Metacarpal Fractures
Original Editor - --Marie Avau , Debby Decock, Farrie Bakalli, Margaux Jacobs
Introduction[edit | edit source]
Hand fractures are common in the general population with relative propensity seen in contact-sport athletes (e.g., boxers, football players) and manual laborers[1]
A metacarpal fracture
- Is a break in one of the five metacarpal bones of either hand.
- Are categorized as being fractures of the head, neck, shaft, and base (from distal at the metacarpal phalangeal joint to proximal at the wrist).[2] [3]
- Boxer fracture is another name for a fracture of the fourth or fifth metacarpal, one of the most common metacarpal fractures. [3]
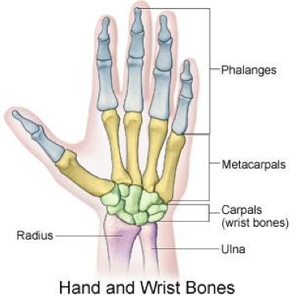
Clinically Relevant Anatomy[edit | edit source]
The hand is composed of 19 bones (5 metacarpals and 14 phalanges), more than 30 tendinous insertions and numerous complex structures.
The metacarpals are long, thin bones which are located between the carpal bones in the wrist and the phalanges in the digits.[4][4]
- Each are comprised of a base, shaft, and head.
- The proximal bases of the metacarpals articulate with the carpal bones,
- Distal heads of the metacarpals articulate with the proximal phalanges and form the knuckles.
- The 1st metacarpal is the thickest and shortest of these bones.
- The 3rd metacarpal is distinguished by a styloid process on the lateral side of its base.
- Soft tissues generally involved with fractures include cartilage, joint capsule, ligaments, fascia, and the dorsal hood fibers.
- With severe polytrauma cases, the tendons and nerves adjacent to the fracture can also be injured. [5]
Etiology[edit | edit source]
Metacarpal fractures typically occur secondary to a direct blow or fall directly onto the hand.
- These fractures commonly occur during athletic activities, particularly in contact sports. Almost one-fourth of cases occur during athletic events.
- Sporting injury is frequently the cause among younger patients
- Work-related injuries are often the cause in middle-aged patients
- Falls are typically the cause in the elderly.
- Fifth metacarpal fractures often occur secondary to punching a wall or other solid object (hence the eponym, "boxer's fracture")[1]
Hand fractures
- make up about 40% of all acute hand injuries
- Constitute about 20% of all fractures occurring below the elbow
Metacarpal fractures
- Typically occur in patients aged 10-40 years
- Men are more likely to be affected than women.
- Young men sustain metacarpal fractures secondary to a punching mechanism or a direct blow to the hand
- Geriatric females sustain these injuries secondary to a low energy fall.
- The incidence rate of fracture seen in association with each digit's metacarpal bone increases from the radial to the ulnar side.
- The incidence rate of 2nd metacarpal fractures is lower than the incidence rate of 5th metacarpal fractures.[1]
- The thumb metacarpal fractures, which is the most common fracture type, are usually caused by an axial blow directed against the partially flexed metacarpal. (It is estimated to occur in 4% of hand fractures. These fractures are called Boxer's fractures and received their name from one of their most common causes of punching an object with a closed fist. This occurs commonly during fist fights or from punching a hard object such as a wall or filing cabinet. Although these breaks usually occur when the hand is closed into a fist, they can also occur when the hand is not clenched and strikes a hard object.[2]
The fractures of the metacarpals can be divided in three parts.
- The first, neck fractures, occurs often when a person punches another person or object. In the majority of cases, surgical intervention is not essential to treat this condition.
- The metacarpal shaft fractures are often produced by longitudinal compression, torsion or direct impact. They are described by the appearance of their respective fracture patterns and can be divided by transverse, oblique, spiral and comminuted.
- Metacarpal base fractures are rare and have minimal consequence because the motion of the joint is small. More common are the fractures of the base of the fifth digit and are the result of a longitudinally directed force [6]
Characteristics/Clinical Presentation[edit | edit source]
Patients with metacarpal fractures generally present with: [5][7]
- Pain
- Swelling
- Ecchymosis (bruise)
- Limitation of movement
- Deformity. Knuckle asymmetry may be observed, and the knuckle may appear to be missing.
