Medical Cannabis
Original Editors -Mark Wojda from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Ryan Scinta, Lucinda hampton, Elaine Lonnemann, Kim Jackson, Ryan Barry, WikiSysop, Mark Wojda and Joseph Ayotunde Aderonmu
Introduction[edit | edit source]
C. sativa is a flowering, fast growing shrub, commonly known as hemp, cannabis, or marijuana. It originates from Central Asia, and is widely distributed in temperate and tropical areas. For thousands of years, Cannabis sativa has been utilized as a medicine and for recreational and spiritual purposes. Phytocannabinoids are a family of compounds that are found in the cannabis plant, which is known for its psychotogenic and euphoric effects; the main psychotropic constituent of cannabis is THC. The pharmacological effects of cannabinoids are a result of interactions between those compounds and cannabinoid receptors, CB1 and CB2, located in many parts of the human body[1].
- Many people around the world believe that the drug should be readily available for both medical and recreational use; however governments around the world still have strict laws about its usage.
- Each country has its own laws and regulations surrounding the drug; some places are more relaxed, whist others still believe the drug should be an illegal substance[2].
Cannabidiol (CBD), the major non-psychoactive constituent of Cannabis sativa L., has gained traction as a potential treatment for:certain conditions.
- At present, the evidence base for the use of medicinal cannabis products is limited. The current evidence base for the use of medicinal cannabis products is heterogeneous, comprising a small number of randomised clinical trials when stratified by condition, symptom or intervention type. These studies are of variable quality, including those with high risk of bias (eg incomplete outcome data), low statistical power, and short follow-up time.
- Recent reviews and analyses indicate there may be some therapeutic benefits of medicinal cannabis products in certain conditions but further research on the treatment efficacy and longer term side effects are warranted.
- Currently, most research and evidence on medicinal cannabis products have come from five clinical conditions: multiple sclerosis; palliative care; epilepsy; nausea and vomiting; and chronic non-cancer pain. [3]
Types of medicinal cannabis products[edit | edit source]
Cannabis is a complex plant comprising more than 500 constituents, including approximately 100 cannabinoids. The main active ingredients used for medical purposes are tetrahydrocannabinol (THC) and cannabidiol (CBD). THC is the psychoactive part of cannabis that produces a ‘high’, and has been used to treat symptoms such as nausea, pain and muscle spasticity. CBD has no psychoactive properties, and has been used to treat several inflammatory disorders and epilepsy.
Medicinal cannabis products can come in three main forms:
- Pharmaceutical: Natural and synthetic medical-grade products with standardised content. The three main products are:
- Dronabinol: Synthetic form of THC
- Nabilone: Synthetic form of THC
- Nabiximols: Chemically pure 50:50 mixture of TCH and CBD.
- Medicinal-grade herbal cannabis: Produced and processed in controlled standard conditions to a medical grade, free of adulterants, higher levels of CBD and other cannabinoids, and contains lower levels of THC. This is provided in herbal form, or processed as an oil, balm, capsule or pill.
- Herbal cannabis on the illegal market: Potentially unstable THC and CBD, and may contain adulterants.[3]
Chronic Pain[edit | edit source]
The International Association for the Study of Pain taskforce looked at all the available research published in peer-reviewed journals on the use of medicinal cannabis for pain management, from preclinical studies to human trials.
They concluded overall the studies’ “quality, rigour, and transparency of reporting” of benefits and harms needs to be improved across the board. We would require higher quality data, for example through randomised controlled trials, to determine the safety and efficacy of using medicinal cannabis for pain[4]
Epilepsy[edit | edit source]
A number of studies have found low evidence for the use of medicinal cannabis products for the treatment of paediatric epilepsy, and for patients up to aged 25 years, especially when first-line treatments (ie anti-epileptic drugs) have been found to be ineffective. The numbers needed to treat are as follows:
- 50% or greater reduction in seizure frequency: 8
- Complete seizure freedom: 17
- Improvement in parental-reported quality of life: 5
- The numbers needed to harm for any adverse event was 3, and serious adverse event was 23.
