Medical Cannabis: Difference between revisions
No edit summary |
No edit summary |
||
| Line 1: | Line 1: | ||
| | ||
<div class="noeditbox">Welcome to [[Pathophysiology of Complex Patient Problems|PT 635 Pathophysiology of Complex Patient Problems]] This is a wiki created by and for the students in the School of Physical Therapy at Bellarmine University in Louisville KY. Please do not edit unless you are involved in this project, but please come back in the near future to check out new information!!</div><div class="editorbox"> | <div class="noeditbox">Welcome to [[Pathophysiology of Complex Patient Problems|PT 635 Pathophysiology of Complex Patient Problems]] This is a wiki created by and for the students in the School of Physical Therapy at Bellarmine University in Louisville KY. Please do not edit unless you are involved in this project, but please come back in the near future to check out new information!!</div><div class="editorbox"> | ||
'''Original Editors '''- [[Pathophysiology of Complex Patient Problems| | '''Original Editors '''-[http://www.physio-pedia.com/User:Mark_Wojda Mark Wojda] [[Pathophysiology of Complex Patient Problems|from Bellarmine University's Pathophysiology of Complex Patient Problems project.]] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Definition/Description: == | == Definition/Description: == | ||
| Line 73: | Line 73: | ||
Glaucoma: | Glaucoma: | ||
The discovery of the effects of cannabis reducing intraocular pressure in glaucoma patients prompted the federal government to establish an investigational drug program known as the ''Compassionate Investigational New Drug Program'' (IND). This program assessed the benefits and risks of cannabis use through the ''Missoula Chronic Clinical Cannabis use study.'' The origins of this program and study derive from a patient, Robert Randall, who found regular cannabis use reduced the halo’s associated with glaucoma and enabled him to see better by reducing his intraocular pressure. Robert Randall had been caught cultivating cannabis. Subsequently, Randall went through a lengthy court proceeding that was based on the fact that no conventional pharmaceutical drug could manage his glaucoma symptoms like cannabis could. Cannabis kept Randall from going blind. Randall’s case was dismissed and the federal government began the IND with seven other patients. The report found cannabis has “clinical effectiveness in treating glaucoma, chronic musculoskeletal pain, spasm and nausea, and spasticity due to multiple sclerosis.” Therefore, the clinical studies conducted by the federal government state that cannabis is an effective medicine for several conditions. <ref>Russo, Ethan, Mary Lynn Mathre, Al Byrne, Robert Velin, Paul J. Back, Juan Sanchez Ramos, and Kristin A. Kirlin. "Chronic Cannabis Use in the Compassionate Investigational New Drug Program." Taylor &amp;amp;amp;amp;amp; Francis. Web. 18 Apr. 2016</ref> | The discovery of the effects of cannabis reducing intraocular pressure in glaucoma patients prompted the federal government to establish an investigational drug program known as the ''Compassionate Investigational New Drug Program'' (IND). This program assessed the benefits and risks of cannabis use through the ''Missoula Chronic Clinical Cannabis use study.'' The origins of this program and study derive from a patient, Robert Randall, who found regular cannabis use reduced the halo’s associated with glaucoma and enabled him to see better by reducing his intraocular pressure. Robert Randall had been caught cultivating cannabis. Subsequently, Randall went through a lengthy court proceeding that was based on the fact that no conventional pharmaceutical drug could manage his glaucoma symptoms like cannabis could. Cannabis kept Randall from going blind. Randall’s case was dismissed and the federal government began the IND with seven other patients. The report found cannabis has “clinical effectiveness in treating glaucoma, chronic musculoskeletal pain, spasm and nausea, and spasticity due to multiple sclerosis.” Therefore, the clinical studies conducted by the federal government state that cannabis is an effective medicine for several conditions. <ref>Russo, Ethan, Mary Lynn Mathre, Al Byrne, Robert Velin, Paul J. Back, Juan Sanchez Ramos, and Kristin A. Kirlin. "Chronic Cannabis Use in the Compassionate Investigational New Drug Program." Taylor &amp;amp;amp;amp;amp;amp; Francis. Web. 18 Apr. 2016</ref> | ||
Post Traumatic Stress Disorder: | Post Traumatic Stress Disorder: | ||
| Line 87: | Line 87: | ||
Chronic Pain: ''JAMA's'' 2015 study found patients using cannabis had a reduction in pain symptoms. One of the studies found at least a 30% reduction in pain symptoms compared to those using placebo for those suffering from chronic pain disorders. The trial with the greatest reduction in pain symptoms found smoked THC reported the greatest beneficial effect. Again, this study should be re-visited due to the questionable quality of the smoked cannabis used. Seven of the trials for the indication of chronic pain assessed nabiximols, an oral mucosal spray consisting of 27mg THC and 25mg CBD. Pain conditions studied in this assessment were neuropathic pain and cancer pain. The systematic review and meta analysis indicates the federal government’s schedule I status of cannabis needs to be changed based on scientific evidence.<ref name="pain and spasticity" /> | Chronic Pain: ''JAMA's'' 2015 study found patients using cannabis had a reduction in pain symptoms. One of the studies found at least a 30% reduction in pain symptoms compared to those using placebo for those suffering from chronic pain disorders. The trial with the greatest reduction in pain symptoms found smoked THC reported the greatest beneficial effect. Again, this study should be re-visited due to the questionable quality of the smoked cannabis used. Seven of the trials for the indication of chronic pain assessed nabiximols, an oral mucosal spray consisting of 27mg THC and 25mg CBD. Pain conditions studied in this assessment were neuropathic pain and cancer pain. The systematic review and meta analysis indicates the federal government’s schedule I status of cannabis needs to be changed based on scientific evidence.<ref name="pain and spasticity" /> | ||
