Multifocal Motor Neuropathy: Difference between revisions
No edit summary |
No edit summary |
||
| Line 130: | Line 130: | ||
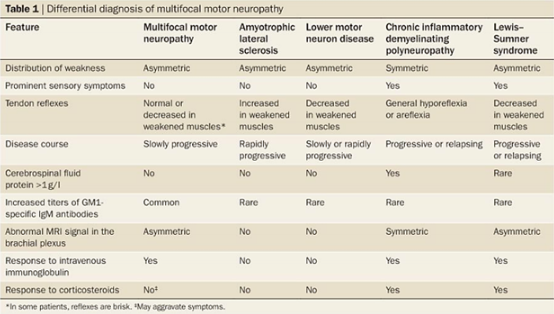
Figure 4: Methods of differentiating between MMN and other possible diagnoses (source)<br> | Figure 4: Methods of differentiating between MMN and other possible diagnoses (source)<br> | ||
== Videos == | == Videos == | ||
add text here relating to key evidence with regards to any of the above headings<br> | |||
== Resources <br> == | == Resources <br> == | ||
Revision as of 02:36, 9 May 2018
Be the first to edit this page and have your name permanently included as the original editor, see the editing pages tutorial for help.
Clinically Relevant Anatomy
[edit | edit source]
Multifocal motor neuropathy (MMN) is a rare disorder predominantly causing weakness in the distal limbs (1). The disorder is purely a motor neuropathy that presents asymmetrically and progresses slowly(1). To distinguish MMN from a motor neuron disease, a conduction block was found as the electrophysiological characteristic (2-4). Axon death occurs due to the lack of conduction which can lead to an entire nerve being affected. The nerves that are typically affected are peripheral nerves and more commonly the radial, ulnar, median and tibial nerves, however; it can affect other nerves as well (1,13). Since its symptoms are similar to that of chronic inflammatory demyelinating polyradiculoneuropathy (CIDP) in that they both occur due to a conduction block, it has been said that MMN is likely an immune-mediated neuropathy (source on doc).
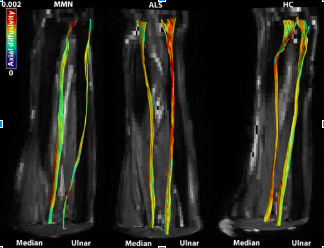
Figure 1: Comparison of the fibre tractography of the ulnar and median nerves in individuals with MMN (left), ALS (middle) and healthy controls (right). The colours indicated correspond to the axial diffusivity (mm2/s) which is correlated with axonal degeneration (source in doc).
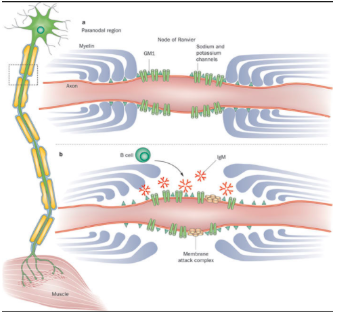
Figure 2: Demonstration of the conduction of electrical signal being blocked on the axon of individuals with MMN (source).
Epidemiology/Prognosis
[edit | edit source]
MMN more commonly affects males in comparison to females with a ratio of 2.7:1(1). Symptoms do not typically appear before the age of 50 years old(1). Men typically experience an earlier onset of MMN symptoms compared to females (1). MMN is not typically found in individuals over 70 years old (1).
The disorder is very similar to amyotrophic lateral sclerosis, however; MMN is seen as a treatable disorder with a good prognosis (10). MMN does not often negatively affect an individual’s lifespan, however; quality of life is often compromised due to symptoms like poor dexterity in manual tasks that are needed for activities of daily living. (Guimarães-Costa R, Bombelli F, Léger J. Multifocal motor neuropathy. Current opinion in neurology. 2013;26:503.) When compared to other diseases such as lower-motor-neuron disease, patients with MMN have a better overall prognosis (source on doc)
Mechanism of Injury / Pathological Process[edit | edit source]
MMN is a disease that progresses steadily (1). Despite the progression of the disease, those affected tend to have a normal life expectancy (1). The underlying pathological process of MMN still remains unclear, however it appears to be immune-mediated, with GM1-specific IgM antibodies playing an important role (review article). A common characteristic of MMN is a motor conduction block, which is evident in electrophysiological studies (82-85). These studies show whether motor axons have an inability to propagate action potentials(82-85). The decreased ability to propagate action potentials, coupled with axonal death lead to motor deficits which create many of the problems related to MMN (10). The pathological process responsible for this may be related to dysfunction of the nodes of Ranvier, which can lead to action potential conduction failure (86, 88). It has also been suggested that demyelination may also occur, however limited evidence and research related to this exists (86, 88). Given this information, nerve dysfunction related to MMN appears to be more generalized rather than specifically related to nerve conduction blocks and local dysfunction of the axonal membrane (82). Further research is still required in order to understand the pathological process of MMN in further detail.
