Mr. L first presented 3 years prior with erectile dysfunction and progressed to additional symptoms of balance and coordination difficulties, slurring of speech, postural tremor, gait ataxia, and action myoclonus, among others. He was referred to physiotherapy by his physician.
This case study follows Mr. L through his rehabilitation journey, from initial assessment to current therapeutic interventions. These interventions include patient education, resistance training, range of motion exercises, balance and gait functional training, pelvic floor training, and dance therapy.
CLIENT CHARACTERISTICS[edit | edit source]
Mr. L is a 62-year-old retired NASA astronaut. He is currently living in California with his husband of 20 years, who is also retired. Mr. L first presented to his family physician three years ago with issues of erectile dysfunction, in which his doctor believed to be result of aging. Over the next year, Mr. L began developing other symptoms seemingly unrelated to his previous health history. He presented with noted difficulty balancing, asymmetric postural tremor (right side), bradykinesia, rigidity, urinary incontinence, and minor slurring of speech – warranting a probable diagnosis of Parkinson’s disease. Mr. L was prescribed oral Levodopa (250 milligrams, four times a day). This medication eased his symptoms for four months, but gradually, he began noticing the return of his symptoms – warranting a reassessment. Despite increasing his medication dosage, Mr. L’s chief complaints were perpetuated. Additionally, he began experiencing gait ataxia with cerebellar dysarthria, action myoclonus, and cold hands and feet. After conducting a thorough physical assessment, it was noted that Mr. L presents with orthostatic hypertension (dropping from 120/94 mmHg in a recumbent position, to 90/68 mmHg, after prolonged standing). Based on the presenting factors, a diagnosis of Multiple System Atrophy-Parkinsonism (MSA-P) was established. The physician referred Mr. L to physiotherapy for gait and mobility training, pelvic floor training, and education on symptom management.
EXAMINATION FINDINGS[edit | edit source]
Subjective[edit | edit source]
Patient Profile[edit | edit source]
- DOB: November 28, 1958 (62 y/o)
- Gender: Male
- Significant Presentation: Probable MSA progressing over 3 years
History of Present Illness[edit | edit source]
Diagnosis of probable MSA-P three weeks ago, right-sided postural tremor, difficulty balancing, bradykinesia, rigidity, urinary incontinence, slurred speech, cerebellar dysarthria, cold hands and feet, action myoclonus, and orthostatic hypotension.
Past Medical History[edit | edit source]
N/A
Previously healthy
Medications[edit | edit source]
- Levodopa (250 mg 4X/day, for 4 months)
- Levodopa (500 mg 4X/day, for 2 months)
- CBD for pain management (occasional)
Health Habits[edit | edit source]
Non-smoker, non-drinker, formerly very active (prior to symptom onset)
Family History[edit | edit source]
No family history of progressive neurological disorders
Psychosocial[edit | edit source]
Patient is experiencing marital issues due to the progressive nature of the disease. Patient also expresses concerns of loneliness, isolation, and depression due to fatality of the diagnosis. Mr. L also worries about burdening his partner and family as the disease progresses and he becomes less independent. Having been previously very active, Mr. L is having trouble coping with his new sedentary lifestyle. Previously, Mr. L volunteered weekly at his local YMCA, running a space exploration program for young children – bringing joy to his life. Due to cerebellar dysarthria, he is having trouble effectively communicating with others. Lastly, he used to really enjoy dancing with his husband but has not been able to do so recently because of his condition.
Living Environment[edit | edit source]
Two-story home with 14 stairs to the second floor. Bedroom located on second floor. Half bathroom on first floor, full bathroom on second floor. Second floor bathroom equipped with a spacious walk-in shower. Hardwood flooring throughout the home.
Functional History[edit | edit source]
Prior to probable MSA-P diagnosis: very active, running 15km a week and walking everywhere within the city. Drove when needed. Able to independently maintain his property and home chores. Able to complete all activities of daily living independently.
Current Functional Status[edit | edit source]
After probable MSA-P diagnosis: able to ambulate 200m independently, but very slowly and unsteadily. Beyond 200m, requires a rollator walker or assist X1. Requires assistance from his husband for ADLs (cooking, cleaning, bathing, shopping, etc.). Trouble controlling urination and bowel movements (requires protective underwear). Able to ascend and descend one flight of stairs with assist X1. Unable to drive. Fine motor activity is limited due to action myoclonus (unable to type). Trouble communicating due to dysarthria.