Palliative care[edit | edit source]
The use of medicinal cannabis products in palliative care is currently unclear.
Nausea and vomiting[edit | edit source]
A small number of studies have found relief of nausea and vomiting in patients with cancer who are undergoing chemotherapy; however, the evidence is lacking and some were compared with now out-of-date practices.
Chronic non-cancer pain[edit | edit source]
There is some evidence available for the treatment of neuropathic pain using medicinal cannabis products; however, the magnitude of effect is small.10 One systematic review found that the numbers needed to treat was 22 for a 30% reduction and 26 for a 50% reduction in self-reported pain intensity
Relevance to Physical Therapy Rehabilitation[edit | edit source]
Since medical and recreational marijuana is becoming legalized in a greater number of states, there is an increased likelihood that physical therapists will treat patients using marijuana to combat different musculoskeletal and neurological conditions. Drug prescription does not fall under the scope of physical therapy practice; therefore, the major role of the therapist is to be an educational resource for patients with questions about the use of medical marijuana. It is recommended that therapists explain the benefits and drawbacks of medical marijuana rather than directly suggesting that the patient initiate using the substance. [5]
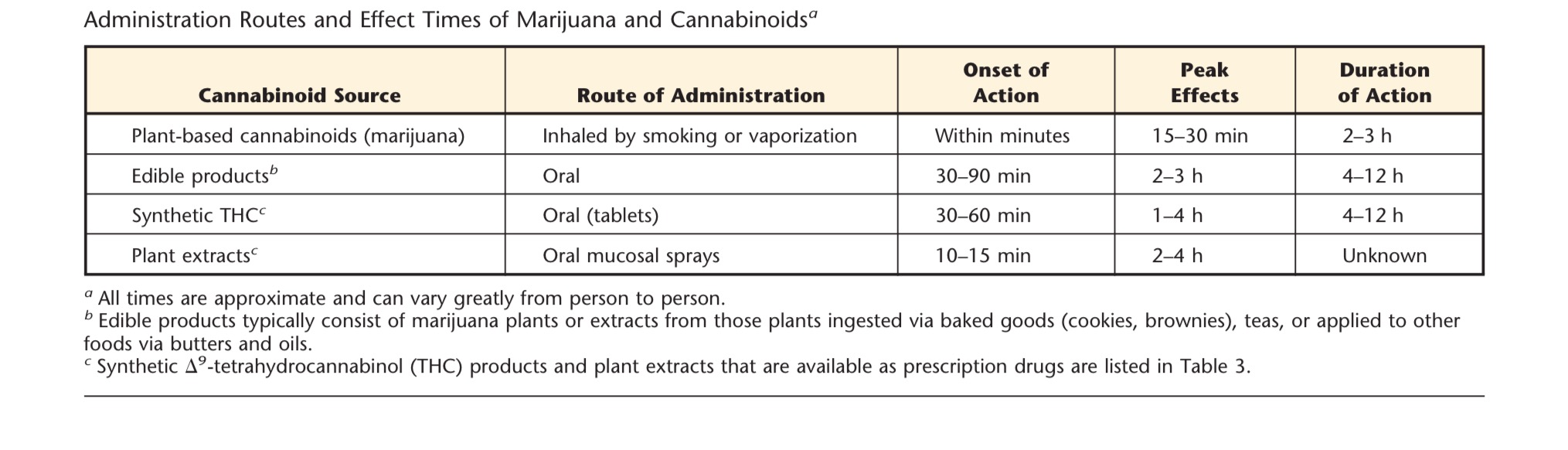
Patients may not be well educated on the different routes of administration of marijuana and its extracts. Below is a chart of different marijuana based products with their associated effect times.
