Mast Cell Activation Syndrome (MCAS): Difference between revisions
(Completed text editing) |
(Finished editing) |
||
| Line 28: | Line 28: | ||
== Clinically Relevant Anatomy == | == Clinically Relevant Anatomy == | ||
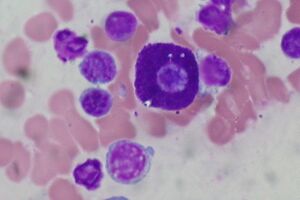
[[File:Mast Cell, Bone Marrow Aspirate, Wright Stain (5916735712).jpg|thumb|Mast Cell Stain]] | |||
Mast cells are granular cells that originate from bone marrow and are distributed throughout the body residing in a wide variety of tissues including but not limited to skin and connective tissues, the GI system, and the respiratory system. They are most commonly located near blood vessels, mucosa, and lymph. <ref>Moon TC, St Laurent CD, Morris KE, Marcet C, Yoshimura T, Sekar Y, Befus AD. Advances in mast cell biology: new understanding of heterogeneity and function. Mucosal Immunol. 2010 Mar;3(2):111-28. doi: 10.1038/mi.2009.136. Epub 2009 Dec 30. PMID: 20043008.</ref> Mediators are found in the membranes surrounding the granules and are released into the environment as a response to allergens. This release results in an inflammatory response that also recruits other immune cells to be released in the region. <ref name=":1">Valent P, Akin C, Arock M, Brockow K, Butterfield JH, Carter MC, et al. Definitions, criteria and global classification of mast cell disorders with special reference to mast cell activation syndromes: a consensus proposal. Int Arch Allergy Immunol. 2012;157(3):215-25.</ref><ref name=":2">Valent P. Mast cell activation syndromes: definition and classification. Allergy. 2013 Apr;68(4):417-24.</ref> | Mast cells are granular cells that originate from bone marrow and are distributed throughout the body residing in a wide variety of tissues including but not limited to skin and connective tissues, the GI system, and the respiratory system. They are most commonly located near blood vessels, mucosa, and lymph. <ref>Moon TC, St Laurent CD, Morris KE, Marcet C, Yoshimura T, Sekar Y, Befus AD. Advances in mast cell biology: new understanding of heterogeneity and function. Mucosal Immunol. 2010 Mar;3(2):111-28. doi: 10.1038/mi.2009.136. Epub 2009 Dec 30. PMID: 20043008.</ref> Mediators are found in the membranes surrounding the granules and are released into the environment as a response to allergens. This release results in an inflammatory response that also recruits other immune cells to be released in the region. <ref name=":1">Valent P, Akin C, Arock M, Brockow K, Butterfield JH, Carter MC, et al. Definitions, criteria and global classification of mast cell disorders with special reference to mast cell activation syndromes: a consensus proposal. Int Arch Allergy Immunol. 2012;157(3):215-25.</ref><ref name=":2">Valent P. Mast cell activation syndromes: definition and classification. Allergy. 2013 Apr;68(4):417-24.</ref> | ||
| Line 61: | Line 61: | ||
==== Common Complaints ==== | ==== Common Complaints ==== | ||
Some of the most common complaints and symptoms include but are not limited to: | Some of the most common complaints and symptoms include but are not limited to:<ref name=":1" /><ref name=":10" /> | ||
* Flushing, itching, and skin rash, skin lesions, and/ or redness | * Flushing, itching, and skin rash, skin lesions, and/ or redness | ||
| Line 77: | Line 77: | ||
* Nasal congestion | * Nasal congestion | ||
* Neurological symptoms | * [[Neurological Disorders|Neurological]] symptoms | ||
* Fatigue and Fibromyalgia like pain | * Fatigue and [[Fibromyalgia]] like pain | ||
* Rashes | * Rashes | ||
* Psychiatric and neurological disorders | * Psychiatric and neurological disorders | ||
* Elhers-Danlos syndrome | * [https://www.physio-pedia.com/Ehlers-Danlos_Syndrome?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal Elhers-Danlos] syndrome | ||