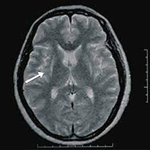
Imaging[edit | edit source]
MRI: T2 weighted MRI revealed a hyperintense putaminal slit sign bilaterally
Precautions/Contraindications[edit | edit source]
Depression, lack of social interaction (decreased involvement with community), and trouble communicating due to dysarthria (no difficulties with comprehension). Otherwise, no contraindications to a physiotherapy program.
Objective[edit | edit source]
General[edit | edit source]
Minor hypomimia, postural AP tremor, action tremor
Posture[edit | edit source]
| Standing | Rounded shoulders, right shoulder depression, forward head posture, forward lean, wide base stance |
| Seated | Rounded shoulders, right shoulder depression, posterior pelvic tilt |
Gait[edit | edit source]
Festination, shuffling (short stride) wide base gait, bradykinetic ambulation, reduced arm swing bilaterally, action myoclonus more prominent during ambulation
Tone[edit | edit source]
High tone on right side of body in comparison to the left
Active Range of Motion (AROM)[edit | edit source]
Upper Extremity
| Left | Right | |
| Shoulder flexion | 80° | 65° |
| Shoulder extension | 40° | 30° |
| Shoulder abduction | 150° | 110° |
| Shoulder adduction | 75° | 70° |
| Elbow flexion | 130° | 120° |
| Elbow extension | 0° | -5° |
| Wrist flexion | 90° | 90° |
| Wrist extension | -10° | -20° |
Lower Extremity
| Left | Right | |
| Hip flexion | 115° | 109° |
| Hip extension | -4° | -4° |
| Hip abduction | 40° | 38° |
| Hip adduction | 45° | 42° |
| Knee flexion | 120° | 115° |
| Knee extension | -5° | -10° |
| Ankle dorsiflexion | 50° | 50° |
| Ankle plantarflexion | 5° | 0° |
| Ankle inversion | 34° | 35° |
| Ankle eversion | 15° | 5° |
Trunk
| C-Spine | T-Spine | L-Spine | |
| Flexion | 50° | 30° | 50° |
| Extension | 10° | 10° | 15° |
| Side flexion L/R | 30/25° | 30/25° | 25/15° |
| Rotation L/R | 70/65° | 30/25° | 0/0° |
Passive Range of Motion (PROM)[edit | edit source]
PROM limited by muscle rigidity and contracture
Strength[edit | edit source]
| Respiratory | MIP: 39.08% of normal values
MEP: 49.59% of normal values |
| Musculoskeletal | Manual muscle testing revealed global muscle weakness (4/5) |
Neurological Testing[edit | edit source]
| Upper Motor Neuron Testing |
|
| Lower Motor Neuron Testing | Normal |
| Myotomes | Abnormal |
| Dermatomes | Sensation WNL |
Self Reported Outcome Measures[edit | edit source]
| Activities-Specific Balance Confidence Scale (ABC)[2] |
|
| Short Form – 36 (SF36)[3][4] |
|
Outcome Measures[edit | edit source]
| Unified Multiple System Atrophy Rating Scale (UMSARS)[5] |
|
| Timed Up and Go (TUG) Test[6] |
|
| Performance-Oriented Mobility Assessment (POMA)[7] |
|
| Function Reach Test[8] |
|
| Single Limb Stance (SLS)[9] |
|
DIAGNOSIS[edit | edit source]
Patient is a 62-year-old male presenting with initial symptoms of bradykinesia, urinary incontinence, difficulty balancing, and increasing issues with ambulation [UMSARS (60/104), TUG (19 seconds), POMA (22/28), SLS (inability), ABC (50%)]. Due to these outcome measure scores and initial presentation the patient is also at an increased risk of falls. The patient was diagnosed with Multiple Systems Atrophy - parkinsonism subtype (MSA-P) and referred to physiotherapy address these issues. The patient expressed concerns regarding their decreasing independence with ADL’s and decreased mental health quality of life due to previously active lifestyle. Although this diagnosis is progressive and will lead to fatality Physiotherapy will be helpful for the patient to improve confidence and functional independence through an exercise program with high focus on balance, mobility, and light resistance training. The patient will also benefit from education surrounding symptom and overall management.