Epilepsy: <br>A report of a parent survey of cannabidiol-enriched cannabis use in pediatric treatment-resistant epilepsy found a drastic improvement in seizure symptoms with little side effects in children who did not respond to on average, 12 anti-epileptic medications prior to cannabidiol-enriched cannabis treatment. The report even notes children that were able to reduce seizures entirely as well as additional positive behavioral findings. The report states "sixteen (84%) of the 19 parents reported a reduction in their child's seizure frequency while taking cannabidiol-enriched cannabis. Of these, two (11%) reported complete seizure freedom, eight (42%) reported a greater than 80% reduction in seizure frequency, and six (32%) reported a 25-60% seizure reduction. Other beneficial effects included increased alertness, better mood, and improved sleep. Side effects included drowsiness and fatigue." <ref>Porter BE, Jacobson C. Report of a parent survey of cannabidiol-enriched cannabis use in pediatric treatment-resistant epilepsy [Internet]. Epilepsy &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp; behavior : E&amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;B. U.S. National Library of Medicine; [cited 2016Apr10]. Retrieved from: http://www.ncbi.nlm.nih.gov/pmc/articles/pmc4157067/</ref> | Epilepsy: <br>A report of a parent survey of cannabidiol-enriched cannabis use in pediatric treatment-resistant epilepsy found a drastic improvement in seizure symptoms with little side effects in children who did not respond to on average, 12 anti-epileptic medications prior to cannabidiol-enriched cannabis treatment. The report even notes children that were able to reduce seizures entirely as well as additional positive behavioral findings. The report states "sixteen (84%) of the 19 parents reported a reduction in their child's seizure frequency while taking cannabidiol-enriched cannabis. Of these, two (11%) reported complete seizure freedom, eight (42%) reported a greater than 80% reduction in seizure frequency, and six (32%) reported a 25-60% seizure reduction. Other beneficial effects included increased alertness, better mood, and improved sleep. Side effects included drowsiness and fatigue." <ref>Porter BE, Jacobson C. Report of a parent survey of cannabidiol-enriched cannabis use in pediatric treatment-resistant epilepsy [Internet]. Epilepsy &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp; behavior : E&amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;B. U.S. National Library of Medicine; [cited 2016Apr10]. Retrieved from: http://www.ncbi.nlm.nih.gov/pmc/articles/pmc4157067/</ref> | ||
Fibromyalgia :<br>One study compared 28 fibromyalgia patients who were users compared to 28 who were not. The route of administration was roughly equal. "54% were self-administering cannabis via smoking, 46% via oral ingestion, and 43% combined both smoking and oral administration." Interestingly, the percentages of various cannabinoids in the products the patients were using were not reported. "Information was recorded via the standard Visual Analogue Scale (VAS), the Fibromyalgia Impact Questionnaire (FIQ), Pittsburg Sleep Quality Index (PSQI), and Short Form 36 Health Survey (SF-36)." The study found the VAS showed a "statistically significant reduction in pain and stiffness and enhanced relaxation as well as increased somnolence or a feeling of well-being". Mental health scores on the SF-36 were "significantly higher in users than non-users." The article states "no other differences of statistical significance were recorded in other items of the SF-36, FIQ, or the PSQI." <ref>Fiz, Jimena, Marta Durán, Dolors Capellà, Jordi Carbonell, and Magí Farré. "Cannabis Use in Patients with Fibromyalgia: Effect on Symptoms Relief and Health-Related Quality of Life." PLoS ONE. Public Library of Science. Web. 06 Apr. 201</ref> <br> | Fibromyalgia :<br>One study compared 28 fibromyalgia patients who were users compared to 28 who were not. The route of administration was roughly equal. "54% were self-administering cannabis via smoking, 46% via oral ingestion, and 43% combined both smoking and oral administration." Interestingly, the percentages of various cannabinoids in the products the patients were using were not reported. "Information was recorded via the standard Visual Analogue Scale (VAS), the Fibromyalgia Impact Questionnaire (FIQ), Pittsburg Sleep Quality Index (PSQI), and Short Form 36 Health Survey (SF-36)." The study found the VAS showed a "statistically significant reduction in pain and stiffness and enhanced relaxation as well as increased somnolence or a feeling of well-being". Mental health scores on the SF-36 were "significantly higher in users than non-users." The article states "no other differences of statistical significance were recorded in other items of the SF-36, FIQ, or the PSQI." <ref>Fiz, Jimena, Marta Durán, Dolors Capellà, Jordi Carbonell, and Magí Farré. "Cannabis Use in Patients with Fibromyalgia: Effect on Symptoms Relief and Health-Related Quality of Life." PLoS ONE. Public Library of Science. Web. 06 Apr. 201</ref> <br> | ||
Revision as of 17:20, 19 April 2016
Original Editors -Mark Wojda from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Ryan Scinta, Lucinda hampton, Elaine Lonnemann, Kim Jackson, Ryan Barry, WikiSysop, Joseph Ayotunde Aderonmu and Mark Wojda
Definition/Description:[edit | edit source]
As a result of cannabis decriminalization and legalization throughout the world, healthcare professionals are faced with more questions from patients regarding cannabis and its use. Healthcare professionals have a responsibility to provide evidence-based guidance on this important medical and social issue. Cannabis has significant health benefits and therapeutic applications to a vast array of medical conditions explored in this page. As with any medical substance, cannabis use also presents with associated risks. This page describes the many uses of cannabis in relation to specific patient populations. This page also compares the risks of cannabis from a medical standpoint with other commonly used drugs. The purpose of this page is to provide a comprehensive, up-to-date educational resource for healthcare professionals, patients, and caregivers guided by current evidence-based research. Additionally, the information presented will attempt to dispel many myths and help clear the smoke around issues surrounding the cannabis plant. This page will be updated continually in the future. This page is dedicated to past and future patients.