* Postural Orthostatic tachycardia syndrome (POTS) <ref name=":4">Matito A, Escribese MM, Longo N, Mayorga C, Luengo-Sánchez O, Pérez-Gordo M, Matheu V, Labrador-Horrillo M, Pascal M, Seoane-Reula ME; Comité de Inmunología de la Sociedad Española de Alergología e Inmunología Clínica (SEAIC). Clinical Approach to Mast Cell Activation Syndrome: A Practical Overview. J Investig Allergol Clin Immunol. 2021 Dec 21;31(6):461-470. doi: 10.18176/jiaci.0675. Epub 2020 Feb 5. PMID: 33541851.</ref> | * Postural Orthostatic tachycardia syndrome (POTS) <ref name=":4">Matito A, Escribese MM, Longo N, Mayorga C, Luengo-Sánchez O, Pérez-Gordo M, Matheu V, Labrador-Horrillo M, Pascal M, Seoane-Reula ME; Comité de Inmunología de la Sociedad Española de Alergología e Inmunología Clínica (SEAIC). Clinical Approach to Mast Cell Activation Syndrome: A Practical Overview. J Investig Allergol Clin Immunol. 2021 Dec 21;31(6):461-470. doi: 10.18176/jiaci.0675. Epub 2020 Feb 5. PMID: 33541851.</ref> | ||
* Celiac disease and gluten intolerances<ref>Theoharides TC, Valent P, Akin C. Mast cells, mastocytosis, and related disorders. New England Journal of Medicine. 2015 Jul 9;373(2):163-72.</ref> | * [[Celiac Disease (Coeliac Disease)|Celiac]] disease and gluten intolerances<ref name=":10">Theoharides TC, Valent P, Akin C. Mast cells, mastocytosis, and related disorders. New England Journal of Medicine. 2015 Jul 9;373(2):163-72.</ref> | ||
* Autoimmune disorders | * Autoimmune disorders | ||
* Hypotension<ref>Valent P, Akin C, Bonadonna P, Hartmann K, Brockow K, Niedoszytko M, Nedoszytko B, Siebenhaar F, Sperr WR, Oude Elberink JNG, Butterfield JH, Alvarez-Twose I, Sotlar K, Reiter A, Kluin-Nelemans HC, Hermine O, Gotlib J, Broesby-Olsen S, Orfao A, Horny HP, Triggiani M, Arock M, Schwartz LB, Metcalfe DD. Proposed Diagnostic Algorithm for Patients with Suspected Mast Cell Activation Syndrome. J Allergy Clin Immunol Pract. 2019 Apr;7(4):1125-1133.e1. doi: </ref> | * Hypotension<ref>Valent P, Akin C, Bonadonna P, Hartmann K, Brockow K, Niedoszytko M, Nedoszytko B, Siebenhaar F, Sperr WR, Oude Elberink JNG, Butterfield JH, Alvarez-Twose I, Sotlar K, Reiter A, Kluin-Nelemans HC, Hermine O, Gotlib J, Broesby-Olsen S, Orfao A, Horny HP, Triggiani M, Arock M, Schwartz LB, Metcalfe DD. Proposed Diagnostic Algorithm for Patients with Suspected Mast Cell Activation Syndrome. J Allergy Clin Immunol Pract. 2019 Apr;7(4):1125-1133.e1. doi: </ref> | ||
| Line 104: | Line 104: | ||
* Gastrointestinal | * Gastrointestinal | ||
* Cardiovascular: light-headed, disregulated heart rate, inflammation | * [[Cardiovascular Disease|Cardiovascular]]: light-headed, disregulated heart rate, inflammation | ||
* Skeletal: bone pain, osteoporosis | * Skeletal: bone pain, [[osteoporosis]] | ||
* Cutaneous: hives, flushing | * Cutaneous: hives, flushing | ||
* Urinary: bladder irritation | * Urinary: bladder irritation | ||
| Line 150: | Line 150: | ||
# Infectious diseases | # Infectious diseases | ||
# Gastrointestinal diseases and IBS | # Gastrointestinal diseases and IBS | ||
# Celiac Disease | # [[Celiac Disease (Coeliac Disease)|Celiac Disease]] | ||
# Adrenal insufficiency | # Adrenal insufficiency | ||
# Cardiovascular disorders and myocardial infarction | # Cardiovascular disorders and myocardial infarction | ||
| Line 170: | Line 170: | ||
Because there are many possible triggers for MCAS, it is important that the fisioterapist recognize and help those with suspected disease avoid potential triggers both in the clinic and in everyday life. | Because there are many possible triggers for MCAS, it is important that the fisioterapist recognize and help those with suspected disease avoid potential triggers both in the clinic and in everyday life. | ||
