Multiple Sclerosis (MS) Case Study: Difference between revisions
(I updated the intro and client characteristics sections and fleshed out some of the citations there.) |
Adrian Smith (talk | contribs) No edit summary |
||
| Line 5: | Line 5: | ||
==Patient Profile== | ==Patient Profile== | ||
Age: 29 | |||
Gender: Female | Gender: Female | ||
Occupation: Graphic Designer | Occupation: Graphic Designer | ||
Subtype: MS (relapsing-remitting) Dx currently? | Subtype: MS (relapsing-remitting) Dx currently? | ||
| Line 109: | Line 113: | ||
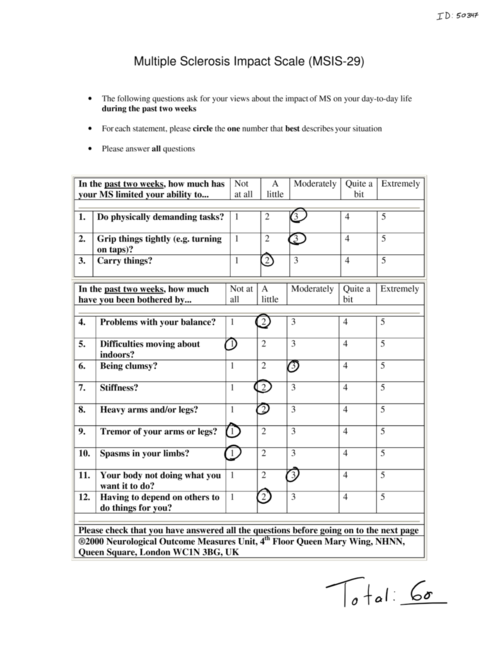
Multiple Sclerosis Impact Scale (MSIS-29) (<nowiki>https://academic.oup.com/brain/article/124/5/962/309935</nowiki>) was used to assess the impact of MS on the patient’s physical and psychological day-today wellbeing in the past 2 weeks. High levels of evidence and recommendation was given by the American Physical Therapy Association Neurology Section Task Force regarding the use of this outcome measure in outpatient MS. patients(<nowiki>https://academic.oup.com/ptj/article/94/5/593/2735536</nowiki>). The patient scored 23.75/100 in the physical impact scale and 30.56/100 in the psychological scale where higher scores indicate greater impact of MS on the patient’s daily wellbeing. The MCID for the physical impact scale has been estimated to be 8points and the psychological impact scale MCID has yet to be agreed upon in in current literature (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4416760/). | Multiple Sclerosis Impact Scale (MSIS-29) (<nowiki>https://academic.oup.com/brain/article/124/5/962/309935</nowiki>) was used to assess the impact of MS on the patient’s physical and psychological day-today wellbeing in the past 2 weeks. High levels of evidence and recommendation was given by the American Physical Therapy Association Neurology Section Task Force regarding the use of this outcome measure in outpatient MS. patients(<nowiki>https://academic.oup.com/ptj/article/94/5/593/2735536</nowiki>). The patient scored 23.75/100 in the physical impact scale and 30.56/100 in the psychological scale where higher scores indicate greater impact of MS on the patient’s daily wellbeing. The MCID for the physical impact scale has been estimated to be 8points and the psychological impact scale MCID has yet to be agreed upon in in current literature (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4416760/). | ||
[[File:MSIS-29 2.png|thumb|650x650px|Retrieved from <nowiki>https://www.mstrust.org.uk/sites/default/files/MSIS-29.pdf</nowiki>]] | [[File:MSIS-29 2.png|thumb|650x650px|Retrieved from <nowiki>https://www.mstrust.org.uk/sites/default/files/MSIS-29.pdf</nowiki>]] | ||
[[File:MSIS-29 1.png|left|thumb|648x648px|Retrieved from <nowiki>https://www.mstrust.org.uk/sites/default/files/MSIS-29.pdf</nowiki>]] | [[File:MSIS-29 1.png|left|thumb|648x648px|Retrieved from <nowiki>https://www.mstrust.org.uk/sites/default/files/MSIS-29.pdf</nowiki>]] | ||
| Line 329: | Line 334: | ||
(NICE: <nowiki>https://www.nice.org.uk/guidance/cg186/chapter/1-Recommendations</nowiki>) | (NICE: <nowiki>https://www.nice.org.uk/guidance/cg186/chapter/1-Recommendations</nowiki>) | ||
Outcome | === Outcome === | ||
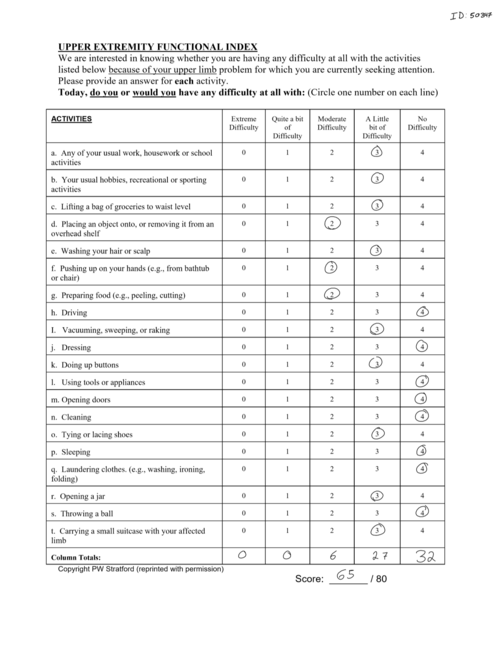
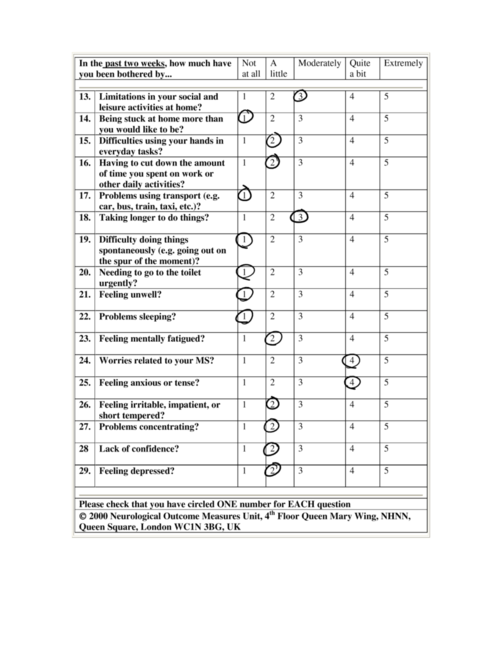
