Morel-Lavallée lesion: Difference between revisions
No edit summary |
(Defintion, epidemiology/aetiology, pathophysiology added) |
||
| Line 3: | Line 3: | ||
== Definition == | == Definition == | ||
A Morel-Lavallée lesion (MLL) was first described in 1853 (1, | A Morel-Lavallée lesion (MLL) was first described in 1853<ref name=":0">Diviti S, Gupta N, Hooda K, Sharma K, Lo L. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5449878/pdf/jcdr-11-TE01.pdf Morel-Lavallee lesions-review of pathophysiology, clinical findings, imaging findings and management]. Journal of clinical and diagnostic research: JCDR. 2017 Apr;11(4):TE01.</ref> <ref name=":1">Singh R, Rymer B, Youssef B, Lim J. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6126206/pdf/main.pdf The Morel-Lavallée lesion and its management: a review of the literature]. Journal of orthopaedics. 2018 Dec 1;15(4):917-21.</ref>. It is a closed soft-tissue degloving injury<ref name=":0" /><ref name=":2">Zairi F, Wang Z, Shedid D, Boubez G, Sunna T. [https://reader.elsevier.com/reader/sd/pii/S1877056816000335?token=193AFCCCD9D35EF9227D6E4A8B2D40CD82BE93612C9E4AE3D66FCFDFAE18AF664140FDCB451AEEEC9F156AAC2CD3531C&originRegion=eu-west-1&originCreation=20221125075833 Lumbar Morel-Lavallée lesion: case report and review of the literature]. Orthopaedics & Traumatology: Surgery & Research. 2016 Jun 1;102(4):525-7.</ref><ref name=":3">LaTulip S, Rao RR, Sielaff A, Theyyunni N, Burkhardt J. [https://downloads.hindawi.com/journals/criem/2017/3967587.pdf Ultrasound utility in the diagnosis of a Morel-Lavallée lesion]. Case Reports in Emergency Medicine. 2017 Feb 1;2017.</ref><ref name=":4">Depaoli R, Canepari E, Bortolotto C, Ferrozzi G. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4353822/pdf/40477_2015_Article_157.pdf Morel-Lavallée lesion of the knee in a soccer player]. Journal of ultrasound. 2015 Mar;18(1):87-9.</ref><ref name=":5">Mettu R, Surath HV, Chayam HR, Surath A. [https://www.researchgate.net/publication/320866983_Chronic_Morel-Lavallee_Lesion_A_Novel_Minimally_Invasive_Method_of_Treatment Chronic Morel-Lavallée lesion: a novel minimally invasive method of treatment]. Wounds. 2016 Nov 1;28(11):404-7.</ref> that usually occurs after blunt trauma<ref name=":0" /><ref name=":1" /><ref name=":2" /><ref name=":4" />. In recent literature, it can also be referred to as Morel-Lavallée seroma or effusion, post-traumatic soft tissue cysts or post-traumatic extravasations<ref name=":1" />. | ||
== Epidemiology and aetiology == | |||
These injuries are uncommon<ref name=":1" /> and there is no consensus on the ratio of men to women. One source reported a 2:1 ratio<ref name=":1" /> while another reported a 1:1 ratio<ref>Christian D, Leland HA, Osias W, Eberlin S, Howell L. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5065277/pdf/jrcr-10-7-30.pdf Delayed presentation of a chronic Morel-Lavallee lesion]. Journal of Radiology Case Reports. 2016 Jul;10(7):30.</ref>. | |||
These injuries occur due to blunt trauma after: | |||