Some of the most relevant triggers in the rehabilitation facility and scope of the physiotherapy practice include: exercise, medication ( opioids, NSAIDS, local anesthetics) changes in body temperature, friction, and vibration. | Some of the most relevant triggers in the rehabilitation facility and scope of the physiotherapy practice include: exercise, medication ( opioids, NSAIDS, local anesthetics) changes in body temperature, friction, and vibration.<ref>Boyden SE, Desai A, Cruse G, Young ML, Bolan HC, Scott LM, et al. Vibratory Urticaria Associated with a Missense Variant in ADGRE2. N Engl J Med. 2016 Feb 18;374(7):656-63. <nowiki>http://www.ncbi.nlm.nih.gov/pubmed/26841242</nowiki></ref><ref>Akin C, Metcalfe DD. Mastocytosis and mast cell activation syndromes presenting as anaphylaxis. In: Castells MC, editor. Anaphylaxis and hypersensitivity reactions. New York: Humana Press; 2011. p. 245-56. <nowiki>http://dx.doi.org/10.1007/978-1-60327-951-2_15</nowiki></ref><ref>Jennings S, Russell N, Jennings B, Slee V, Sterling L, Castells M, et al. The Mastocytosis Society survey on mast cell disorders: patient experiences and perceptions. J Allergy Clin Immunol Pract. 2014 Jan-Feb;2(1):70-6. <nowiki>http://www.ncbi.nlm.nih.gov/pubmed/24565772</nowiki></ref> | ||
Other common relevant triggers include: food allergy, increased stress, environmental allergens, infection, and venoms (bee/wasp, snake, spider, fire ant, etc). | Other common relevant triggers include: food allergy, increased emotional and situational stress, environmental allergens, infection, and venoms (bee/wasp, snake, spider, fire ant, etc). | ||
==== Elhers-Danlos Syndrome (EDS) and Hypermobility Sprectum disorders (HSD) ==== | ==== Elhers-Danlos Syndrome (EDS) and Hypermobility Sprectum disorders (HSD) ==== | ||
Because mast cells are so intertwined in the connective tissues where they reside, there is the possibility that they play a distinct role in connective tissue related autoimmune dysfunctions, although the link between the two is still not clear. In hypermobility dysfunctions the chronic release of mast cell factors may be the link between the hypermobility disorder and the autoimmune disorder. It is hypothesized that the connection between MCAS and hEDS/HSD may be due to the presence of Tryptase and Histamine (as well as other mast cell mediators) who also play a role in promoting the proliferation of fibroblasts and collagen production. <ref name=":8">Monaco A, Choi D, Uzun S, Maitland A, Riley B. Association of mast-cell-related conditions with hypermobile syndromes: a review of the literature. Immunol Res. 2022 Aug;70(4):419-431. doi: 10.1007/s12026-022-09280-1. Epub 2022 Apr 21. PMID: 35449490; PMCID: PMC9022617.</ref><ref>Seneviratne SL, Maitland A, Afrin L. Mast cell disorders in Ehlers-Danlos syndrome. Am J Med Genet C Semin Med Genet. 2017;175:226–236. doi: 10.1002/ajmg.c.31555. [PubMed] [CrossRef] [Google Scholar]</ref> There are also many shared clinical features between MCAS and hEDS/HSD. <ref name=":8" /> The understanding of this connection may allow the physiotherapist to identify patients with unexplained symptoms and refer them for further diagnosis. | Because mast cells are so intertwined in the connective tissues where they reside, there is the possibility that they play a distinct role in connective tissue related autoimmune dysfunctions, like [https://www.physio-pedia.com/Ehlers-Danlos_Syndrome?