Etiology/Origin
[edit | edit source]
The plant was first named “cannabis” by a German physician by the name of Leonhart Fuchs in 1542 A.D. Prior to 1542 A.D, throughout the world, it was known as an important medication. [1]
One of the first medical reports in western medicine regarding cannabis was William B ‘O Shaughnessy’s, “On the Preparations of the Indian Hemp, or Gunjah.” Published in 1848, this report analyzed several medical indications and the effect an indian hemp preparation had on them. In rheumatism, O’ Shaughnessy found “alleviation of pain in most, remarkable increase of appetite in all, unequivocal aphrodisia, and great mental cheerfulness.” His report observed the effect of cannabis preparations on hydrophobia, cholera, tetanus, infantile convulsions, and delirium tremens. In the conclusion O’ Shaughnessy reports, “in hemp the profession has gained an anti-convulsive remedy of the greatest value.” [2]
Following O’Shaughnessy’s report, in 1850 cannabis was added to the official handbook of medications, The United States Pharmacopeia. Within the handbook it was regarded as an official medication for a wide-range of ailments. [1]
Today, cannabis has been difficult to study as a complete plant substance from a pharmaceutical standpoint. The Journal of the American Medical Association (JAMA) reports “cannabis is a complex of more than 400 compounds including flavonoids and terpenoids and approximately 70 cannabinoids other than delta 9 tetrahydrocannabinol (THC). These cannabinoids have individual, interactive, and even entourage effects (effects of a compound that are only appreciable in the presence of other compounds) that are not fully understood and that contribute to the net effect of marijuana.” Additionally, “patients will need to experiment with different strains and doses to achieve the desired effects, without much input or oversight from physicians.”Additionally, JAMA reports, “The federal government and states should support medical marijuana research” [3]
Currently, evidence suggests cannabis may be “an effective treatment for chronic pain, neuropathic pain, muscle spasm due to multiple sclerosis or paraplegia. In most states with medical marijuana laws, marijuana can be used to treat severe or chronic pain and severe or persistent muscle spasms.” Cannabis use can be "certified by a physician but it cannot be prescribed by a physician due to its schedule I status." [4]
Anatomy
[edit | edit source]
Humans and drugs have a long, complex relationship. Drugs are predominantly developed from plants because humans have receptors throughout their bodies for the compounds produced from plants. “The synthesis of THC by Raphael Mechoulam led researchers to discover a signaling system. The signaling system of the endocannabinoid system started evolving more than 500 million years ago. The endocannabinoid system and their receptors are found in fish, reptiles, earthworms, leeches, amphibians, birds, and mammals. The evolution of the cannabinoid signaling system indicates it plays a functional role in physiology.” [5]
Cannabinoid receptors belong to a superfamily of G-protein receptors. G-protein receptors are involved in many disease processes.
Cannabinoid G-Protein coupled receptors were initially discovered by Professor Allyn Howett and William Devane. These researchers “mapped the brain's cannabinoid receptor and discovered the main mental and physiological centers cannabis works upon. “
[6]
“Within the brain cannabinoid receptors can be found in the hippocampus (memory), cerebral cortex (higher cognition), cerebellum (motor coordination), basal ganglia (movement), hypothalamus (appetite), amygdyla (emotion), and elsewhere. There are few cannabinoid receptors in the brainstem (respiration and heart beat) which explains why you cannot fatally overdose on cannabis.” [5]
Lisa Matsuda is responsible for discovering the DNA sequence that “encodes the THC receptor in the rat’s brain.” Matsuda also cloned the cannabis receptor.
The cloning of the cannabis receptor enabled researchers to discover cannabinoid agonists and cannabinoid antagonists. Researchers were also able to discover cannabinoid receptors. “The CB1 receptor is a central nervous system receptor and is responsible for the high. THC binds to the CB1 receptor creating the high.”[7]
CB2 receptors are found throughout the peripheral nervous system and the immune system. “CB2 receptors are present in the gut, liver, spleen, heart, kidneys, bones, blood vessels, lymph cells, endocrine glands, and reproductive organs.” THC stimulates the CB2 receptors but this does not result in a "high" because they are not found in the brain. “Therefore, the CB1 receptors mediates the high and the CB2 receptor controls the immune response.”[8]
Endocannabinoids: “The discovery of cannabinoid receptors lead to Mechoulam’s discovery of the naturally occurring endogenous (made internally) cannabinoid. The endocannabinoids are responsible for an array of medical implications. The endocannabinoids attach to the same receptors that THC attaches to. Currently, there are two endocannabinoids. Anandamide and 2-AG (2-arichidonoylglycerol) which bind to both CB1 and CB2 receptors."[5]
According to an editorial in the 2015 June issue of the Journal of the American Medical Association (JAMA), it states, “The endocannabinoid system is involved in axon elongation, neurogenesis, neural maturation and specification, glia formation, neuronal migration, and synaptic pruning. Furthermore, the endocannabinoid system evolves during adolescence.”[3]
Classification
[edit | edit source]
The Federal classification of cannabis as a medicine:
The US Department of Health and Human Services: Patent # 6630507: Titled "Cannabinoids as Antioxidants and NeuroProtectants"
The US Department of Health and Human Services states: "Cannabinoids have been found to have antioxidant properties and are found to have particular application as neuroprotectants, for example in limiting neurological damage following ischemic insults, such as stroke and trauma, or in the treatment of neurodegenerative diseases, such as Alzheimer's Disease, Parkinson's Disease and HIV dementia."Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Cannabis as a plant:
Cannabis is classified as a member of the cannabaceae plant family. Cannabis is classified under the single species of hemp (C. sativa). The female version of hemp is considered “marijuana” and consists of the indica, sativa, and ruderalis varieties. Cannabis has thousands of varieties and the effects of each variety are different. Hops belongs to the cannabaceae plant family as well. Hops is used in the production of beer, a celebrated legal drug.
[9][10]
Federal Classification
[edit | edit source]
The Federal classification of cannabis legally: Schedule 1 narcotic, no accepted medical value.
As defined by the United States Controlled Substance Act (CSA).
“Schedule I drugs are defined as:
(A) The drug or other substance has a high potential for abuse.
(B) The drug or other substance has no currently accepted medical use in treatment in the United States.
(C) There is a lack of accepted safety for use of the drug or other substance under medical supervision.”
