Metatarsus Adductus
Introduction[edit | edit source]
Metatarsus adductus (MA) is cited in a 1994 article by F R Dietz [1] as the most common congenital foot deformity in newborns. In a 2019 article by Rampal and Giuliano, it was stated as occurring in 0.2% of births.[2]
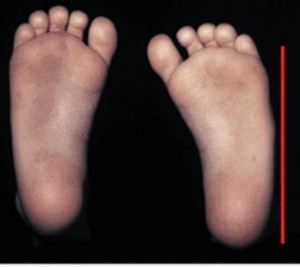
MA is a deformity occurring only in the transverse plane of the foot.[2] In appearance, MA is seen as an adduction deformity or medial deviation of the forefoot at the tarsometatarsal joints (Lisfranc joint) with respect to the hindfoot.[1] [3]. This occurs in association with soft tissue contractures. Metatarsal deviation occurs in the the transverse plane with a convex lateral border of the foot and prominent styloid process.[4]The foot therefore is observed as 'C' shaped.
Clinically Relevant Anatomy[edit | edit source]
See: Basic Structure of the Foot and Ankle
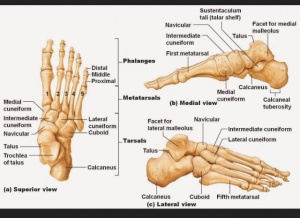
Metatarsals
Lisfranc joint
Forefoot and hind foot
Hindfoot is comprised of : Tibiofibular joint , Talocular joint and the Subtalar (Talocalcanean) joint.[5]
Midfoot (Midtarsal Joints) is comprised of: Talocalcaneonavicular Joint, Cuneonavicular Joint, Cuboideonavicular Joint, Intercuneuform Joints, Cuneocuboid joint and the Calcaneocuboid Joint.[5]
Forefoot is comprised of: Tarsometatarsal Joints, Intermaetatarsal Joint, Metatarsophalangeal Joints and Interphalangeal Joints.[5]
It is caused by in-utero position and constriction of the fetus.[6]It is also called as pigeon toes.
The child having this deformity walks with an in-toe gait during early infancy.[6]
In many cases it is self limiting too.[7]
Types[edit | edit source]
Metatarsus Adductus may be classified as:
Flexible: Presents with adduction of the 5 metatarsal bones at the tarsometatarsal joint.
Rigid: Presents with medial subluxation of the tarsometatarsal joints. There is valgus of the hindfoot and the navicular is later to the head of the talus.
Classification[edit | edit source]
By Bleck [8]
Grade 1[edit | edit source]
Adduction of the forefoot without inversion and passive abduction is possible either manually or by the means of electrical stimulation.
Grade 2[edit | edit source]
The foot is shortened a bit. The forefoot is in adduction and inversion. The external border of the foot is convex whereas the internal border is concave. The base of the fifth metatarsal is prominent. This can be partially corrected.
Grade 3[edit | edit source]
This consist of a structural deformity where the length of the foot is shortened. Surgical correction is the only option in this grade.
Transverse sulci is in medial region of the foot, increased internal longitudinal arc. Passive correction is not possible.
Epidemiology and Etiology[edit | edit source]
There is an incidence of 1 in 100 to 1 in 5,000 live births.[9] The cause of metatarsus adductus remains unknown. It is however, thought to be related to intrauterine compression. Family history may also be a causative factor. Other theories of causal relation includes abnormal tendon insertion of tibialis anterior, tibialis posterior and abductor hallucis muscles.[10]
Clinical Presentation[edit | edit source]
The forefoot is adducted and sometimes supinated, but the midfoot and hindfoot are normal. There is the convexity of the lateral border of the foot, with the concavity of the medial border. Older children may present with an in-toeing gait.
Diagnostic Procedures[edit | edit source]
Transmalleolar Axis Bisector[edit | edit source]
This is a geometric tool used to do the clinical assessment of Metatarsus Adductus.
Heel bisector line[edit | edit source]
This was discovered by Bleck. It was used to assess the severity of Metatarsus adductus and even used as a treatment outcome measure of stretching applied for this condition.
This is a simple measure that assesses the flexibility and severity of the metatarsus adductus. It is a manual assessment and no types of equipment are needed.[7]
Management / Interventions[edit | edit source]
This condition mostly doesn't require any form of treatment and resolves on its own. The conditions like cerebral palsy, spina bifida, Slipped capital femoral epiphysis, congenital displacement of the hip, and metabolic disorders like rickets, osteogenesis imperfecta needs to be ruled out.[11]
Specific treatment for metatarsus adductus is often determined by the following factors:
- Child's Age
- Medical History
- The extent of the condition
- Tolerance for the specific procedure
- Expectations for the condition
Interventions include:[edit | edit source]
- Passive Stretching
- Passive Manipulation exercises
- Stretching
- Serial Casting
- Footwear
- Surgery to release the joints
Prognosis[edit | edit source]
Generally excellent. Most cases of metatarsus adductus often resolves on its own
References[edit | edit source]
- ↑ 1.0 1.1 Dietz FR. Intoeing--fact, fiction and opinion. American Family Physician. 1994 Nov 1;50(6):1249-59.
- ↑ 2.0 2.1 Rampal V, Giuliano F. Forefoot malformations, deformities and other congenital defects in children. Orthopaedics & Traumatology: Surgery & Research. 2020 Feb 1;106(1):S115-23.
- ↑ 3.0 3.1 Alonge VO. Proposing Transmalleolar Axis Bisector (TMAB) as a Geometrically Accurate Alternative to the Heel Bisector Line for the Clinical Assessment of Metatarsus Adductus. Int J Foot Ankle. 2020;4:041.
- ↑ Marshall N, Ward E, Williams CM. The identification and appraisal of assessment tools used to evaluate metatarsus adductus: a systematic review of their measurement properties. Journal of foot and ankle research. 2018 Dec;11(1):1-0.
- ↑ 5.0 5.1 5.2 Magee, D. J. (2008). Orthopedic physical assessment. St. Louis, Mo: Saunders Elsevier.
- ↑ 6.0 6.1 Merens TA. The toddler gait—normal or not. Pediatric Annals. 2015 May 1;44(5):187-90.
- ↑ 7.0 7.1 Marshall N, Ward E, Williams CM. The identification and appraisal of assessment tools used to evaluate metatarsus adductus: a systematic review of their measurement properties. Journal of foot and ankle research. 2018 Dec;11(1):1-0.
- ↑ Bleck EE. Metatarsus adductus: classification and relationship to outcomes of treatment. Journal of pediatric orthopedics. 1983 Feb 1;3(1):2-9.
- ↑ Wildhe T.Foot deformities at birth: a longitudinal prospective study over a 16 year period. J Pediatric Orthopedic. 1997;17(1):20-24
- ↑ Hassan N, Roger J (2015) Management of Metatarsus Aductus, Bean-Shaped foot, residual clubfoot adduction and Z-shaped foot in children, with conservative treatment and and double column osteotomy of the first cuneiform and cuboid. Ann Orthop Rheumatol3(3):1050.
- ↑ Berry KM. Evidence-Based Management of In-Toeing in Children. Clinical Pediatrics. 2018 Oct;57(11):1261-5.