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal Elhers-Danlos Syndrome], although the link between the two is still not clear. In hypermobility dysfunctions the chronic release of mast cell factors may be the link between the hypermobility disorder and the autoimmune disorder. It is hypothesized that the connection between MCAS and hEDS/HSD may be due to the presence of Tryptase and Histamine (as well as other mast cell mediators) who also play a role in promoting the proliferation of fibroblasts and collagen production. <ref name=":8">Monaco A, Choi D, Uzun S, Maitland A, Riley B. Association of mast-cell-related conditions with hypermobile syndromes: a review of the literature. Immunol Res. 2022 Aug;70(4):419-431. doi: 10.1007/s12026-022-09280-1. Epub 2022 Apr 21. PMID: 35449490; PMCID: PMC9022617.</ref><ref>Seneviratne SL, Maitland A, Afrin L. Mast cell disorders in Ehlers-Danlos syndrome. Am J Med Genet C Semin Med Genet. 2017;175:226–236. doi: 10.1002/ajmg.c.31555. [PubMed] [CrossRef] [Google Scholar]</ref> There are also many shared clinical features between MCAS and hEDS/HSD. <ref name=":8" /> The understanding of this connection may allow the physiotherapist to identify patients with unexplained symptoms and refer them for further diagnosis. | ||
==== Urticaria ==== | ==== Urticaria ==== | ||
[[Urticaria]] is prevelant both in EDS and MCAS. Basophils and mast cells are most commonly responsible for the urticaria/flushing <ref name=":8" /><ref name=":9">Szalewski RJ, Davis BP. Ehlers-Danlos Syndrome is associated with Idiopathic Urticaria-a retrospective study [abstract]. J Allergy Clin Immunol. 2019;143. 10.1016/j.jaci.2018.12.204.</ref><ref>Greiwe J. An index case of a rare form of inducible urticaria successfully treated with omalizumab [abstract] Ann Allergy Asthma Immunol. 2018;121:S84. doi: 10.1016/j.anai.2018.09.273. </ref> but there is no direct cause found as of yet, and may be just a result of the mast cell disease alone. | |||
Connections have also been drawn between Lupus erythematosus (SLE) and chronic spontaneous urticaria as a result of mast cell dysfunction. | |||
Connections have also been drawn between Lupus erythematosus (SLE) and chronic spontaneous urticaria as a result of | |||
==== Rheumatoid arthritis (RA) ==== | ==== Rheumatoid arthritis (RA) ==== | ||
[[Rheumatoid Arthritis]] is chronic autoimmune disease caused by the inflammation of the synovium surrounding joints. It commonly attacks smaller joint of the body, but can also affect larger joints). Various immune cells are found in the synovium including T cells, B cells, and mast cells leading to the synovitis and disease process.<ref>Pitzalis C, Kelly S, Humby F. New learnings on the pathophysiology of RA from synovial biopsies. Curr Opin Rheumatol. 2013;25:334–344. </ref> | |||
Studies have shown with histological evidence that there are increased numbers of mast cells in the joint synovium in people who present with RA versus those of a control group.<ref>Malmstrom V, Catrina AI, Klareskog L. The immunopathogenesis of seropositive rheumatoid arthritis: from triggering to targeting. Nat Rev Immunol. 2017;17:60–75. [PubMed] [Google Scholar]</ref>. Different phenotypes of synovitis have been found in relation to the density of mast cells in the synovium.<ref name=":9" /> Other studies show the increased number of mast cells or IgE mediated cells in the synovium of joints in of people with RA. This contributes to the degradation of the synovium and in some cases the cartilage and bone. <ref>Crisp AJ, Chapman CM, Kirkham SE, Schiller AL, Krane SM. Articular mastocytosis in rheumatoid arthritis. Arthritis Rheum. 1984;27:845–851. [PubMed] [Google Scholar]</ref> | Studies have shown with histological evidence that there are increased numbers of mast cells in the joint synovium in people who present with RA versus those of a control group.