[11]
Indications[edit | edit source]
This section of the page will be continuously updated.
Cancer:
Manuel Guzman and his team of researchers discovered cannabis inhibits cancer tumor growth. The study found cannabinoids “inihibit gliomas in animals by modulating key cell signaling pathways, mostly the endoplasmic reticulum stress response, thereby inducing antitumoral actions such as the apoptotic death of tumor cells and the inhibition of tumor angiogenesis.”[12]
The National Cancer Institute states: “Cannabis and cannabinoids have been studied in the laboratory and the clinic for relief of pain, nausea and vomiting, anxiety, and loss of appetite.”[13]
Additionally, the institute explains, “Cannabis has been shown to kill cancer cells in the laboratory.” However, cannabis is not approved by the FDA in the treatment of cancer either as an adjunct or as an alternative treatment method. [13]
Glaucoma:
The discovery of the effects of cannabis reducing intraocular pressure in glaucoma patients prompted the federal government to establish an investigational drug program known as the Compassionate Investigational New Drug Program (IND). This program assessed the benefits and risks of cannabis use through the Missoula Chronic Clinical Cannabis use study. The origins of this program and study derive from a patient, Robert Randall, who found regular cannabis use reduced the halo’s associated with glaucoma and enabled him to see better by reducing his intraocular pressure. Robert Randall had been caught cultivating cannabis. Subsequently, Randall went through a lengthy court proceeding that was based on the fact that no conventional pharmaceutical drug could manage his glaucoma symptoms like cannabis could. Cannabis kept Randall from going blind. Randall’s case was dismissed and the federal government began the IND with seven other patients. The report found cannabis has “clinical effectiveness in treating glaucoma, chronic musculoskeletal pain, spasm and nausea, and spasticity due to multiple sclerosis.” Therefore, the clinical studies conducted by the federal government state that cannabis is an effective medicine for several conditions. [14]
Post Traumatic Stress Disorder:
A study from the Hadassah University Hospital outpatient clinic in Jerusalem, Israel yielded promising results for those suffering from unremitting chronic PTSD. The open-label study conducted over the span of three weeks on ten patients explored "tolerance, safety, and preliminary effects of delta-9-THC as an add-on treatment for patients with chronic PTSD." To evaluate the effects of the medication intervention, the study used the “Clinician-Administered PTSD scale (CAPS), the Clinical Global Impression Scale (CGI), the Pittsburg Sleep Quality Index (PSQI), the self- reported Nightmare Frequency Questionnaire (NFQ), and the clinician- administered Nightmare Effects Survey (NES). The study used a 5 milligram (mg) oral dose of THC administered twice daily. Only three of the patients reported adverse reactions to the drug.” Interestingly, those were not severe enough to discontinue treatment. The study “yielded statistically significant improvements in global symptom severity, sleep quality, the frequency of nightmares, and PTSD hyperarousal symptoms." The study verifies the therapeutic application of cannabinoids in treating PTSD symptoms. [15]
A 2014 study from the Journal of Psychoactive Drugs found “A 75% reduction of Clinician Administered Post-Traumatic Stress Scale (CAPS) symptoms in patients using cannabis.” This study confirms that cannabis reduces symptoms of PTSD in individuals using cannabis as compared with those who do not. [16]
In the July 2015 issue of The American Legion, a magazine dedicated to those serving the United States, veterans make it clear they want access to medical marijuana specifically for “pain and PTSD”. The article notes "Veterans Affairs (VA) prohibits its physicians from discussing cannabis use, even in states where medical marijuana is legal." Scott Murphy, the founder of, Veterans for Safe Access and Compassionate Care, contends "medical marijuana can help reduce their (veterans) opiate dependence and leads to fewer suicides." The article states former veterans are saying "narcotic painkillers, sleeping pills, amphetamines, antidepressants and drugs they are being prescribed are dangerous, if not lethal." With the mounting evidence illustrating the benefits of cannabis to those serving our country the article pinpoints "VA acknowledges that veterans who use medical marijuana may lose access to some medical care." The article shows how medical marijuana can play an important role in recovery for veterans returning home from war. [17]
Multiple Sclerosis:
A 2015 study from the Journal of The American Medical Association (JAMA), “Cannabinoids for Medical Use A Systematic Review and Meta-Analysis”, found "moderate quality evidence to support the use of cannabinoids for the treatment of chronic pain and spasticity." The report highlights two studies that found a "50% reduction in spasticity symptoms." Additionally, two other studies found a “30% reduction in spasticity symptoms.” The report looked at studies which included the following: an oral mucosal spray of CBD/THC (nabiximols), orally ingested synthetic THC (Dronabinol), a synthetic cannabinoid derivative mimicking THC (nabilone), oral capsules of combined THC/CBD, smoked THC of low potency and questionable quality ranging from 2.5%-9.4%, and an oral tablet of pure >98% natural delta-9-THC. The systematic review and meta-analysis, although indicating "moderate quality evidence", should be re-evaluated due to inherent flaws in the report. Many of the beneficial compounds found in the natural cannabis plant went ignored. The low concentrations of the smoked THC indicates a much-needed re-evaluation of the samples used. The review should include the entire cannabinoid profile of the sample. Furthermore, these studies indicate the federal government’s scheduling of cannabis as a schedule I drug needs to be changed based on scientific evidence. [18]
Chronic Pain: JAMA's 2015 study found patients using cannabis had a reduction in pain symptoms. One of the studies found at least a 30% reduction in pain symptoms compared to those using placebo for those suffering from chronic pain disorders. The trial with the greatest reduction in pain symptoms found smoked THC reported the greatest beneficial effect. Again, this study should be re-visited due to the questionable quality of the smoked cannabis used. Seven of the trials for the indication of chronic pain assessed nabiximols, an oral mucosal spray consisting of 27mg THC and 25mg CBD. Pain conditions studied in this assessment were neuropathic pain and cancer pain. The systematic review and meta analysis indicates the federal government’s schedule I status of cannabis needs to be changed based on scientific evidence.[18]
Epilepsy:
A report of a parent survey of cannabidiol-enriched cannabis use in pediatric treatment-resistant epilepsy found a drastic improvement in seizure symptoms with little side effects in children who did not respond to on average, 12 anti-epileptic medications prior to cannabidiol-enriched cannabis treatment. The report even notes children that were able to reduce seizures entirely as well as additional positive behavioral findings. The report states "sixteen (84%) of the 19 parents reported a reduction in their child's seizure frequency while taking cannabidiol-enriched cannabis. Of these, two (11%) reported complete seizure freedom, eight (42%) reported a greater than 80% reduction in seizure frequency, and six (32%) reported a 25-60% seizure reduction. Other beneficial effects included increased alertness, better mood, and improved sleep. Side effects included drowsiness and fatigue." [19]
Fibromyalgia :
One study compared 28 fibromyalgia patients who were users compared to 28 who were not. The route of administration was roughly equal. "54% were self-administering cannabis via smoking, 46% via oral ingestion, and 43% combined both smoking and oral administration." Interestingly, the percentages of various cannabinoids in the products the patients were using were not reported. "Information was recorded via the standard Visual Analogue Scale (VAS), the Fibromyalgia Impact Questionnaire (FIQ), Pittsburg Sleep Quality Index (PSQI), and Short Form 36 Health Survey (SF-36)." The study found the VAS showed a "statistically significant reduction in pain and stiffness and enhanced relaxation as well as increased somnolence or a feeling of well-being". Mental health scores on the SF-36 were "significantly higher in users than non-users." The article states "no other differences of statistical significance were recorded in other items of the SF-36, FIQ, or the PSQI." [20]
Alzheimer’s, Huntington’s, and Parkinson’s Disease:
A report from the Lancent Journal of Neurology reports cannabis has significant therapeutic potential in the treatment of Alzheimer's, Huntington's, and Parkinson's Disease. [21]
Safety[edit | edit source]
No reported overdoses:
Today, no deaths have ever been recorded due to a “cannabis overdose”. Therefore, it is reasonable to assume, from a health perspective, that cannabis is safer than many legal and illegal drugs.[22] "Every 19 minutes someone overdoses from a prescription drug overdose."[23]Therefore, it's safe to assume, that cannabis is safer compared to prescription drugs.
Cannabis and the Lungs:
A report from The National Institute of Drug Abuse (NIDA) attempted to find a link between cannabis and impaired pulmonary function. Contrary to common public misconception, the report found no link between cannabis and lung disease. In fact, the report found cannabis plays a protective role in lung function. [24]
Cannabis and the Brain:
Robert Heath's 1976 study was sensationalized and has since been debunked. Robert Heath's unethical experiment poisoned Rhesus Monkeys with smoke by cutting off their oxygen supply while administering cannabis filled cigarettes. This study is the source of the claim that cannabis causes brain damage. [25]
Cannabis Compared to Alcohol:
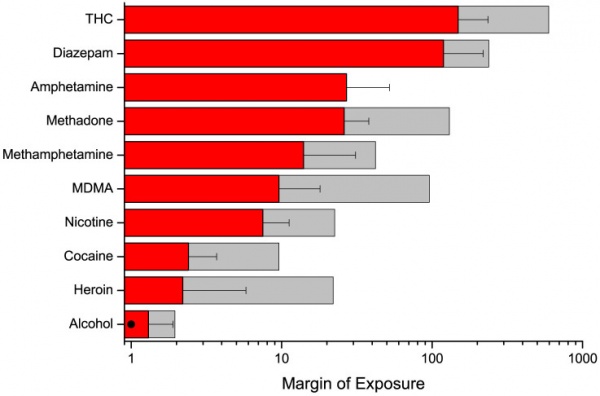
A “Comparative risk assessment of alcohol, tobacco, cannabis and other illicit drugs using the margin of exposure approach” states
“Specifically, the results confirm that the risk of cannabis may have been overestimated in the past. At least for the endpoint of mortality, the MOE for THC/cannabis in both individual and population-based assessments would be above safety thresholds (e.g. 100 for data based on animal experiments). In contrast, the risk of alcohol may have been commonly underestimated.”
Therefore, it can be assumed from a health standpoint, that cannabis is significantly safer than alcohol. [26]
Risks[edit | edit source]
Risks:
It has been recommended that the age at which medical marijuana exposure can occur needs further research. A JAMA editorial states “brain development occurs until age 25, the endocannabinoid system is involved in brain development, cannabinoid exposure during critical periods of development is associated with long-lasting changes in behavior and cognition." [3]However, the report does not explcitly state how the long-lasting changes in behavior and cognition could result specifically in adolescent impairments. Furthermore, alcohol is readily available to those 21 years of age and the same discussion is not happening.
Physical risks of regular cannabis use in patients include “symptoms of chronic bronchitis and increased rate of respiratory tract infections and pneumonia.” However, cannabis does not need to be smoked therefore these risks can be easily avoided. [27]
The physical effects of regular cannabis use are mild compared to legal substances like alcohol. Cannabis is 9% addictive in adult users which is less than alcohol, prescription narcotics, and cigarettes.[28]
The 2015 JAMA report notes withdrawal symptoms are characterized by “anxiety, irritability, craving, dysphoria, and insomnia.”[27] These withdrawal symptoms are mild compared to alcohol. Alcohol withdrawal can cause seizures[29] and is widely available for individuals over 21 years or older even though brain development continues until 25 years of age.[30]
Synthetic Cannabinoids are not a safe alternative: Medical cannabis prohibition has created a market many are exploiting, the consequences of which are worse than cannabis itself. Synthetic cannabinoids are no exception. A 2015 JAMA report stated synthetic cannabinoids can cause adverse health effects that "include but are not limited to excited delirium, acute kidney injury, seizures, psychosis, hallucinations, cardiotoxic effects, coma, and death-with some users dying before they could reach the emergency department." Natural cannabis does not cause these adverse effects and cannot cause death strictly from use. In the report, users stated they tried the synthetic cannabinoids "out of curiosity for experimentation (91%), a desire to get high (89%), to relax (71%), and to get high without risking a positive drug test (71%)." More importantly to note is the sale and manufacturing of these substances flourishes due to lack of regulation. Currently, many shops will market these products as a "safe" form of getting high or as an alternative to cannabis. Marketing aims towards younger individuals who can legally buy these products in "smoke shops" if they are 18 years old which is before the human brain is fully developed. These unsafe and toxic products illustrate a common side effect of prohibition which is people using more harmful products than cannabis under the assumption that they are much safer. [31]
Edibles and Proper Dosing: The edibles industry has been under a lot of pressure since recreational marijuana has been implemented. The edibles industry needs to step up its ability to properly dose products for the sake of medical patients seeking relief.