- Finger misalignment may also be noted.
- A metacarpal head fracture is associated with axial compression of the extended digit which causes severe discomfort.
- In a metacarpal base fracture, movement of the wrist or longitudinal compression exacerbates the pain.
- Any metacarpal fracture angulation can produce a pseudo-claw deformity.
Differential diagnosis[edit | edit source]
Injuries to neighboring bones (carpal bones, phalanges) and associated soft tissues (ligaments, tendons) need to be excluded.
Evaluation[edit | edit source]
The evaluation includes:
- Standard radiographs of the hand (anteroposterior, lateral, and oblique). In the vast majority of cases, this will be enough to confirm the diagnosis and form a management plan. Confirmation of more subtle injuries can be obtained using special views such as Brewerton (metacarpal heads), Roberts, and Betts (thumb) views.
- CT is sometimes necessary for the base of metacarpal fractures to check for any intra-articular displacement and determine if there is a need for surgery
Outcome Measures[edit | edit source]
- Grip Strength: measured with a dynamometer
- Range of motion
- Patient Specific Functional Scale
- DASH
- Michigan Hand Outcome Questionnaire (MHO): In this questionnaire they asses 6 criteria for people with a hand disorder: overall hand function, activities of daily living (ADL), pain, work performance, aesthetics, and patient satisfaction with hand function. [3][8]
Medical management[edit | edit source]
The goal of treatment is a restoration of anatomy and function.
- Antibiotics and tetanus prophylaxis are options for open fractures as per standardized guidelines.
- The modality of treatment will vary depending on skin integrity (open versus closed fracture), the number of digits/metacarpals fractured, the stability of the specific, degree of comminution, displacement, and/or rotational malalignment
- In general, increasing degrees of displacement, comminution, and rotational malalignment are critical factors in assessing the fracture patterns potential for stability and reduction maintenance with nonoperative management.[1]
- The GP/Specialist after assessing the fracture will perform gentle tests and imaging to work out if surgery is needed.
- If surgery is not needed a physiotherapist will make a custom splint, which will support the healing fracture.
Physical Therapy Management[edit | edit source]
Full strength and range of motion is the goal of rehabilitation.
Under physiotherapist’s instructions
- Hand exercises with light resistance such as rubber bands or squeeze ball can help if there is scarring or extensor lag develops.
- Soft tissue recovery may be more of a problem than the bony one.
- Rest and elevation are important, and so is the quality of splinting - poor splinting can cause stiffness, pressure sores, or even compartment syndrome
Physiotherapists use a number of techniques to regain movement in the hand, wrist and fingers, including:
- swelling management with massage and compression garments
- soft tissue massage to help with muscle tension and pain
- providing client with a home exercises program of specific movements and strengthening exercises.
Most hand fractures can be treated non-operatively [4] This very informative 4 minute video gives a basic run done on Physio treatment
More specific Advice.
These are the steps to be followed in a stable fracture: [10]
- Buddy strapping the injured digit to another digit is used as a non-operative technique. This is used with or without the application of varying degrees of splint. The ‘buddy’ reduces the risk of rotational deformity. The splinting of the fracture should be with an aim if 20 degrees wrist extension, the metacarpophalangeal joint in 60-70 degree flexion and interphalangeal joint extension [11]
- Early motion is generally considered appropriate when there are stable fractures or rigid fractures. It is hypothysed that early motion has the potential for improved outcomes.[12]
- Generally AROM (active ROM) exercises without resistance can begin 2 to 3 weeks after operative treatment in uninvolved or bordering/adjacent joints. [7](Stern PJ., level of evidence 5), [5] [6] [2]
- Active Motion: If the fracture is internally fixed, the active range of motion can start early. Most fractures are treated by immobilization, but the active motion can begin after three weeks of therapy, starting with the joints not splintered during the initial immobilization. This phase usually lasts 3-6 weeks. [2] [3] [10][11]
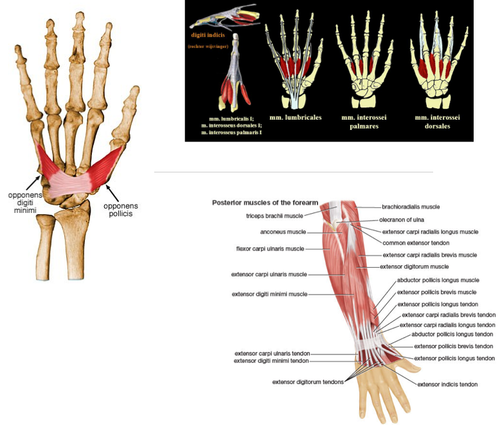
- Specific tendon gliding should be included in the active motion. The following muscles should be involved: m. flexor digitorum profundus, m. flexor digitorum superficialis, m., extensor digitorum communis, m. extensor indicis propius and m. extensor digiti minimi
- Tendon gliding is important to prevent adhesions,increased circulation about the fracture site, decreased edema and compression at the fracture site.