<ref>Malmstrom V, Catrina AI, Klareskog L. The immunopathogenesis of seropositive rheumatoid arthritis: from triggering to targeting. Nat Rev Immunol. 2017;17:60–75. [PubMed] [Google Scholar]</ref>. Different phenotypes of synovitis have been found in relation to the density of mast cells in the synovium.<ref name=":9" /> Other studies show the increased number of mast cells or IgE mediated cells in the synovium of joints in of people with RA. This contributes to the degradation of the synovium and in some cases the cartilage and bone. <ref>Crisp AJ, Chapman CM, Kirkham SE, Schiller AL, Krane SM. Articular mastocytosis in rheumatoid arthritis. Arthritis Rheum. 1984;27:845–851. [PubMed] [Google Scholar]</ref> | ||
==== Multiple Sclerosis ==== | ==== Multiple Sclerosis ==== | ||
There has also been a connection noted between MCAS and multiple sclerosis that would benefit from continued research.<ref>Conti P, Shaik-Dasthagirisaheb Mast cell serotonin immunoregulatory effects impacting on neuronal function: implications for neurodegenerative and psychiatric disorders. Neurotox Res. 2015;28:147–53. doi: 10.1007/s12640-015-9533-0. [PubMed] [CrossRef] [Google Scholar]</ref> <ref>Kolkhir PV, Olisova OY, Kochergin NG, Sulaimanov SA. Chronic urticaria: diagnostic approach practiced by medical specialists and general practitioners of Russia. Russ J Skin Vener Dis. 2015;18:45–51. doi: 10.17816/dv36963. [CrossRef] [Google Scholar]</ref><ref>Min HK, Kim K, Lee S, Kim H. Roles of mast cells in rheumatoid arthritis. Korean J Intern Med. 2020;35:12–24. doi: 10.3904/kjim.2019.271. [PMC free article] [PubMed] [CrossRef] [Google Scholar]</ref> | There has also been a connection noted between MCAS and [[multiple sclerosis]] that would benefit from continued research.<ref>Conti P, Shaik-Dasthagirisaheb Mast cell serotonin immunoregulatory effects impacting on neuronal function: implications for neurodegenerative and psychiatric disorders. Neurotox Res. 2015;28:147–53. doi: 10.1007/s12640-015-9533-0. [PubMed] [CrossRef] [Google Scholar]</ref> <ref>Kolkhir PV, Olisova OY, Kochergin NG, Sulaimanov SA. Chronic urticaria: diagnostic approach practiced by medical specialists and general practitioners of Russia. Russ J Skin Vener Dis. 2015;18:45–51. doi: 10.17816/dv36963. [CrossRef] [Google Scholar]</ref><ref>Min HK, Kim K, Lee S, Kim H. Roles of mast cells in rheumatoid arthritis. Korean J Intern Med. 2020;35:12–24. doi: 10.3904/kjim.2019.271. [PMC free article] [PubMed] [CrossRef] [Google Scholar]</ref> | ||
* | * | ||
== Resources <br> == | == Resources <br> == | ||
[https://tmsforacure.org/symptoms/symptoms-and-triggers-of-mast-cell-activation/ Mast cell Disease Society] | |||
[https://www.aaaai.org/conditions-treatments/related-conditions/mcas American Academy of Allergy, Asthma & Immunology] | |||
Case Study hosted by Jeannie Di Bon: [https://youtu.be/9jhG4WTu__U Living with Mast Cell Activation Syndrome] | |||
[https://youtu.be/unUVf-vbLbA What is Mast Cell Activation Syndrome:] Dr. Arnold Deering | |||
== References == | == References == | ||
<references /> | <references /> | ||
Revision as of 01:04, 28 November 2022
Top Contributors - Zeina Grifoni, Lucinda hampton, Carina Therese Magtibay and Kim Jackson
Introduction/Definition[edit | edit source]
Mast Cell Activation Syndrome (MCAS) is one of several Mast Cell diseases (MCD) . It is particularly hard to identify and is often misdiagnosed or left unreckogonized for many years. It prenests with a wide range of differing symptoms and can be the result of many different triggers that are not always consistent across the population of these infected and can be inconsistent even within the individual who suffers from MCAS.