Patients who are known users of medicinal or recreational marijuana for analgesic purposes should be encouraged to keep a pain journal.Therapists should have patients periodically complete valid and reliable pain scales to ensure that the treatment is providing the desirable effects. One of the major roles of the physical therapist is to monitor patients for potential abuse of the substance and/or co-administration with alcohol, benzodiazepines, or opioids. These patients may present with amplified confusion or somnolence and demonstrate personality changes or psychotic-like behaviors. If these signs are noted, the problem should be reports the prescribing physician by the therapist. [5]
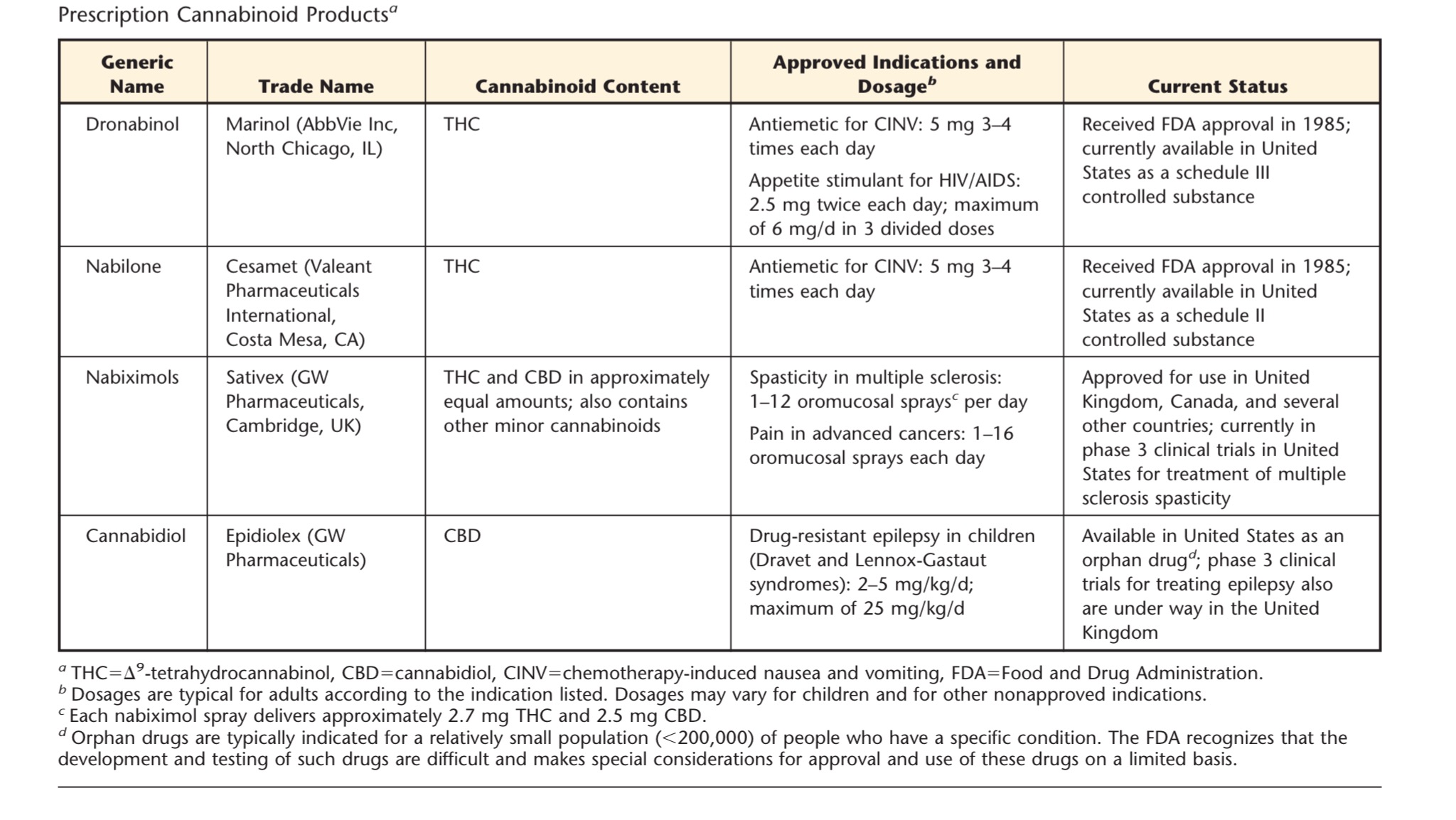
In the table below are several presecribed cannabinoid based medications that have been either been approved by the FDA or are currently under clinical trials. These drugs may start to be prescribed more in the future.