After 8 weeks of biweekly sessions, the patient has increased finger dexterity demonstrated by a decrease of 4.6 seconds on the right and 7.1 seconds on the left during the Nine-Hole peg Test. The patient was able to purchase a used e-bike which she describes as life changing. She is able to get on her bike and exercise without the fear of potentially getting stranded somewhere due to fatigue. The patient was able to receive funding through the Assistive Devices Program (ADP) allowing her to be fitted for an Ankle Foot Orthoses. As a result, decreased right foot drop and increased gait speed was observed. The results of the Six-Minute Walk Test also indicate a significant improvement of 79 meters from baseline (total 487 meters). Furthermore, the patient reports feeling more confident during ambulation. The patient demonstrated some other improvements according to the outcome measures re-administered during the last assessment. For the Upper Extremity Functional Scale (UEFS) she scored a 70/80 indicating improvement in upper extremity function. For the Fatigue Scale for Cognitive and Motor Function her total score of 36/100, (14/50 on cognitive fatigue and 22/50 on the motor fatigue) also indicates improvement. The MSIS-29 showed similar improvement, with a reduction of the physical impact score from 23.75 to 16.25, and the psychological impact score reduced to 25, from 30.56 prior. The patient has met all goals (i.e., increase balance, decrease fatigue, increase upper limb function and dexterity) and is ready to be discharged and seen on a “as needed” basis for exercise progression. The importance of continuing to be physically active and monitoring fatigue was emphasized to the patient during the last appointment. | |||
After 8 weeks of biweekly sessions, the patient has increased finger dexterity demonstrated by a decrease of 4.6 seconds on the right and 7.1 seconds on the left during the Nine-Hole peg Test. The patient was able to purchase a used e-bike which she describes as life changing. She is able to get on her bike and exercise without the fear of potentially getting stranded somewhere due to fatigue. The patient was able to receive funding through the Assistive Devices Program (ADP) allowing her to be fitted for an Ankle Foot Orthoses. As a result, decreased right foot drop and increased gait speed was observed. The results of the Six-Minute Walk Test also indicate a significant improvement of 79 meters from baseline (total 487 meters). Furthermore, the patient reports feeling more confident during ambulation. The patient demonstrated some other improvements according to the outcome measures re-administered during the last assessment. For the Upper Extremity Functional Scale (UEFS) she scored a 70/80 indicating improvement in upper extremity function. For the Fatigue Scale for Cognitive and Motor Function her total score of 36/100, (14/50 on cognitive fatigue and 22/50 on the motor fatigue) also indicates improvement. | |||
==Discussion== | ==Discussion== | ||
Revision as of 02:18, 20 May 2020
Case Study Assignment[edit | edit source]
* In progress, please do not edit prior to May 22, 2020*
The purpose of the present fictional case study is to demonstrate major multiple sclerosis (MS) clinical findings and propose appropriate, evidence-based management interventions that effectively address an active patient’s participation restriction.
Patient Profile[edit | edit source]
Age: 29
Gender: Female
Occupation: Graphic Designer
Subtype: MS (relapsing-remitting) Dx currently?
Referral: Recent Dx from family physician, referred to PT to aid in functional goals related to hiking/something else?
Problem List:
- Fatigue (mental & physical)
- Deteriorating dexterity (typing, things falling out of hand)
