Multiple Sclerosis: A Case Study
Introduction:[edit | edit source]
Multiple Sclerosis (MS) is an autoimmune disorder characterized by demyelination and subsequent axonal injury and loss in the central nervous system (Kamm, Uitdehaag, & Polman, 2014). This injury to the central nervous system causes white matter lesions, also known as plaques, which are responsible for the patients’ symptoms. There are a few different classifications of MS based on occurrence of relapses or progression. The most common form is Relapsing Remitting MS (RRMS) whereby the patient will have new symptoms emerge or a worsening of past symptoms, followed by full, or near full recovery (Kamm, Uitdehaag, & Polman, 2014). The majority of RRMS cases eventually transition to a progressive form called Secondary Progressive Multiple Sclerosis (SPMS) (Kamm, Uitdehaag, & Polman, 2014). About 15% of MS cases are Primary Progressive (PPMS) where function continues to decline from onset (Kamm, Uitdehaag, & Polman, 2014). This case study follows a young female patient with Relapsing Remitting MS.
This case study discusses a 27 year old female diagnosed with Relapsing Remitting Multiple Sclerosis two years ago.
Patient first noticed symptoms that persisted for 24 hours including vision loss in one eye accompanied by facial weakness, numbness and difficulty with speech (dysarthria) in April of 2017. After the symptoms did not subside, patient reached out to her family doctor who then suggested further testing. Patient underwent magnetic resonance imaging (MRI) and a lesion was revealed on the brainstem. These results lead to Jane being classified as having Clinically Isolated Syndrome (Lublin et al. 2014). Patients such as this one are classified as having Clinically Isolated Syndrome when an initial event leads to a clinical presentation of symptoms and the MRI reveals lesions (Lublin et al. 2014). It wasn’t until three months after her initial MRI that the patient started experiencing extreme fatigue and balance problems possibly due to lower extremity weakness. She underwent a second MRI which revealed another lesion in her right cerebral hemisphere. Due to a relapse in her symptoms, she was formally diagnosed with Relapsing Remitting Multiple Sclerosis (RRMS) (Lublin & Reingold, 1996). It has been two years since the patients diagnosis and she has opted to come to physiotherapy to help control her fatigue, lower limb weakness, coordination and maintain general fitness.
The purpose of this case study is to present the patients symptoms of MS (fatigue, balance and lower limb weakness) and their response to physical therapy treatment. Similar cases of moderate to severe Multiple Sclerosis presenting with fatigue and weakness have shown significant improvements through physical therapy treatment (Khan & Amataya, 2017). In general, both strength training and endurance training result in fatigue reduction, however evidence is insufficient to specify which training modality has the strongest effect (Khan & Amataya, 2017). Paltamaa (2012) concluded that although there is a need for specificity of balance exercises in people with MS there is evidence that suggests progressive aerobic and resistance exercises have positive effects on balance in people with MS who present with mild or moderate symptoms (people who are still able to perform such exercises).
Client Characteristics:[edit | edit source]
Patient is a 27 year-old caucasian female diagnosed with Relapsing Remitting Multiple Sclerosis that began two years ago. The patient is a current smoker and has a history of depression. The patient self referred herself to physiotherapy to help manage her weakness, coordination and fatigue. Additionally, the patient is looking to learn how to self manage her symptoms.
Examination Findings:[edit | edit source]
Subjective Assessments
History of Present Illness:
- Medical diagnosis (Dx): Relapsing Remitting Multiple Sclerosis
- Rehabilitation Hx: no previous physiotherapy intervention used for current symptoms
- Current symptoms: fatigue, weakness (mainly in lower extremities), difficulty with gait, impaired balance and coordination
Medical History:
- Past medical Hx: diagnosed with Mononucleosis at age 17
- Co-morbid condition: diagnosed with depression at age 15 and currently smokes an average of 1 pack of cigarettes every 2 days
Social History:
- Lives with partner in a bungalow that has 6 steps to reach the entrance of the home, parents live 15 minutes away, works as a 4th grade teacher
- Hobbies include skiing and hiking
Functional Status:
- Reports difficulty finding motivation to leave the house or do simple housework due to fatigue
- Feels like her legs are too weak to participate in her hobbies, and hasn’t attempted to ski since diagnosis. She occasionally will go on short, easy hikes if she's having a good day.
Medication:
Alysse (birth control)
Ocrelizumab/Ocrevus (infusion treatment for multiple sclerosis)
Self report tests:
- Lower Extremity Function Questionnaire (LEFS) was used to assess the patient's ability to perform everyday tasks. The lower the score, the greater the disability (Lower Extremity Function Questionnaire, n.d.)
- Patient Health Questionnaire (PHQ-9) was used to assess the patient's depression severity. A score of 10 suggests moderate depression severity and that judgements on treatment should be based on the patient's functional impairments and duration of symptoms (Patient Health Questionnaire, n.d.).