FDP tendons and selected tendon glide should be performed by actively flexing the injured PIP joint while positioning the other DIP joints in extension. The EI and EDQ tendons should glide on the adjacent EDC tendon and the EDC tendons on the underlying bone. By extending the MPC joints while IP joints are flexed, tendon gliding of the EDC tendon should be performed.
Exercises for tendon gliding :
A : Claw posture to achieve extensor digitorum communis tendon glide over metacarpal bone
B : Intrinsic plus posture to achieve central slip. Lateral bands glide over proximal phalanx 1
C : Flexor digitorum profundus (FDP) blocking exercises to glide FDP tendon over phalanx 1
D : Hook fist posture to promote selective FDP tendon glide
E : Flexor digitorum sublimis blocking exercise to glide FDS tendon over middle phalanx
F : Sublimis fist posture to promote selective FDS tendon glide
[10]
- Passive Motion: Passive motion can be initiated during the repair phase, when callus is starting to form. This motion will stimulate bone and cartilage healing. The passive range of motion (PROM) can be divided in physiological motion or arthrokinematic motion. Passive motion can be initiated after sufficient clinical healing at approximately 5-6 weeks of therapy. [2] [8] , [3]
- Once the therapist knows the location of the fracture, joint mobilization can be started. It is preferable to applicate arthrokinematic motion before traditional PROM. The force in physiological PROM is applied at a distance from the joint axis of motion, which can be produced extra load around the fracture site. For arthrokinematic motion, the force is directed perpendicular to the joint surface, which is not stressing the fracture site.
- The timing of initiation of joint mobilization depends on the structures involved in the injury. If the structures resisting the force are not involved in the injury, joint mobilization can be initiated at the same time as active motion. Compression on the fracture can result in shortening, angulation or rotational malalignment of the bone.
- Traditional PROM aims to assist in articular cartilage healing, reduce swelling and stiffness. Continuous passive motion (CPM) is a form of PROM. It applies force through the phalanx, thus applies a torque to the fracture site. CPM has the potential to decrease edema and improve synovial fluid production. CPM can be applied as soon as traditional PROM is allowed. However, Continuous passive motion can never replace active and resistive exercise and the application of CPM should not be painful.
Important to know is that a full PROM is necessary before full AROM and ultimate function of the hand can be achieved. [4] - Resistive Motion: Four weeks after the injury light resistance can be performed in most metacarpal fractures which are treated by immobilization. Active motion should only be continued if healing has not started. Resistive exercise should also be delayed when a fracture is fixed by pinning until these pins are removed, to ensure stability of the fracture. Light resistive exercise helps with scar remodeling and improved motion. There are several types pf resistive exercises such as the weight-well exercises. This kind of exercise strengthens the finger flexors (FDP and FDS muscles).
- Functional activities and work simulation should be included in the resistive exercises as soon as possible.[10]
Key research[edit | edit source]
Hardy MA. Principles of Metacarpal and Phalangeal Fracture Management: A Review of Rehabilitation Concepts. Journal of Orthopedic and Sports Physical Therapy. 2004; 34:781-791.