- Psychosocial aspects of life affected (inability to participate in bike rides with husband, fatigue affecting ability to work full days? And some job tasks affected)
Introduction[edit | edit source]
Multiple sclerosis (MS) is a neurological condition characterized by inflammatory demyelination over multiple episodes and locations in the central nervous system (Kalb, 2010). MS’ complex nature - its variance among patients, unpredictability, potential to create a heavy social and emotional burden on patients - can make appropriate, effective management challenging for community physiotherapists (Kalb, 2010). The debilitating symptoms (fatigue, arm movement and/or vision problems, ambulatory impairment, etc.; Kalb, 2010) can considerably impact patients’ ability to fulfill their occupational, familial, and community roles. The purpose of the present fictional case is to illustrate the clinical presentation of MS and propose appropriate, evidence-based management interventions that effectively address an active patient’s participation restriction.
Case:
29 year-old graphic designer Betty Jackson first noticed her symptoms in the summer of 2019 when she was biking along the lake with her husband and noticed she was experiencing difficulty reading signage and using her arms to keep her bike steady. As she finished her route she felt excessively fatigued. These symptoms persisted for a few days, eventually affecting her productivity at work, prompting a visit to her family physician. Upon assessment of MRI findings which showed demyelination plaques in the corpus callosum, the physician classified her event as a “clinically isolated syndrome” (Kalb, 2010) of MS. Approximately 10 months later, Betty’s symptoms resurfaced: she experienced the same fatigue, vision and arm issues as before. After seeing her physician again, a secondary MRI revealed more distal demyelination plaques. She was diagnosed with relapsing-remitting MS (RRMS; Kalb, 2010). The physician referred her to a private physiotherapy clinic in the community for motor control training and gait safety education. Betty is under considerable stress as a result of her recent diagnosis. She is fearful she will lose her job or will not be able to support her children considering potential future gait impairment and considerable fatigue.
Fatigue is of great importance to Betty’s participation as a worker and a parent. Regular exercise has been cited widely in the literature as beneficial for promoting restful sleep and reducing fatigue in individuals with MS (Snook et al., 2009; Motl & Gosney, 2008). Therefore education on, and implementation of regular safe exercise should play a central role in Betty’s treatment plan. As for addressing Betty’s concerns regarding gait, the National Multiple Sclerosis Society’s recommendations for managing gait impairment provide pertinent information to inform gait education and potential management of further impairment. They recommend addressing multiple aspects of gait including vision, fatigue, foot wear, and balance impairments (Kalb, 2010). Interestingly, in a case study conducted on a woman with similar concerns and clinical presentation, a 3 month locomotor training program involving a combination of virtual-reality based and overground balance interventions, and body-weight-supported/treadmill training twice a week, improvements were observed both at post-intervention and 2-month follow-up in gait speed, endurance and balance (Fulk, 2005).