PROBLEM LIST[edit | edit source]
- Decreased ambulatory agility and increased fall risk (TUG = 19 seconds)
- Moderate fall risk as per his 22/28 POMA score
- Decreased mental health and feeling of independence due to the progression of the disease
- Decreased Quality of life 12/36 on the SF-36 questionnaire
- Increased right-sided tone and rigidity during PROM
- Bradykinetic ambulation with festination’s during gait and ADLs
- Decreased right sided AROM compared to right (UE’s and LE’s)
- Decreased confidence during gait and ADL’s due to fear of falling (ABC 50%)
- Right UE and LE weakness during resisted movements (RIM = 4/5 globally)
- Orthostatic hypotension (130/82mmHg to 98/76mmHg)
- Moderate-severe impairment and functioning within various domains (motor, autonomic, and ADL’s) seen during UMSARS Assessment
- Urinary incontinence due to autonomic decline associated with MSA progression
- Lack of knowledge regarding support/progression of condition
PATIENT GOALS[edit | edit source]
Short-Term Goals[edit | edit source]
- Body Structure/Function
- Increase shoulder flexion on both left and right sides from 80 and 65 degrees, respectively, to 120 degrees within 3 weeks.
- Improve right shoulder abduction from 110 degrees to 150 degrees within 3 weeks.
- Activity
- Increase Activities-Specific Balance Confidence Scale from 50% to 65% (MDC = 13%) within 4 weeks
- To be able to stand on one limb within 5 weeks so he can pass the single-leg stance test
- Participation
- Gain strength and aerobic capacity through countertop exercises so he will be able to help his husband cook at home within 3 weeks
- Ensure that the patient has adequate supports and education for both himself and his family within one week of the initial visit to assist with future needs
Long-Term Goals[edit | edit source]
- Body Structure/Function
- Increase pelvic floor strength through exercise to minimize the risk of urinary incontinence within 8 weeks
- Improve both upper extremity and lower extremity strength through resisted exercise interventions within 10 weeks
- Activity
- Ambulate 500 meters with the use of a quad cane and no extra assistance before having to stop due to fatigue in 8 weeks
- Ascend one flight of stairs with no additional supports within 8 weeks
- Participation
- Encourage Mr. L to go on 3 short walks around the block per week with husband, using rollator to improve daily physical activity
- Improve his SF-36 score from 12/36 to 24/36 within 10 weeks which would demonstrate an improvement in overall quality of life
INTERVENTION[edit | edit source]
| Treatment Intervention | Frequency | Intensity | Time | Rationale |
|---|---|---|---|---|
Education:
|
During appointment 1-2 when deemed appropriate | N/A | Ongoing throughout intervention | Problem List (3, 8, 12)
If the patient understands the role of physiotherapy and other members of the interprofessional team there will be better adherence to interventions. Providing clear explanations and education about the importance of physical activity and functional independence can ensure the patient and the rest of the circle of care is on the same page for the treatment going forward. This will lead to improved mental health and quality of life for the patient. |
Resistance Program:
|
3x/week | All exercises can be done with gravity as the resistance but can progress to weights as tolerated. | 2 sets of 8 repetitions each | Problem List (1, 2, 5, 7, 9, 11)
Since the patient has relatively weaker muscles, which has been causing him many issues such as decreased ambulation and increased fall risks as well as limitations in his activities of daily life, it is important to work on strengthening exercises to try to gain muscle strength. Resistance training has been shown to greatly improve muscle strength, gait, and postures in patients with MSA-P according to Sandalis et al (2001). In terms of the specific exercises that were selected for this intervention, it was important to focus on functional movements that could assist the patient with his ADLs, as well as addressing the lack of range of motion in the shoulder and hip joints. Should this exercise program for the patient become too easy, it can always be progressed by adding more sets and/or repetitions or increasing the resistance. |
Range of Motion:
|
2x/week during appointments | Moving into end range/ slight discomfort |
|
Problem List (5, 7)