Resources[edit | edit source]
Hand and Metacarpal Fractures
Bennett's fracture
http://www.sciencedirect.com.ezproxy.vub.ac.be:2048/science/article/pii/S089411300380011X
https://www.youtube.com/watch?v=uWQtpqXRx-w
http://www.physioadvisor.com.au/14681850/metacarpal-fracture-physioadvisor.htm
http://www.orthobullets.com/hand/6037/metacarpal-fractures
http://medical-dictionary.thefreedictionary.com/fracture+of+fifth+metacarpal
http://www.journalagent.com/pubmed/linkout.asp?ISSN=1306-696X&PMID=20849050
http://www.webmd.com/a-to-z-guides/boxers-fracture?print=true
Clinical Bottom Line[edit | edit source]
Bottom line (=The main or essential point)
A metacarpal fracture is a break in one of the five metacarpal bones of either hand. It is categorized as being head fractures, neck fractures, shaft fractures and base fractures. These fractures can either be displaced or non- displaced. The main cause of most metacarpal fractures of the fingers is a direct forceful blow on the fingers. Each fracture-type has specific clinical presentation.
In some cases, there may be a wrong diagnosis for a metacarpal fracture because other disorders often present the same symptoms. Because of that, it is necessary to submit the patient to a physical examination and radiograph. By taking several X-rays of the hand, the severity of the fracture can be evaluated.https://www.youtube.com/watch?v=uWQtpqXRx-w
Medical treatment must not sacrifice the hand functions. The primary goals of medical management are to achieve anatomic and stable reduction, bony union, and early mobilization to minimize disability. Knowledge of the relevant anatomy, acting muscular forces and the mechanisms of fractures is required to choose the appropriate treatment.
The intervention of the physical therapist consist of applying strength exercises or guide the healing process by using a splint. Alongside of the improved functionality, active, passive and resistive exercises also affect the recovery process.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Moore A, Varacallo M. Metacarpal hand fracture. InStatPearls [Internet] 2019 Jan 16. StatPearls Publishing.Available from:https://www.ncbi.nlm.nih.gov/books/NBK536960/ (last accessed 6.4.2020)
- ↑ 2.0 2.1 2.2 2.3 2.4 http://www.physioadvisor.com.au/14681850/metacarpal-fracture-physioadvisor.htm (level of evidence 5)
- ↑ 3.0 3.1 3.2 3.3 3.4 Blomberg J, Metacarpal fracture, Orthobullets & oral boards, 2014 (level of evidence 5)
- ↑ 4.0 4.1 4.2 4.3 Rafael D. Et al., Current management of metacarpal fractures, hand the clinics, 2013 (level of evidence 5)
- ↑ 5.0 5.1 5.2 Hardy MA. Principles of Metacarpal and Phalangeal Fracture Management: A Review of Rehabilitation Concepts. Journal of Orthopedic and Sports Physical Therapy. 2004; 34:781-791.(level of evidence 5)
- ↑ 6.0 6.1 Kathleen M. Kollitz et. Al., Metacarpal fractures: treatment and complication, American Association for Hand Surgery 2013, Springer, Published online: 16 October 2013, HAND (2014) 9:16–23
- ↑ 7.0 7.1 Michael DelCore ,Metacarpal fractures, orthopaedicsone ,2015.
- ↑ 8.0 8.1 Karriem-Norwood, Boxers fracture, webmd , 2014
- ↑ Medicine in a nutshell Physio excercises for patients with metacarpal fractures Available from:https://www.youtube.com/watch?v=1xrlrp8Ooa0&feature=youtu.be (last accessed 6.4.2020)
- ↑ 10.0 10.1 10.2 10.3 T. GRANT PHILLIPS, M.D. et al, Diagnosis and Management of Scaphoid Fractures, Washington Hospital Family Practice Residency, Washington, Pennsylvania, 2004.http://coruraltrack.org/wp-content/uploads/2013/01/Scaphoid-Fractures-AFP.pdf
- ↑ 11.0 11.1 Tiel-van Buul MM et al, The value of radiographs and bone scintigraphy in suspected scaphoid fracture. A statistical analysis. J Hand Surg [Br] 1993;18:403-6.
- ↑ J. J. de Jongel et al, Fractures of the metacarpals. A retrospective analysis of incidence and aetiology and a review of the English-language literature, ‘Department of Traumatology, and ‘Department of Plastic and Reconstructive Surgery, University Hospital Groningen, The Netherlands. Injury, 1994, Vol. 25, 365-369, August.