A challenging aspect of this case is the significant occupational modification that will likely be necessary for the patient. Graphic design requires a high level of upper extremity motor function, and without considerable workplace modification, ergonomic intervention, or additional support from the employer, continuing to pursue this line of work may prove unrealistic. For this reason the involvement of an occupational therapist and/or social worker may be warranted.
Kalb, R. (2010). Multiple Sclerosis: A focus on rehabilitation. National Multiple Sclerosis Society, Professional Resource Center.
Snook, E. M., & Motl, R. W. (2009). Effect of exercise training on walking mobility in multiple sclerosis: a meta-analysis. Neurorehabilitation and neural repair, 23(2), 108-116.
Link: https://journals.sagepub.com/doi/pdf/10.1177/1545968308320641
Motl, R. W., & Gosney, J. L. (2008). Effect of exercise training on quality of life in multiple sclerosis: a meta-analysis. Multiple Sclerosis Journal, 14(1), 129-135.
Link: https://pdfs.semanticscholar.org/6708/a26bf557aa0651c4a3a919b557739c8169bb.pdf
Fulk GD. (2005). Locomotor training and virtual reality-based balance training for an individual with multiple sclerosis: a case report. Journal of Neurologic Physical Therapy, 29, 34-42. https://doi.org/10.1097/01.npt.0000282260.59078.e4
Client Characteristics[edit | edit source]
Betty Jackson is a 29 years old woman living with her spouse and two children in an apartment in Sudbury, Ontario. Her primary condition is RRMS. She was referred to the physiotherapy clinic by her general physician to address her motor control impairment. The physician also suggested education regarding gait and mobility aids to address Betty’s concerns about potential falls and disability. Additionally, Betty hopes to mitigate her fatigue so she can get more done at work.
Examination Findings[edit | edit source]
Date of Initial Assessment: May 12th 2020
Subjective Assessment:
Demographics
- Name: Betty Jackson
- Date of Birth: January 12, 1991
- Age: 29
- Sex: Female
History (Hx) of Present Illness
Medical diagnosis: Relapsing Remitting Multiple Sclerosis
- Diagnosed in April 2020 following MRI imaging ordered by her family physician
- 2 previous relapses (first relapse in June 2019, second relapse in March 2020) in the last year both of which presented with excessive fatigue, blurry vision, impaired upper extremity function
Rehabilitation History: Previously attended physiotherapy regarding rehabilitation of a sprained left ankle following a sports injury approximately 10yrs ago, but has not been to physiotherapy regarding current condition previously
Past Medical History:
- No current comorbidities or relevant past conditions
- No previous major surgeries
Current symptoms or status:
- Primary Complaints: Patient reports following her last relapse-remission episode, she has experienced uncoordinated, difficult arm and hand movements especially with her right arm which is her dominant side. In addition, the patient complains of occasional experiences of unsteadiness when taking a step, greater than normal fatigue following a work day and/or ADLs, and feeling “clumsier than usual”. Patient also reported occasional difficulty focusing on tasks at work.
- Aggravating Factors: warm weather, stressful work life
- Easing Factors: cooler weather, rest
Social History:
- Lives in an apartment with husband and two children (aged 4 and 5). Apartment building has 4 steps to the front entrance, and elevators to the patient's unit floor. Apartment unit has no stairs within. Husband works as an arborist (part-time to full-time depending on season). Patient also mentioned that her husband is a life-time indoors smoker and has no intention of quitting.
Hobbies: Enjoys biking with her husband, and playing with her kids
Occupation: Graphic designer, full-time
Functional status/Activity – current and previous
- Previously high activity level with complete independence
- No prior fall history but experiences occasional instability during longer periods of walking
- Currently reports difficulty with completing previously tolerable biking routes, and playing with her children for prolonged periods. Occasionally needs assistance from husband with work around the house and errands.