A recent research letter in JAMA’s 2015 issue analyzed edibles from Los Angeles, San Francisco, and Seattle Washingt[3]on, some of the largest medical cannabis markets in the country. Although the results of the study were limited and are not generalizable they illustrate the need for greater quality control in the medical cannabis industry with respect to accurate dosing specifically with respect to edibles. Over 50% of the edibles in the study were not within the 10% margin of detectable THC and CBD concentrations. 60% of the edibles examined were under-dosed. Many people respond to edibles poorly because they lack education regarding the pharmacological action of them. Edibles take longer to work and are metabolized stronger through the liver. [32]People lacking education in edibles take too many too quickly not understanding they take time to be absorbed. People need to be more educated regarding edible cannabis products and the industry needs to work on more accurate dosing for the sake of medical patients fighting chronic conditions. [33]
Contraindications: According to JAMA “Explicit contraindications such as schizophrenia, bipolar disorder, or substance dependence need to be identified along with measures to minimize the likelihood that persons with contraindications would be able to obtain medical marijuana.”[3] However, these contraindications are not conclusive.
Drug Interactions[edit | edit source]
A study in JAMA found a “25% reduction in opioid related deaths in states with medical marijuana programs.”[34] The study states, “Medical marijuana laws, when implemented, may represent a promising approach for stemming runaway rates of nonintentional opioid analgesic effects.” As the epidemic negatively impacts the country, politicians like Elizabeth Warren call for more studies to be done on cannabis to curb the destructive effects of the opioid epidemic.[35]
Additionally, “there is some evidence of cross-tolerance between cannabinoids and opioids.”[3]
Relevance to Physical Therapy[edit | edit source]
Few studies have been done in relation to cannabinoids as an adjunct to physical therapy treatment. However, two future areas of research could focus on professional athletic populations and patients with neurological or movement related disorders.
Many athletes of various backgrounds and professions support the use of cannabis.
It has been reported that over half of the NFL uses cannabis throughout the course of the season.[36]
Former NFL running back Ricky Williams says, “The teams don’t care, you know, they weren’t trying to take care of me. So, I had to take care of myself. One of the ways I took care of myself was using cannabis.” [37]
Former quarterback for the Chicago Bears Jim McMahon reports, "With my chronic pain, all my surgeries I've had. The arthritis. It's getting me through the day. It's helped so many people: epileptics, cancer patients... it helps me every day. I feel a heck of a lot better than when I had to take all those pain pills."[38]
In action sports athletic populations cannabis is widely used and accepted. Canadian snowboarder Ross Rebagliati had to fight to keep his gold medal from the 1998 Olympic Games after testing positive for 17 nanograms of THC in a millimeter of his urine. Rebagliati states
“It's not like alcohol, where you feel invincible. You can analyze the risk at a higher level and you can make a better decision with your heightened awareness. For an experienced user — and I emphasize experienced user — if you are charging hard, it can give you a brain check, make you more aware of the risks and the opportunities."
Seven times X Games Gold Medalist, Tanner Hall, one of the most influential skiers in the world, endorses the use of cannabis. Tanner Hall has suffered severe injuries throughout his career and credits cannabis to help aid his recovery. Hall says, “Drugs are stupid, dude. I know that. Let's keep it natural." Hall continues, "Under the FIS rules, you can drink as much alcohol as you can, take crazy pills with a prescription. But if you happen to set that little tree on fire and smell it, you're out. Think about that. Big up to Washington and Colorado for leading the charge."[39]
Based off these subjective reports, physical therapists could evaluate the effects of cannabis and develop ways to objectively report differences in performance in athletic populations.
It is well documented that exercise is neuroprotective. Many people are limited in their ability to exercise as a result of pain, spasticity, or neurological problems such as unremitting seizures. Cannabis’ ability to reduce pain, reduce spasticity, and reduce seizures could alter the course of a patient’s physical therapy care. More research needs to be conducted regarding physical therapy and cannabis therapeutics. Based off of clinical research done on cannabis and its effects on parkinson’s disease, epilepsy, spasticity and pain associated with multiple sclerosis and paraplegia, it is reasonable to propose research interventions combining both exercise and cannabis. Additionally, the role of a physical therapist is to advocate for patients. If a physical therapist notes improvement in a chronic condition due to the use of cannabis, then he or she should advocate for access to the substance.
Case Reports/ Case Studies:
[edit | edit source]
This page will be continually updated in the future.