== | * Motor vehicle accidents<ref name=":0" /><ref name=":1" /><ref name=":6">De Coninck T, Vanhoenacker F, Verstraete K. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6251078/pdf/jbsr-101-2-1401.pdf Imaging features of Morel-Lavallée lesions]. Journal of the Belgian Society of Radiology. 2017;101(Suppl 2).</ref><ref name=":5" /><ref name=":7">Badjate DM, Jain D, Phansopkar P, Wadhokar OC. [https://www.cureus.com/articles/109372-a-physical-therapy-rehabilitative-approach-in-improving-ac_1 A Physical Therapy Rehabilitative Approach in Improving Activities of Daily Living in a Patient With Morel-Lavallée Syndrome: A Case Report]. Cureus. 2022 Sep 24;14(9).</ref> | ||
* Falls<ref name=":0" /><ref name=":5" /><ref name=":7" /> | |||
* Sport-related injuries<ref name=":0" /> <ref name=":1" /><ref name=":5" /><ref name=":7" /> | |||
MLL can also be iatrogenic e.g. after abdominal liposuction or mammoplasty<ref name=":0" /><ref name=":1" /><ref name=":5" /> | |||
== Pathophysiology == | |||
[[File:Morel-lavallee-illustrations.jpg|thumb|450x450px|Case courtesy of Dr Matt Skalski, <a href="https://radiopaedia.org/?lang=us">Radiopaedia.org</a>. From the case <a href="https://radiopaedia.org/cases/22762?lang=us">rID: 22762</a>]] | |||
MLL occurs due to shearing forces which separate the skin and subcutaneous tissue from the deep fascia, causing a potential space<ref name=":0" /><ref name=":1" /><ref name=":3" /><ref name=":4" /><ref name=":6" /><ref name=":8">Weiss NA, Johnson JJ, Anderson SB. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4427222/pdf/wjem-16-438.pdf Morel-lavallee lesion initially diagnosed as quadriceps contusion: ultrasound, MRI, and importance of early intervention]. Western Journal of Emergency Medicine. 2015 May;16(3):438.</ref><ref name=":9">Cruz N, Jiménez R. [https://reader.elsevier.com/reader/sd/pii/S2210261221002340?token=C80C41D90F7CEE3ACB97BCC5E93E1B4C35747C6360CCC9420F281E1AAAB782FC4FE027E1EABB65CE512F7BAB5AF7354A&originRegion=eu-west-1&originCreation=20221125082018 Morel-Lavallée lesion diagnosed 25 years after blunt trauma]. International Journal of Surgery Case Reports. 2021 Apr 1;81:105733.</ref>. Damage to the lymphatic and blood vessels leads to an accumulation of blood and lymph<ref name=":0" /><ref name=":2" /><ref name=":3" /><ref name=":6" /><ref name=":8" /> and necrotic fat<ref name=":0" /><ref name=":2" /><ref name=":6" /><ref>Cochran GK, Hanna KH. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5207285/pdf/10.1177_1558944716646776.pdf Morel-Lavallee lesion in the upper extremity.] Hand. 2017 Jan;12(1):NP10-3.</ref> in the potential space, causing a haematoma or seroma<ref name=":8" />. Blood will start to be reabsorbed over time leaving a serosanguinous fluid surrounded by a haemosiderin layer<ref name=":1" />. Inflammation is then induced by the haemosiderin layer leading to a fibrous capsule<ref name=":1" /><ref name=":9" />. This fibrous capsule prevents more fluid reabsorption, initiating a chronic MLL<ref name=":2" />. | |||
MLL are often associated with pelvic or acetabular fractures but can also occur without a fracture<ref name=":7" />. | |||