Other information:
Medications: Rebif (self-administered subcutaneously 3x per week) (reference this website and hyperlink “rebif”) https://mssociety.ca/managing-ms/treatments/medications/disease-modifying-therapies-dmts/rebif
Diagnostic Tests: MRI Imaging identifying both active and inactive demyelination plaques within the corpus callosum and in the periventricular white matter
Hand dominance: Right-handed
Health Habits: non-smoker, 1-2 wine glasses per week, no recreational drug use
Patient’s goals and concerns:
- Maintain and prevent as much upper extremity function and balance in walking as possible
- Manage fatigue symptoms as patient feels she no longer is able to participate in biking routes with her husband and friends
- Patient expressed serious concerns about future potential decreases in her own function and mobility and how it will affect her ability to work and take care of her children. This is especially a concern as her husband’s occupation is busiest during the summer when the temperature is higher, and the symptoms seem to be worse. Another area of concern for the patient is the recently noticed decline in her right arm and hand function which will greatly impact her occupation.
Self-reported Measures:
Upper Extremity Functional Scale (UEFS) (HYERLINK: https://www.physio-pedia.com/Upper_Extremity_Functional_Index) was administered to assess the patient’s ability to complete everyday activities using her upper extremities. Patient scored 65/80 upon initial assessment. A lower score on the UEFS indicates higher levels of disability.
Fatigue Scale for Cognitive and Motor Function was administered to assess the degree of the patient’s fatigue on cognitive and motor function. There is a high level of evidence and recommendation from the American Physical Therapy Association Neurology Section Task Force regarding the use of this outcome measure in outpatient MS patients (https://academic.oup.com/ptj/article/94/5/593/2735536). Patient scored 43/100 on the total score indicating mild fatigue, 17/50 on the cognitive fatigue sub-score which is below the cut-off for identifiable fatigue, and 26/50 on the motor fatigue sub-score indicating mild motor fatigue(https://journals-sagepub-com.proxy.queensu.ca/doi/pdf/10.1177/1352458509348519)
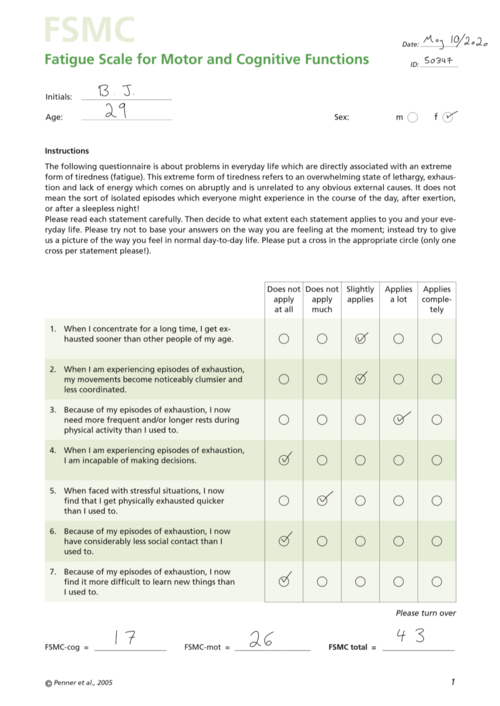
Multiple Sclerosis Impact Scale (MSIS-29) (https://academic.oup.com/brain/article/124/5/962/309935) was used to assess the impact of MS on the patient’s physical and psychological day-today wellbeing in the past 2 weeks. High levels of evidence and recommendation was given by the American Physical Therapy Association Neurology Section Task Force regarding the use of this outcome measure in outpatient MS. patients(https://academic.oup.com/ptj/article/94/5/593/2735536). The patient scored 23.75/100 in the physical impact scale and 30.56/100 in the psychological scale where higher scores indicate greater impact of MS on the patient’s daily wellbeing. The MCID for the physical impact scale has been estimated to be 8points and the psychological impact scale MCID has yet to be agreed upon in in current literature (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4416760/).