Mast cell activation is a normal response in our bodies to the introduction of potentially harmful triggers. The activation of the mast cells can be a result of an IgE mediated response or a non- IgE mediated response [1]the reactions of which, in both cases can vary from mild to severe and include a wide range of varied symptoms. [2] Mast cell Activation Syndrome occurs when there is an over-reaction and/or inappropriate reaction of the mast cells to a stimuli, known or unrecognized, that can not be explained by any other disease.
3 types of mat cell activation: [3]
- Monoclonal (primary):
- This is a rare form of the dysfunction.
- It is the result of over-profiletarion of mast cells and usually involves mutations in the KIT gene or aberrant expression of the CD25 or CD2.
- Monoclonal mast cell activation syndrome can also be a result of mastocytosis.
- Secondary (non-clonal):
- There is a normal level of mast cell production in the tissues.
- Mast cells are inappropriately activated as an allergic reaction to typically harmful triggers creating either a heightened IgE or non-IgE mediated response.
- Idiopathic:
- No defined allergic or autoimmune cause has been identified for the diagnosis of idiopathic mast cell activation syndrome.
- It is a non-clonal/secondary idiopathic MCAS.
- This is likely more prevalent than the other forms ( 1 and 2 above) of mast cell activation syndrome.
While these categories have been set, many people suffer from more than one type of mast cell activation which can lead to severe life threatening reactions and anaphylaxis.[1]
MCAS also has correlations with other orthopedic diseases. While MCAS has been recognized for many decades, there is still much research needed in order to understand the causes, triggers, and the many potential systemic effects.
Clinically Relevant Anatomy[edit | edit source]
Mast cells are granular cells that originate from bone marrow and are distributed throughout the body residing in a wide variety of tissues including but not limited to skin and connective tissues, the GI system, and the respiratory system. They are most commonly located near blood vessels, mucosa, and lymph. [4] Mediators are found in the membranes surrounding the granules and are released into the environment as a response to allergens. This release results in an inflammatory response that also recruits other immune cells to be released in the region. [5][6]
For a mast cell to survive, it first binds onto a stem cell factor in the bone marrow, KIT (a transmembrane tyrosine kinase receptor) [7] , and then it adapts using environmental cues to the cell’s phenotype where it resides becoming a mature mast cell. [8]They are influenced by many factors including: Interleukin-3, 4, 9 and transforming growth factor beta1. [9]
There are 2 types of mast cells:
- MCT - connective tissue, skin, peritoneal cavity (T for tryptase in the granules). They express interleukin-5 and 6.
- MCTC- gut and respiratory mucosa (TC for tryptase and chymase). They express interleukin-4. [8]
Common mediators released in the mast cell response:
- Histamine
- Leukotrines
- Prostaglandins
- Tryptase
- Interleukins
- Heparin
- Tumor necrosis factor
Mechanism / Pathological Proces[edit | edit source]
Mast cells coordinate an immune response to pathogens through surface receptors, receptors for adenosine phosphate, estrogen, and immunoglobulins, physical stimuli (pressure and temperature), and toxins.