- Fatigue Severity Scale (FSS): Mean score of 5.3 (>/=4 classified as substantial fatigue)
- Rosti‐Otajärvi et al. (2017) states adequate validity and reliability of FSS
Diagnostic Tests:
- Magnetic Resonance Imaging (MRI)
- Lumbar puncture (spinal tap)
Objective Assessment
Timed Up and Go (TUG): 10.5 seconds = just above the norm of < or equal to 10 seconds
Berg: 46/56 = 42-56% at an increase risk of falling
Cranial nerve function tests: WNL except CNXII had decrease sensation and motor control over V1
Babinski: positive
Clonus: positive
LMN reflexes UE/LE: WNL
Dermatomes: WNL
Myotomes: UE: not tested; LE: WNL
Resisted LE testing: hip flexors, knee extensor, knee flexors 4-/5, DF and PF 4/5
Heel knee shin test: 3 bilaterally showing minimal impairment; patient is able to accomplish activity with slightly less than normal control, speed and steadiness
Finger to nose test: WNL (4) on right; 3 on left showing minimal impairment; patient is able to accomplish activity with slightly less than normal control, speed, steadiness
Sensation testing: superficial and deep: WNL
Clinical Impression:[edit | edit source]
Patient was a previously active 27 year old woman diagnosed with Relapsing Remitting Multiple Sclerosis two years ago when she first started showing signs of the disease. Three months within the year, the patient experienced her her first relapse of the disease which ultimately lead to
Problem List:
- Fatigue impacting overall quality of life
- Lower limb weakness impairing functional mobility
- Impaired coordination affecting activities of daily living
- Current smoke (1 pack every 2 days)
Intervention:[edit | edit source]
Patient Centred Goals:
Short Term Goals:
- Improve lower extremity strength, by successfully completing 10 consecutive moderate depth unsupported squats by 2 months.
- Successfully coordinate 3 consecutive jumping jacks by 2 months.
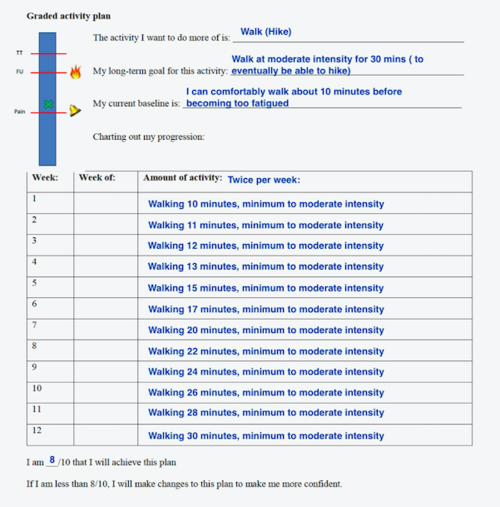
- Improve walking endurance to 30 minutes of moderate intensity using a graded exercise walking program by two months.
- Reduce smoking to 1/2 pack per week by 2 months.
Long Term Goals:
- Reduce score on the FSS to average of 4 or below within 6 months.
- Hike a moderate difficulty trail for a duration of 1 hour within 6 months.
- Ski 2 green runs in a day within 2 years.
- Cessation of smoking by 6 months.
Approaches/Techniques:
Adults with MS should engage in at least 30 minutes of moderate intensity aerobic activity 2 times per week and strength training of major muscle groups 2 times per week to achieve important fitness benefits (Latimer-Cheung, 2013).
Resistance Training:
The patient will start with 10-15 reps for one set and will work up to doing 2 sets for strength exercises such as squats, leg press, hamstring curls, abductor/adductor machine and calf raises.
Aerobic Training:
The patient will participate in a graded walking activity plan until she can sustain a moderate intensity walk for a 30 minute duration as seen in the figure below:
Tai Chi will be recommended to the patient to help improve overall balance and coordination. Tai Chi has been proven to have consistent and significant improvements in patients with MS’ balance and coordination. In addition, the physical exercise and mindfulness training incorporated in Tai Chi has shown improvements in patients mental health, specifically depression. The patient will begin incorporating Tai Chi into her schedule by participating in 30 minutes per week and eventually progressing to the recommended 45 minutes per week (Burschka, Keune, Oy, Oschmann, & Kuhn, 2014).
Self Management:
1) Keep an activity and symptom diary to track symptoms and discover patterns
2) Education on energy conservation strategies
- forming a mental map of resting spots/benches for outings
- Have a set plan for the day to avoid fatigue (ex. doing more fatiguing exercises at the end of the day)
3) Education on importance of keeping core temperature low to avoid disease worsening symptoms (Allen et al., 2018) and how to accomplish this
- Taking breaks
- Seated exercises
- Working out in a cool environment
4) Incorporating social cognitive therapy (SCT) into the exercise program. SCT includes educating patient on goal setting, outcome expectations and self efficacy (Coote et al., 2017).