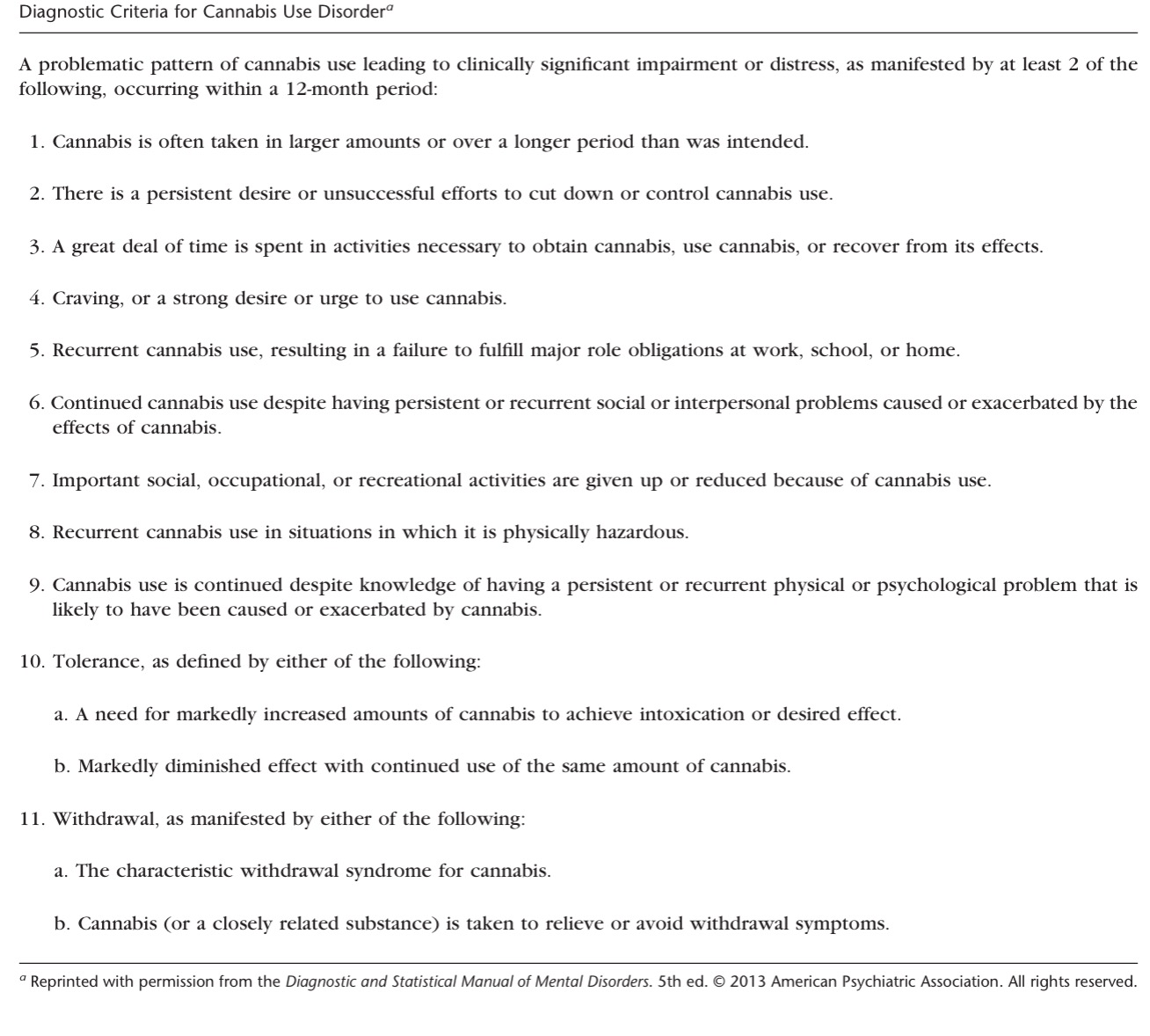
Therapists should also be able to identify patients for Cannabis Use Disorder (CUD). (See diagnostic criteria questionnaire below) Patients using marijuana for the use of chronic pain are less likely to suffer from cannabis use problems compared with individuals who used medical cannabis for other reasons (e.g., anxiety, insomnia, and muscle spasms). [6]
This has been shown to occur primarily in recreational users and risk of this disorder in individuals using medical marijuana has yet to be fully established. [7]
Case Reports/ Case Studies:[edit | edit source]
This page will be continually updated in the future.