Mast cells main role of creating an immune response to potentially harmful stimuli and pathogens is initiated when surface receptors for adenosine phosphate, estrogen, and immunoglobulins, physical stimuli (pressure and temperature), and toxins become active. This leads to the synthesis of an increased number of mediators and the release histamine and proteases. This, in turn, leads to an increased production of prostaglandins and leukotrienes (lipid-derived mediators) and many pro and anti-inflammatory cytokines and chemokines. The result of mast cell response can vary greatly intensity. It can be as small as the red bump around a mosquito bite or a full anaphylactic reaction.[5][6][10]
Mast cells, in addition to the allergic response, have many other functions in the cell. They are responsible for homeostasis, phagocytosis, cytokine and chemokine production, and the immediate release of vasoactive substances.[11] Mast cells are found within tissues as opposed to other immune cells which are located outside of cells. They are surrounded by nerves, blood vessels, and lymphatic vessels.
Clinical Presentation[edit | edit source]
There are a wide variety of clinical symptoms associated with Mast Cell Activation Syndrome. Some of the variation in symptoms and clinical presentation are due to the different mediators that may be released by the mast cell in response to a noxious stimulus. In addition, for people who have MCAS, the body’s response to a specific stimulus is unpredictable and the level of immune reaction that occurs may change with recurrent exposures. Often, because of the amount of mast cells in the Gastrointestinal tract, there are a host of GI symptoms present.
Common Complaints[edit | edit source]
Some of the most common complaints and symptoms include but are not limited to:[5][12]
- Flushing, itching, and skin rash, skin lesions, and/ or redness
- Fatigue , headaches, body aches
- Osteoporosis, bone pain
- Gastrointestinal symptoms including
- bloating, pain, nausea, diarrhea, GERD, IBS symptoms
- Throat swelling, shortness of breath
- Cramping
- Weight loss and enlarged lymph nodes
- Problems with clotting and bleeding
Correlates[edit | edit source]
There have also been many non-specific correlates to MCAS, and while there is mounting evidence in favor of correlations between these issues and MCAS, more research is necessary to fully understand how mast cell activation directly causes them.
- Nasal congestion
- Neurological symptoms
- Fatigue and Fibromyalgia like pain
- Rashes
- Psychiatric and neurological disorders
- Elhers-Danlos syndrome
- Postural Orthostatic tachycardia syndrome (POTS) [13]
- Celiac disease and gluten intolerances[12]
- Autoimmune disorders
- Hypotension[14]
Because MCAS is episodic and unpredictable and the range of severity of triggers can change over time and in the same individual, the identification of these correlates in the diagnosis of MCAS is not recommended.
Diagnostic Procedures[edit | edit source]
MCAS can be difficult to diagnose. There are three specific criteria, of which all must be met, to have a true diagnosis of MCAS. [1][13]
- Systemic symptoms (involving a minimum of 2 organ systems) of mast cell activation that are severe and recurrent
- Noted activation or elevated mast cells
- A response to treatment with mast cell stabilizer or mast cell mediator therapy, mast cell blockers like histamine receptor blockers
Organ systems commonly recognized for diagnosis are as follows:
- Ear, nose, throat
- Gastrointestinal
- Cardiovascular: light-headed, disregulated heart rate, inflammation
- Skeletal: bone pain, osteoporosis
- Cutaneous: hives, flushing
- Urinary: bladder irritation
Testing and Measures[edit | edit source]
- Serum testing:
- Primary testing for MCAS is based on values found of the Tryptase release through serum testing. The threshold for serum Tryptase is 20% above baseline plus 2ng/ml. The blood sample needs to be collected within 4 hours of symptomatic episode, and then compared to baseline. If there is no already known baseline levels, testing for baseline must be done 24-48 hours after the activation episode. While this is the best test to rule in MCAS, a negative result does not necessarily rule out MCAS because so much of the test relies on timing of the sample collection during the reaction process.
- Urinary testing:
- Urinary testing has been done to in order to identify mediators from a mast cell response in the urine within 24 hours of the reaction taking place. The test must also correspond to the case story and historical symptoms. Testing is checking the levels of N-methylhsitamine and prostaglandins D2, metabolyte 11β , prostaglandin F2α,DM, leukotrienes E4 or MIAA. [5]
- Test by treatment:
- While not as objectively measurable, this method offers a diagnosis for MCAS if treatment for it is successful (As in the 3rd diagnostic requirement).