HIV:
Woolridge E, Barton S, Samuel J, Osorio J, Dougherty A, Holdcroft A. Cannabis use in HIV for pain and other medical symptoms. J Pain Symptom Manage 2005;29(4):358-67.
http://www.ncbi.nlm.nih.gov/pubmed/15857739
Multiple Sclerosis:
Consroe P, Musty R, Rein J, Tillery W, Pertwee R. The perceived effects of smoked cannabis on patients with multiple sclerosis. European Neurology 1997;38:44-48.
http://www.ncbi.nlm.nih.gov/pubmed/9252798
Chong MS, Wolff K, Wise K, Tanton C, Winstock A, Silber E. Cannabis use in patients with multiple sclerosis. Mult Scler 2006;12(5):646-51.
http://www.ncbi.nlm.nih.gov/pubmed/17086912
Spinal Cord Injury:
Malec J, Harvey RF, Cayner JJ. Cannabis effect on spasticity in spinal cord injury. Archives of Physical Medicine and Rehabilitation 1982;63:116-118.
http://www.ncbi.nlm.nih.gov/pubmed/6978699
Crohn's Disease:
Lal S, Prasad N, Ryan M, Tangri S, Silverberg MS, Gordon A, Steinhart H. Cannabis use amongst patients with inflammatory bowel disease. Eur J Gastroenterol Hepatol 2011;23(10):891-6.
http://www.ncbi.nlm.nih.gov/pubmed/21795981
Resources
[edit | edit source]
For information regarding your states cannabis laws:
http://norml.org/
For information regarding which strains you or your patient's are using:
For information regarding cannabis therapeutics for different conditions including veterans:
http://www.safeaccessnow.org/
Realm of Caring: Pediatric Epilepsy
Information on legal issues: Marijuana policy project:
Drug policy information:
Recent Related Research (from Pubmed)[edit | edit source]
see tutorial on Adding PubMed Feed
Failed to load RSS feed from http://www.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=169y_86ceC_-bu0xhVp8W0LNFt6JjWkKQVWt20NBFGwPUebovR|charset=UTF-8|short|max=10: Error parsing XML for RSS
References[edit | edit source]
see adding references tutorial.
- ↑ 1.0 1.1 Jacobson R. Medical Marijuana: How the Evidence Stacks Up [Internet]. Scientific American. [cited 2016Apr17]. Retrieved from: http://www.scientificamerican.com/article/medical-marijuana-how-the-evidence-stacks-up/
- ↑ O'Shaughnessy WB. On the Preparations of the Indian Hemp, or Gunjah: Cannabis Indica Their Effects on the Animal System in Health, and their Utility in the Treatment of Tetanus and other Convulsive Diseases [Internet]. Provincial Medical Journal and Retrospect of the Medical Sciences. U.S. National Library of Medicine; [cited 2016Apr14]. Retrieved from: http://www.ncbi.nlm.nih.gov/pmc/articles/pmc2490264/
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 D'Souza DC, Ranganathan M. Medical Marijuana Is the Cart Before the Horse. The Journal of The American Medical Association. 2015Jun23;313(24):2431–2.
- ↑ Thompson AE. Medical Marijuana. The Journal of The American Medical Association. 2015Jun23;313(24):2508.
- ↑ 5.0 5.1 5.2 Lee M. [Internet]. Projectcbd.org. 2016 [cited 14 April 2016]. Available from:https://www.projectcbd.org/article/brain-and-marijuana-book-excerpt
- ↑ Marijuana Research: Discovery of the Cannabinoid Receptor System [Internet]. Drug Science . [cited 2016Apr14]. Retrieved from: http://www.drugscience.org/petition/c3d.html
- ↑ Matsuda LA, Lolait SJ, Brownstein MJ, Young AC, Bonner TI. Structure of a cannabinoid receptor and functional expression of the cloned cDNA. Nature. 1990;346:561–4. [PubMed] [Ref list] )
- ↑ Munro S, Thomas KL, Abu-Shaar M. Molecular characterization of a peripheral receptor for cannabinoids. Nature. 1993)
- ↑ Classification | USDA PLANTS [Internet]. Classification | USDA PLANTS. [cited 2016Apr13]. Retrieved from: http://plants.usda.gov/java/classificationservlet?source=display
- ↑ The Editors of Encyclopædia Britannica. cannabis [Internet]. Encyclopedia Britannica Online. Encyclopedia Britannica; [cited 2016Apr13]. Retrieved from: http://www.britannica.com/plant/cannabis-plant
- ↑ Controlled Substance Schedules [Internet]. Resources -. [cited 2016Apr10]. Retrieved from: http://www.deadiversion.usdoj.gov/schedules/
- ↑ Guzman M, Blazquez C, Casanova LL, Planas A, Pulgar TGD, Villanueva C, et al. Inhibition of tumor angiogenesis by cannabinoids - FASEB J [Internet]. [cited 2016Apr13]. Retrieved from: http://www.fasebj.org/content/17/3/529.full
- ↑ 13.0 13.1 Cannabis and Cannabinoids [Internet]. National Cancer Institute. [cited 2016Apr16]. Retrieved from: http://www.cancer.gov/about-cancer/treatment/cam/patient/cannabis-pdq
- ↑ Russo, Ethan, Mary Lynn Mathre, Al Byrne, Robert Velin, Paul J. Back, Juan Sanchez Ramos, and Kristin A. Kirlin. "Chronic Cannabis Use in the Compassionate Investigational New Drug Program." Taylor &amp;amp;amp;amp;amp; Francis. Web. 18 Apr. 2016
- ↑ Roitman, Pablo, Raphael Mechoulam, Rena Cooper-Kazaz, and Arieh Shalev. "Preliminary, Open-Label, Pilot Study of Add-On Oral Δ9-Tetrahydrocannabinol in Chronic Post-Traumatic Stress Disorder." Clinical Drug Investigation Clin Drug Investig 34.8 (2014): 587-91.
- ↑ Greer, George R., Charles S. Grob, and Adam L. Halberstadt. "PTSD Symptom Reports of Patients Evaluated for the New Mexico Medical Cannabis Program." Journal of Psychoactive Drugs 46.1 (2014): 73-77. Web. Cannabis and PTSD symptom reduction
- ↑ Olson K. The Cannabis Question. The American Legion. 2015Jul;179(1):24.fckLRVeterans want medical cannabis option.