Secondary risk factors for an MLL include female gender and BMI of over 25<ref name=":0" />. | |||
== Clinical Presentation == | == Clinical Presentation == | ||
MLL occurs most commonly over the greater trochanter (>60% of cases) (1,2,5,6,8,11), proximal femur (2,5,1,), buttock (2,3,6), knee (2,6,8,11) and in rare cases, the lumbar region (2,3,6,11). It can also occur at the scapula (3,8). Delayed presentation (months or years) can occur in up to ⅓ of patients (1,5). The most common signs and symptoms include: | |||
* Pain (1,3,,45) | |||
* Swelling (1,4,5) | |||
* Stiffness (6,13) | |||
* Cutaneous anaesthesia or hypothesia may be present (1,3,4,5) | |||
* Ecchymosis may be present (13) | |||
* Abrasions may be present (13) | |||
* Secondary dermal changes e.g. discolouration, frank necrosis, drying/cracking (1,13) | |||
* Compressible, fluctuant swollen area (1,3,5,6,13). The fluctuant swelling is an essential clinical characteristic (13) | |||
== Complications == | |||
The necrotic tissue associated with the MLL is particularly susceptible to infection(2) and if infection occurs, it can lead to | |||
* Cellulitis (2) | |||
* Abscess (2) | |||
* Osteomyelitis (2) | |||
* Necrosis of underlying tissues due to pressure (13) | |||
== Diagnostic Procedures == | |||
add text here relating to diagnostic tests for the condition<br> | |||
== Management / Interventions<br> == | == Management / Interventions<br> == | ||
Revision as of 10:26, 25 November 2022
Definition[edit | edit source]
A Morel-Lavallée lesion (MLL) was first described in 1853[1] [2]. It is a closed soft-tissue degloving injury[1][3][4][5][6] that usually occurs after blunt trauma[1][2][3][5]. In recent literature, it can also be referred to as Morel-Lavallée seroma or effusion, post-traumatic soft tissue cysts or post-traumatic extravasations[2].
Epidemiology and aetiology[edit | edit source]
These injuries are uncommon[2] and there is no consensus on the ratio of men to women. One source reported a 2:1 ratio[2] while another reported a 1:1 ratio[7].
These injuries occur due to blunt trauma after:
MLL can also be iatrogenic e.g. after abdominal liposuction or mammoplasty[1][2][6]
Pathophysiology[edit | edit source]
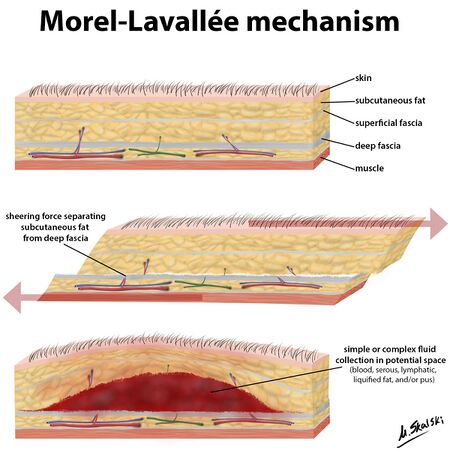
MLL occurs due to shearing forces which separate the skin and subcutaneous tissue from the deep fascia, causing a potential space[1][2][4][5][8][10][11]. Damage to the lymphatic and blood vessels leads to an accumulation of blood and lymph[1][3][4][8][10] and necrotic fat[1][3][8][12] in the potential space, causing a haematoma or seroma[10]. Blood will start to be reabsorbed over time leaving a serosanguinous fluid surrounded by a haemosiderin layer[2]. Inflammation is then induced by the haemosiderin layer leading to a fibrous capsule[2][11]. This fibrous capsule prevents more fluid reabsorption, initiating a chronic MLL[3].
MLL are often associated with pelvic or acetabular fractures but can also occur without a fracture[9].
Secondary risk factors for an MLL include female gender and BMI of over 25[1].