HIV:
Woolridge E, Barton S, Samuel J, Osorio J, Dougherty A, Holdcroft A. Cannabis use in HIV for pain and other medical symptoms. J Pain Symptom Manage 2005;29(4):358-67.
http://www.ncbi.nlm.nih.gov/pubmed/15857739
Multiple Sclerosis:
Consroe P, Musty R, Rein J, Tillery W, Pertwee R. The perceived effects of smoked cannabis on patients with multiple sclerosis. European Neurology 1997;38:44-48.
http://www.ncbi.nlm.nih.gov/pubmed/9252798
Chong MS, Wolff K, Wise K, Tanton C, Winstock A, Silber E. Cannabis use in patients with multiple sclerosis. Mult Scler 2006;12(5):646-51.
http://www.ncbi.nlm.nih.gov/pubmed/17086912
Spinal Cord Injury:
Malec J, Harvey RF, Cayner JJ. Cannabis effect on spasticity in spinal cord injury. Archives of Physical Medicine and Rehabilitation 1982;63:116-118.
http://www.ncbi.nlm.nih.gov/pubmed/6978699
Crohn's Disease:
Lal S, Prasad N, Ryan M, Tangri S, Silverberg MS, Gordon A, Steinhart H. Cannabis use amongst patients with inflammatory bowel disease. Eur J Gastroenterol Hepatol 2011;23(10):891-6.
http://www.ncbi.nlm.nih.gov/pubmed/21795981
Resources[edit | edit source]
For information regarding your states cannabis laws:
http://norml.org/
For information regarding which strains you or your patient's are using:
For information regarding cannabis therapeutics for different conditions including veterans:
http://www.safeaccessnow.org/
Realm of Caring: Pediatric Epilepsy
Information on legal issues: Marijuana policy project:
Drug policy information:
References[edit | edit source]
see adding references tutorial.
- ↑ Breijyeh,Z.;Jubeh,B.Bufo, S.A.; Karaman, R.; Scrano, L. Cannabis: A Toxin-Producing Plant with Potential Therapeutic Uses.Toxins 2021, 13, 117. Available from: https://res.mdpi.com/d_attachment/toxins/toxins-13-00117/article_deploy/toxins-13-00117.pdf (accessed 5.4.2021)
- ↑ best in Au Where is cannabis legal Available from:https://bestinau.com.au/marijuana-laws-from-around-the-world-where-is-cannabis-legal/ (accessed 5.4.2021)
- ↑ 3.0 3.1 RACGP Medicinal Cannabis Available from:https://www.racgp.org.au/advocacy/position-statements/view-all-position-statements/clinical-and-practice-management/medical-cannabis (accessed 5.4.2021)
- ↑ IASP Position Statement on the Use of Cannabinoids to Treat Pain Available from:https://www.iasp-pain.org/PublicationsNews/NewsDetail.aspx?ItemNumber=11145&navItemNumber=643 (accessed 5.4.2021)
- ↑ 5.0 5.1 Ciccone CD. Medical Marijuana: Just the Beginning of a Long, Strange Trip? Physical Therapy. 2016;97(2):239–48.
- ↑ Cohen NL, Heinz AJ, Ilgen M, Bonn-Miller MO. Pain, cannabis species, and cannabis use disorders. J Stud Alcohol Drugs. 2016; 77:515–520.
- ↑ Richter L, Pugh BS, Ball SA. Assessing the risk of marijuana use disorder among adolescents and adults who use marijuana.Am J Drug Alcohol Abuse. 2016;13:1–14.