Objective Assessment:[edit | edit source]
Observation: Patient is visibly anxious, shifting weight in the seat often, and speaking quickly especially during conversation about her work, taking care of her children and how the future impairments of MS will affect this. Patient walked into the clinic independently with no gait aid.
Posture: Slight forward head posture but otherwise unremarkable.
Cognition: Patient is oriented to person, place, and time as well as alert.
Myotomes: WNL
Dermatomes: WNL
Sensation Testing: WNL
Active ROM:
- Csp: WNL
- Tsp: WNL
- Lsp: WNL
- L/E grossly: WNL
- U/E grossly: WNL
Manual muscle testing:
- Left: L/E grossly 4-. U/E grossly 3+
- Right: L/E grossly 4-. U/E grossly 3+
LMN reflexes: grossly grade 2+ (normal)
Clonus: Right side= Positive, Left Side=Negative
(https://bestpractice.bmj.com/topics/en-gb/140/history-exam)
Cranial Nerve Eye Movement Testing: Nystagmus noted in intermittently in right eye
(https://bestpractice.bmj.com/topics/en-gb/140/diagnosis-approach)
Heel-to-toe Test (10 repetitions each side):
- Left: WNL, Right: WNL
Finger-to-nose Test (10 repetitions each side):
- Patient was able to complete all repetitions bilaterally.
- Right: Patient’s movements become uncoordinated after 5th repetition and inaccurate upon target locating. Mild dysmetria noted as well.
- Left: Patient’s movements become uncoordinated after 8th repetition and inaccurate upon target locating. No dysmetria noted.
Finger-Opposition Test:
- Right: Slow, uncoordinated finger-to-pad movement noted.
- Left: slow movement noted during finger-to-pad noted. Coordination not affected.
Grip Strength-Dynamometer: RS: 20kgs, LS: 24kgs
- This is below average strength according to age based normative value (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3101655/).
6-minute walk test (hyperlink: https://www.physio-pedia.com/Six_Minute_Walk_Test_/_6_Minute_Walk_Test) High evidence in outpatient MS patients (https://academic.oup.com/ptj/article/94/5/593/2735536): 408m, slightly above mean for patients with MS with mild disability on EDSS. (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3076913/)
- The 6-minute walk test has high evidence and is recommended by the by the American Physical Therapy Association Neurology Section Task Force as an effective outcome measure to perform for patients with MS in outpatient clinical settings (https://academic.oup.com/ptj/article/94/5/593/2735536).
Gait: step length and step cadence slowed as patient approached end of 6minute walk test. Right foot noted at initial contact. Poor right sided foot clearance due to foot drop during mid-swing as patient approached end of 6-minute walk test (https://bestpractice.bmj.com/topics/en-gb/140/history-exam).
Spasticity: Modified Ashworth Scale (Kalb et al.)
- Lower extremity:
| Gross Body Movement | Modified Ashworth Grade - Left | Modified Ashworth Grade – Right |
| Hip Flexors | 0 | 0 |
| Hip Extensors | 0 | 0 |
| Hip Abductors | 0 | 0 |
| Hip Adductors | 0 | 0 |
| Knee Flexors | 0 | 0 |
| Knee Extensors | 0 | 1 |
| Ankle Dorsiflexors | 0 | 0 |
| Ankle Plantar Flexors | 0 | 1+ |
- Upper Extremity:
| Gross Body Movement | Modified Ashworth Grade - Left | Modified Ashworth Grade – Right |
| Shoulder Flexors | 0 | 1 |
| Shoulder Extensors | 0 | 0 |
| Shoulder Abductors | 0 | 1 |
| Elbow Flexors | 1 | 1 |
| Elbow Extensors | 0 | 0 |
| Wrist Flexors | 1 | 1+ |
| Wrist Extensors | 0 | 1 |
| Finger Flexors | 1 | 1+ |
| Finger Extensors | 1 | 1 |
(1): Slight increase in muscle tone, manifested by a catch and release or by minimal resistance at the end of the range of motion (ROM) when the affected part is moved in flexion or extension
(1+): Slight increase in muscle tone, manifested by a catch, followed by minimal resistance throughout the remainder (less than half) of the ROM. (https://www.strokengine.ca/en/indepth/mashs_indepth/)
Nine-Hole Peg Test (hyperlink: https://www.physio-pedia.com/Nine-Hole_Peg_Test):
- Left: 16 seconds
- Right: 19 seconds
- This is indicative of abnormal hand function in patients with MS who are at risk of limitations in activity and participation restrictions
- The American Physical Therapy Association Neurology Section Task Force has rated this outcome measure with a high level of evidence for patients with MS in an outpatient setting (https://academic.oup.com/ptj/article/94/5/593/2735536)
BERG balance scale (hyperlink: https://www.physio-pedia.com/Berg_Balance_Scale) : 50/56
- This score is above the cut-off score of 45/56, therefore indicating there is currently no increased risk of falls for the patient (https://academic.oup.com/ptj/article/76/6/576/2633009).