Clinical Presentation[edit | edit source]
Symptoms:
- Asymmetrical distal limb weakness, which follows a nerve path, but does not include sensory loss (typically tibial, radial, ulnar and median nerves) (1,13).
- Wrist drop is usually the first symptom seen along with foot drop and a reduction in grip strength (1,13).
- Symptoms typically start in the leg and typically move to the arm. Later on symptoms may move to the upper arm but rarely move to the upper leg (1).
- Weakness tends to increase when exposed to cold environments (14).
- Patients who have the disease for a long time will typically experience muscle atrophy (12,13).
- Cramps and fasciculations appear in over 50% of patients (12).
- Decrease in tendon reflexes in the affected muscles are common (12).
- In rare cases, respiratory issues may occur because of the involvement of the phrenic nerve (16-19).
- Over 50% of patients experience significant fatigue that affects their daily living and careers (1).
Diagnostic Procedures[edit | edit source]
Diagnosis of MMN is found using clinical and electrophysiological characteristics (5). The results can be supported using ancillary investigations which may present as normal or slightly elevated CSF protein, abnormal signals in the brachial plexus as seen in an MRI, and blood work to assess GM1-specific IgM antibodies (15, 20, 22-24). Ultrasonography has also shown enlargements along the brachial plexus in about 90% of patients (12).
Figure 3: Flowchart of method of diagnosing MMN (55)
Diagnostic Criteria[edit | edit source]
Clinical criteria (source***)
1. Slow or stepwise progressive limb weakness
2. Asymmetric limb weakness
3. Fewer than seven affected limb regions
4. Decreased or absent tendon reflexes in affected limbs
5. Signs and symptoms more pronounced in arms than in legs
6. Age 20-65 years at disease onset
7. No objective sensory abnormalities except for vibration sense
8. No bulbar signs or symptoms
9. No upper motor neuron features
10. No other neuropathies
11. No myopathy
Laboratory criteria
1. Cerebrospinal fluid protein <1g/l
2. High GM1-specific IgM antibody titer
3. High signal intensity on T2-weighted MRI of the brachial plexus
Electrodiagnostic criteria
1. Definite motor conduction block
2. Probable motor conduction block
3. Slowing of conduction compatible with demyelination
4. Normal sensory nerve conduction in arm segments with motor conduction block; normal sensory neuron action potential amplitudes on distal stimulation
Definite MMN
1-11 on clinical criteria, 1 on laboratory criteria, and 1 and 4 on electrodiagnostic criteria
Probable MMN
1-3 and 6-11 on clinical criteria, 1 on laboratory criteria, and 2 and 4 on electrodiagnostic criteria
Possible MMN
1 and 7-11 on clinical criteria, 2 or 3 on laboratory criteria, and 3 and 4 on electrodiagnostic criteria
Outcome Measures[edit | edit source]
- Grip Strength
- INCAT Disability Scale
add links to outcome measures here (see Outcome Measures Database)
Medical Management / Interventions[edit | edit source]
Treatment and management options for MMN are limited. Early recognition of the disease is essential in order to prevent and delay axonal loss (10). Currently, high-dose intravenous immunoglobulin (IVIg) is the standard treatment for patients suffering from MMN and if used early on, it may prevent axonal damage (6-10). The use of IVIg has been shown to have improvements related to muscle strength and reduced disability. However, the decreases in disability tend to primarily be attributed to improvements in muscle strength. After many years of prolonged IVIg use, neurological deficits may progress despite a continual increase in dose of IVIg (10, 11). This is most likely due to continuing axonal degeneration which results in reduced muscular strength . Side effects of IVIg include rashes, chills, fever, mild hypotension or hypertension, nausea, malaise, headache and mild arthralgia (116). In order to determine the optimal dosage of IVIg, both muscle strength and muscle function should be monitored to optimize function (119). Other immunomodulatory therapies have been suggested, however mixed results have been found. Prednisolone and plasmapheresis appear to be ineffective in treating patients with MMN and may even have negative effects. (20,127,129) Cyclophosphamide, which was the first drug used to treat patients suffering from MMN, has been shown to be effective in some patients, however its adverse effects prevent its long-term use. (60)
Differential Diagnosis[edit | edit source]
Differential diagnoses for MMN include amyotrophic lateral sclerosis, lower motor neuron disease, chronic inflammatory demyelinating polyneuropathy and Lewis-Summer syndrome (5)
Figure 4: Methods of differentiating between MMN and other possible diagnoses (source)
Videos[edit | edit source]
add text here relating to key evidence with regards to any of the above headings
Resources
[edit | edit source]
add appropriate resources here
Case Studies[edit | edit source]
add links to case studies here (case studies should be added on new pages using the case study template)
References[edit | edit source]
References will automatically be added here, see adding references tutorial.