Clinical Presentation[edit | edit source]
MLL occurs most commonly over the greater trochanter (>60% of cases) (1,2,5,6,8,11), proximal femur (2,5,1,), buttock (2,3,6), knee (2,6,8,11) and in rare cases, the lumbar region (2,3,6,11). It can also occur at the scapula (3,8). Delayed presentation (months or years) can occur in up to ⅓ of patients (1,5). The most common signs and symptoms include:
- Pain (1,3,,45)
- Swelling (1,4,5)
- Stiffness (6,13)
- Cutaneous anaesthesia or hypothesia may be present (1,3,4,5)
- Ecchymosis may be present (13)
- Abrasions may be present (13)
- Secondary dermal changes e.g. discolouration, frank necrosis, drying/cracking (1,13)
- Compressible, fluctuant swollen area (1,3,5,6,13). The fluctuant swelling is an essential clinical characteristic (13)
Complications[edit | edit source]
The necrotic tissue associated with the MLL is particularly susceptible to infection(2) and if infection occurs, it can lead to
- Cellulitis (2)
- Abscess (2)
- Osteomyelitis (2)
- Necrosis of underlying tissues due to pressure (13)
Diagnostic Procedures[edit | edit source]
add text here relating to diagnostic tests for the condition
Management / Interventions
[edit | edit source]
add text here relating to management approaches to the condition
Differential Diagnosis
[edit | edit source]
add text here relating to the differential diagnosis of this condition
Resources
[edit | edit source]
add appropriate resources here
References[edit | edit source]
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 Diviti S, Gupta N, Hooda K, Sharma K, Lo L. Morel-Lavallee lesions-review of pathophysiology, clinical findings, imaging findings and management. Journal of clinical and diagnostic research: JCDR. 2017 Apr;11(4):TE01.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 Singh R, Rymer B, Youssef B, Lim J. The Morel-Lavallée lesion and its management: a review of the literature. Journal of orthopaedics. 2018 Dec 1;15(4):917-21.
- ↑ 3.0 3.1 3.2 3.3 3.4 Zairi F, Wang Z, Shedid D, Boubez G, Sunna T. Lumbar Morel-Lavallée lesion: case report and review of the literature. Orthopaedics & Traumatology: Surgery & Research. 2016 Jun 1;102(4):525-7.
- ↑ 4.0 4.1 4.2 LaTulip S, Rao RR, Sielaff A, Theyyunni N, Burkhardt J. Ultrasound utility in the diagnosis of a Morel-Lavallée lesion. Case Reports in Emergency Medicine. 2017 Feb 1;2017.
- ↑ 5.0 5.1 5.2 Depaoli R, Canepari E, Bortolotto C, Ferrozzi G. Morel-Lavallée lesion of the knee in a soccer player. Journal of ultrasound. 2015 Mar;18(1):87-9.
- ↑ 6.0 6.1 6.2 6.3 6.4 Mettu R, Surath HV, Chayam HR, Surath A. Chronic Morel-Lavallée lesion: a novel minimally invasive method of treatment. Wounds. 2016 Nov 1;28(11):404-7.
- ↑ Christian D, Leland HA, Osias W, Eberlin S, Howell L. Delayed presentation of a chronic Morel-Lavallee lesion. Journal of Radiology Case Reports. 2016 Jul;10(7):30.
- ↑ 8.0 8.1 8.2 8.3 De Coninck T, Vanhoenacker F, Verstraete K. Imaging features of Morel-Lavallée lesions. Journal of the Belgian Society of Radiology. 2017;101(Suppl 2).
- ↑ 9.0 9.1 9.2 9.3 Badjate DM, Jain D, Phansopkar P, Wadhokar OC. A Physical Therapy Rehabilitative Approach in Improving Activities of Daily Living in a Patient With Morel-Lavallée Syndrome: A Case Report. Cureus. 2022 Sep 24;14(9).
- ↑ 10.0 10.1 10.2 Weiss NA, Johnson JJ, Anderson SB. Morel-lavallee lesion initially diagnosed as quadriceps contusion: ultrasound, MRI, and importance of early intervention. Western Journal of Emergency Medicine. 2015 May;16(3):438.
- ↑ 11.0 11.1 Cruz N, Jiménez R. Morel-Lavallée lesion diagnosed 25 years after blunt trauma. International Journal of Surgery Case Reports. 2021 Apr 1;81:105733.
- ↑ Cochran GK, Hanna KH. Morel-Lavallee lesion in the upper extremity. Hand. 2017 Jan;12(1):NP10-3.