The BERG balance scale is recommended and has a high quality of evidence for outpatient patients with MS as determined in a consensus report by the American Physical Therapy Association Neurology Section Task Force (https://academic.oup.com/ptj/article/94/5/593/2735536).
Clinical Impression:[edit | edit source]
Physiotherapy Diagnosis:
29yr old female diagnosed with remitting-relapsing multiple sclerosis presenting with decreased motor coordination in bilateral upper extremity especially on the right dominant side, weakness in bilateral upper extremity, fatigue, and altered gait mechanics. The symptoms and deficits experienced by the patient have caused decreased ability to independently participate in instrumental activities of daily living, decreased productivity at work, decreased balance, decreased conditioning due to fatigue, and overall anxious outlook regarding her future function and independence. Prognosis is positively affected by the patient’s high motivation to maintain, supportive spouse, and previously high level of activity. Prognosis is negatively affected by anxious and stressful thoughts regarding future functions, and passive smoking at home. The patient will benefit from physiotherapy services to increase function of upper extremity, increased balance, manage fatigue, optimize gait pattern, and improve patient’s attitude towards the future.
Problem List:
- Bilateral upper extremity weakness
- Decreased upper extremity motor coordination affecting occupation and activities of daily living
- Increased right dominant hand dexterity affecting occupation
- Decreased tolerance to activity due to fatigue
- Decreased balance
- Altered gait pattern
- Decreased participation in hobbies
- Decreased productivity at work
Intervention[edit | edit source]
Gait Aid
The use of gait aids such as canes have been indicated as a fall risk factor in individuals with MS of varying ages (Cattaneo 2002, Nilsagard 2009, Coote 2013). Considering the patient's right-sided deficits during gait (i.e., step length/cadence, foot drop, poor foot clearance) particularly after several minutes of testing, an ankle-foot orthosis (AFO) or functional electrical stimulation (FES) can be worn to mitigate the drop foot.
Several studies have demonstrated that FES and AFO use can improve mobility, improve walking speed, reduce walking effort, and reduce incidence of falls, leading to improved quality of life in people with MS (Taylor 2016, Dapul 2015, Bulley 2014, van der Linden 2014, Esnouf 2010). Bulley et al, 2014 concluded that individuals using either device (i.e., AFO or FES) reported assistance on hills/stairs, increased participation in life, greater confidence, less stress, and less mental effort when walking.
Home Based Intervention
I). Aerobic Training: Taking into consideration the patient's hobbies, she can potentially seek out a bicycle with pedal assist (i.e., e-bike). An e-bike would allow her to pedal normally and if needed she can use the pedal assist (e.g., uphill or once fatigue begins to set in). Other methods of optimizing performance would be to have her bike at dusk or dawn to avoid the peak temperatures during the day and avoid overheating.
- Frequency: 2x/week
- Intensity: Moderate intensity (5/10 RPE)
- Type: Aerobic
- Time: 30min
(https://www.csep.ca/en/guidelines/physical-activity-guidelines-for-special-populations)
II). Dexterity and Upper Limb Training: The patient's occupation requires a certain degree of dexterity to manipulate different graphic design tools. The use of manipulable objects (e.g., clay, nuts/bolts, marbles) in patients with MS presenting with upper limb dexterity complications has been shown to significantly improve motor functioning, manual dexterity and hand grip strength (Ortiz-Rubio 2016, Lammers 2016, Kamm 2015).