- ↑ 18.0 18.1 Whiting PF, Wolff RF, Deshpande S, Nisio MD, Duffy S, Hernandez AV, et al. Cannabinoids for Medical Use. Jama. 2015;313(24):2460–8.Use of cannabinoids for chronic pain and spasticity
- ↑ Porter BE, Jacobson C. Report of a parent survey of cannabidiol-enriched cannabis use in pediatric treatment-resistant epilepsy [Internet]. Epilepsy &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp; behavior : E&amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;B. U.S. National Library of Medicine; [cited 2016Apr10]. Retrieved from: http://www.ncbi.nlm.nih.gov/pmc/articles/pmc4157067/
- ↑ Fiz, Jimena, Marta Durán, Dolors Capellà, Jordi Carbonell, and Magí Farré. "Cannabis Use in Patients with Fibromyalgia: Effect on Symptoms Relief and Health-Related Quality of Life." PLoS ONE. Public Library of Science. Web. 06 Apr. 201
- ↑ Baker D, Pryce G, Giovannoni G, Thompson AJ. The therapeutic potential of cannabis. The Lancet Neurology. 2003;2(5):291–8.
- ↑ Internet]. Overdose Death Rates. 2015 [cited 2016Apr11]. Retrieved from: https://www.drugabuse.gov/related-topics/trends-statistics/overdose-death-rates
- ↑ Paulozzi L, Baldwin G, Franklin G, Kerlikowske G, Jones C, Ghiya N, et al. CDC Grand Rounds: Prescription Drug Overdoses—a U.S. Epidemic [Internet]. Jamanetwork.com. JAMA ; 2012 [cited 2016Apr15]. Retrieved from: http://jama.jamanetwork.com/article.aspx?articleid=1356004
- ↑ Tashkin DP, Simmons MS, Sherrill DL, Coulson AH. Heavy habitual marijuana smoking does not cause an accelerated decline in FEV1 with age. Am J Respir Crit Care Med American Journal of Respiratory and Critical Care Medicine. 1997;155(1):141–8.
- ↑ Harper JW, Heath RG, Myers WA. Effects of cannabis sativa on ultrastructure of the synapse in monkey brain. J Neurosci Res Journal of Neuroscience Research. 1977;3(2):87–93.
- ↑ Lachenmeier DW, Rehm J. Comparative risk assessment of alcohol, tobacco, cannabis and other illicit drugs using the margin of exposure approach [Internet]. Scientific Reports. Nature Publishing Group; [cited 2016Apr15]. Retrieved from: http://www.ncbi.nlm.nih.gov/pmc/articles/pmc4311234/http://www.ncbi.nlm.nih.gov/pmc/articles/pmc4311234
- ↑ 27.0 27.1 Hill KP. Medical Marijuana for Treatment of Chronic Pain and Other Medical and Psychiatric Problems. Jama. 2015;313(24):2474–81.
- ↑ Arkowitz H. Experts Tell the Truth about Pot [Internet]. Scientific American. [cited 2016Apr13]. Retrieved from: http://www.scientificamerican.com/article/the-truth-about-pot/
- ↑ Rogawski MA. Update on the Neurobiology of Alcohol Withdrawal Seizures [Internet]. Epilepsy Currents. Blackwell Science Inc; [cited 2016Apr13]. Retrieved from: http://www.ncbi.nlm.nih.gov/pmc/articles/pmc1312739/
- ↑ Aamodt S, Cox T. Brain Maturity Extends Well Beyond Teen Years [Internet]. NPR. NPR; [cited 2016Apr14]. Retrieved from: http://www.npr.org/templates/story/story.php?storyid=141164708
- ↑ Trecki J, Gerona RR, Schwartz MD. Synthetic Cannabinoid-Related Illnesses and Deaths. Journal of The American Medical Association. 2015Jul9;:103–7.fckLRSynthetic cannabinoids JAMA
- ↑ Sharma P, Murthy P, Bharath MMS. Chemistry, Metabolism, and Toxicology of Cannabis: Clinical Implications [Internet]. Iranian Journal of Psychiatry. Tehran University of Medical Sciences; [cited 2016Apr10]. Retrieved from: http://www.ncbi.nlm.nih.gov/pmc/articles/pmc3570572/
- ↑ Vandrey R, Raber JC, Raber ME, Douglass B, Miller C, Bonn-Miller MO. Cannabinoid Dose and Label Accuracy in Edible Medical Cannabis Products. Jama. 2015;313(24):2491.
- ↑ Hayes MJ, Brown MS. Medical Cannabis Laws and Opioid Mortality [Internet]. JAMA Network. [cited 2016Apr13]. Retrieved from: http://archinte.jamanetwork.com/article.aspx?articleid=1898878
- ↑ Holpuch A. Elizabeth Warren asks CDC to consider legal marijuana as alternative painkiller [Internet]. The Guardian. Guardian News and Media; 2016 [cited 2016Apr13]. Retrieved from: http://www.theguardian.com/us-news/2016/feb/12/elizabeth-warren-medical-marijuana-painkiller-opioid-abuse
- ↑ Freeman M. NFL Players View Pot as a Savior [Internet]. Bleacher Report. [cited 2016Apr13]. Retrieved from: http://bleacherreport.com/articles/2486218-banned-but-bountiful-marijuana-coveted-by-nfl-players-as-invaluable-painkiller
- ↑ Samuel E. Ricky Williams recommends NFL players use marijuana for pain [Internet]. NY Daily News. [cited 2016Apr16]. Retrieved from: http://www.nydailynews.com/sports/football/ricky-williams-recommends-nfl-players-marijuana-pain-article-1.2517890
- ↑ O'leary D. Ex-Bears QB McMahon says medical marijuana got him off pills [Internet]. NY Daily News. [cited 2016Apr16]. Retrieved from: http://www.nydailynews.com/sports/football/ex-bears-qb-mcmahon-medical-marijuana-pills-article-1.2513260
- ↑ Blevins J. Acceptance of pot grows like weeds in sports world [Internet]. - The Denver Post. [cited 2016Apr16]. Retrieved from: http://www.denverpost.com/marijuana/ci_24809236/acceptance-pot-grows-like-weeds