Although range of motion, of which is limited in the patient, can often be addressed through muscle strengthening and functional tasks such as walking, it is still important to address range of motion deficits directly (Mazzoni, Shabbot, & Cortes, 2012). With muscle rigidity and limited range of motion being predominant characteristics of this patient, similar to most patients with MSA-P, active-assisted range of motion as well as passive range of motion from a physiotherapist should be included in the intervention. Passive range of motion can be completed as needed to ensure that there are limited contractures and rigidity while active-assisted range of motion can be done at home to maintain the newly achieved range of motion. |
Balance/Gait Specific Exercises:
|
3x/week | Light intensity during gait exercises | Balance
|
Problem List (1, 2, 3, 4, 6, 8, 11)
Balance exercises (specifically those with a focus on vestibular and visual training) have been shown to increase balance in patients with Parkinson’s disease and therefore patients like Mr. L who have a large component of parkinsonism accompanying his recent diagnosis of MSA-P[10]. There is also evidence that balance exercises combined with resistance training in the lower extremities will increase this benefit further[10]. Gait and balance exercises can decrease the risks of falls by improving TUG, POMA, and SLS while also aid in increasing Mr. L’s confidence while ambulating in the community[11]. Gait training and aerobic exercise will encourage Mr. L to continue his previously active lifestyle. |
Pelvic Floor Physio:
|
5x/week | Moderate intensity | Hold for 3-5 seconds
2 sets of 10 reps |
Problem List (3, 4, 12)
Since the patient is experiencing urinary incontinence which ultimately decreases his quality of life, Kegel exercises (pelvic floor exercises) have been incorporated into his intervention and home exercise program. This will ensure that the patient has better self-control with his urinary retention (Cavkaytar, Kokanali, Topcu, Aksakal, & Doganay, 2015) and should lead to him being capable of resuming some of his activities, such as dancing. |
| Group Rehabilitation Dance Classes: | Once per week | Light-moderate intensity | 30 minutes to start (can progress) | Problem List (1, 4, 3, 8)
Group dance targeted for individuals with neuromuscular diseases can help improve quality of life and sense of community involvement. Classes have also been shown to increase balance, gait, and confidence with movement[12]. Mr. L will especially benefit from this program because he can take what he learns and continue to dance with his husband. |
References[edit | edit source]
- ↑ http://www.ant-tnsjournal.com/Mag_Files/17-1/dw2008530184030_17-1-P74.pdf
- ↑ Powell LE, Myers AM. The activities-specific balance confidence (ABC) scale. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 1995 Jan 1;50(1):M28-34.
- ↑ Ware Jr JE. SF-36 health survey.
- ↑ Lins L, Carvalho FM. SF-36 total score as a single measure of health-related quality of life: Scoping review. SAGE open medicine. 2016 Sep 30;4:2050312116671725.
- ↑ Wenning GK, Tison F, Seppi K, Sampaio C, Diem A, Yekhlef F, Ghorayeb I, Ory F, Galitzky M, Scaravilli T, Bozi M. Development and validation of the unified multiple system atrophy rating scale (UMSARS). Movement Disorders. 2004 Dec;19(12):1391-402.
- ↑ Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. Journal of the American geriatrics Society. 1991 Feb;39(2):142-8.
- ↑ Tinetti ME, Speechley M. Prevention of falls among the elderly. New England journal of medicine. 1989 Apr 20;320(16):1055-9.
- ↑ Duncan PW, Weiner DK, Chandler J, Studenski S. Functional reach: a new clinical measure of balance. Journal of gerontology. 1990 Nov 1;45(6):M192-7.
- ↑ Vellas BJ, Wayne SJ, Romero L, Baumgartner RN, Rubenstein LZ, Garry PJ. One‐leg balance is an important predictor of injurious falls in older persons. Journal of the American Geriatrics Society. 1997 Jun;45(6):735-8.
- ↑ 10.0 10.1 Keus SH, Bloem BR, Hendriks EJ, Bredero‐Cohen AB, Munneke M, Practice Recommendations Development Group. Evidence‐based analysis of physical therapy in Parkinson's disease with recommendations for practice and research. Movement disorders. 2007 Mar 15;22(4):451-60.
- ↑ Mak MK, Pang MY. Balance confidence and functional mobility are independently associated with falls in people with Parkinson’s disease. Journal of neurology. 2009 May;256(5):742-9.
- ↑ Ciantar SR, Bearss KA, Levkov G, Bar RJ, DeSouza JF. Investigating Affective and Motor Improvements with Dance in Parkinson’s Disease. bioRxiv. 2019 Jan 1:665711.