II.a) Modeling Clay kneading: Patient kneads modelling clay with the hand forming a ball, flattening, and rolling and squeezing (5 sec) the clay (left and right hands).
- Frequency: 2x/week
- Intensity: N/A
- Type: Dexterity
- Time: 15min
II.b) Assembly: Patient assembles bolts and nuts of varying sizes using both hands.
- Frequency: 2x/week
- Intensity: N/A
- Type: Dexterity
- Time: 15min
II.c) Upper Limb Strengthening: Banded resistance training for shoulders and upper arms (Shoulder Flexion,
Horizontal Abduction, Elbow Extension, Elbow Flexion).
- Frequency: 2x/week
- Intensity: 50% 1RM (light resistance band)
- Type: Endurance
- Time: 1 set 10-15 reps with 1-2 minutes rest between exercises
(https://www.csep.ca/en/guidelines/physical-activity-guidelines-for-special-populations)
Therapist-Guided Interventions[edit | edit source]
I) Vestibular and Coordination Training (PT supervised): The patient expresses a fear of falling/tripping due to continued balance issues. Specific balance and vestibular intervention have been shown to decrease risk of falls, decrease fatigue, and increase upright postural control (Coote 2013, Hebert 2011).
Upright Postural Control: Standing with eyes open. Progress to foam surface and try with eyes closed when appropriate.
- BOS: firm surface—shoulder width apart
- BOS: firm surface—heels and toes together
- BOS: firm surface—tandem
Perform 1–3 with:
- Ball catch/toss (from and to PT)
- Head movement: head up (neck extension) and down (neck flexion)
- Frequency: 2x/week
- Intensity: N/A
- Type: Vestibular/Coordination
- Time: 30min
II.) MS Education: There is strong evidence for incorporating education about fatigue management and energy conservation especially in conjunction to exercise programs (Khan 2017, Asano 2014, Finlayson 2011, Hebert 2011). Education can include topic such as;
- Work simplification (finding ergonomic tools for her workplace)
- Impact of heat and time of day on fatigue level
- Mindfulness-based training
- The importance of continuing exercise after the treatment program for long-term benefits
(NICE: https://www.nice.org.uk/guidance/cg186/chapter/1-Recommendations)
Outcome[edit | edit source]
After 8 weeks of biweekly sessions, the patient has increased finger dexterity demonstrated by a decrease of 4.6 seconds on the right and 7.1 seconds on the left during the Nine-Hole peg Test. The patient was able to purchase a used e-bike which she describes as life changing. She is able to get on her bike and exercise without the fear of potentially getting stranded somewhere due to fatigue. The patient was able to receive funding through the Assistive Devices Program (ADP) allowing her to be fitted for an Ankle Foot Orthoses. As a result, decreased right foot drop and increased gait speed was observed. The results of the Six-Minute Walk Test also indicate a significant improvement of 79 meters from baseline (total 487 meters). Furthermore, the patient reports feeling more confident during ambulation. The patient demonstrated some other improvements according to the outcome measures re-administered during the last assessment. For the Upper Extremity Functional Scale (UEFS) she scored a 70/80 indicating improvement in upper extremity function. For the Fatigue Scale for Cognitive and Motor Function her total score of 36/100, (14/50 on cognitive fatigue and 22/50 on the motor fatigue) also indicates improvement. The MSIS-29 showed similar improvement, with a reduction of the physical impact score from 23.75 to 16.25, and the psychological impact score reduced to 25, from 30.56 prior. The patient has met all goals (i.e., increase balance, decrease fatigue, increase upper limb function and dexterity) and is ready to be discharged and seen on a “as needed” basis for exercise progression. The importance of continuing to be physically active and monitoring fatigue was emphasized to the patient during the last appointment.
Discussion[edit | edit source]
Self study questions[edit | edit source]
References [1]
Any and all images follow copyright regulations outlined by Physiopedia [2]