- Endoscopy:
- An endoscopy may show elevated or mast cell numbers in the GI tract but is much more invasive and not commonly used as a diagnostic procedure.
Management / Interventions[edit | edit source]
Treatments for MCAS consist of both medication and lifestyle management. The best treatment is to avoid and triggers of the disease. Due to the nature of the disease, however, it can be very difficult to know what the triggers are.
Mast cells also tend to be overactive in stressful situations, so strategies of stress management of stress may be helpful in decreasing activity of the mast cells resulting in fewer or less intense reactive episodes.
For those with secondary MCAS who respond to venom /IgE induced MCAS, immunotherapy may be recommended. [15][16][17]
The purpose medicinal treatment is to manage the immediate symptoms because only when the symptoms have been decreased can the range of triggers be reduced. Treatment for severe presentations of MCAS may need lifelong immunotherapy, Anti- IgE therapy, or pharmacological therapy.[1]
Medications:
- H1 antihistamines may stabilize the mast cells and reduce the acute allergy symptoms like: itching, rashes, flushing and headaches, and brain fog.
- 1st generation H1 antihistamines include: Hydroxyzine Hydrochloride, Diphenhydramine, Chloroheniramine, Doxepin Hydrochloride, Ketotifen
- 2nd generation H1 antihistamines usually cuase less drowsiness and include: Fexofenadine, Loratidine, Desloratidine, Levocetirixine, Cetirizine.[1]
- H2 antihistamines also help with mast cell stability and reduction of symptoms, but may also help reduce GI symptoms. These include: famotidine and cimetidine.[1]
- Mast cell stabilizers and Glucocorticosteroids may reduce GI symptoms and brain fog.
- Mast Cell targeted drugs or broadly acting Tyrosine kinase inhibitors. Some of these will block no only the over production of mast cells but also the IgE activation. [18]
- Aspirin therapy for elevated prostaglandins will help with brain fog, bone pain, and flushing but needs to be taken in high doses that may be difficult to tolerate.[18][19][20]
A combination of therapies may be required to dampen MCAS based on the presentation and disease precess of each individual.[19]
Differential Diagnosis[edit | edit source]
MCAS is difficult to diagnoses due to the diverse range of symptoms and varied presentation. It is therefore necessary to complete a thorough differential diagnosis ruling out other possible causes for the presenting symptoms.[1] [3]
Syndromes/diseases to be considered include:[3]
- Infectious diseases
- Gastrointestinal diseases and IBS
- Celiac Disease
- Adrenal insufficiency
- Cardiovascular disorders and myocardial infarction
- Phychological factors
- Oncologic disorders
- Endocrine dysfunctions
- Toxicity
Other mast cell diseases should also be ruled out including:
- Systemic Mastocytosis (SM)
- Cutaneous mastocytosis (CM)
- Smoldering mastocytosis (SSM)
- Hereditary alpha tryptasemia (HaT)
Relevance in Physiotherapy[edit | edit source]
Because there are many possible triggers for MCAS, it is important that the fisioterapist recognize and help those with suspected disease avoid potential triggers both in the clinic and in everyday life.
Some of the most relevant triggers in the rehabilitation facility and scope of the physiotherapy practice include: exercise, medication ( opioids, NSAIDS, local anesthetics) changes in body temperature, friction, and vibration.[21][22][23]
Other common relevant triggers include: food allergy, increased emotional and situational stress, environmental allergens, infection, and venoms (bee/wasp, snake, spider, fire ant, etc).
Elhers-Danlos Syndrome (EDS) and Hypermobility Sprectum disorders (HSD)[edit | edit source]
Because mast cells are so intertwined in the connective tissues where they reside, there is the possibility that they play a distinct role in connective tissue related autoimmune dysfunctions, like Elhers-Danlos Syndrome, although the link between the two is still not clear. In hypermobility dysfunctions the chronic release of mast cell factors may be the link between the hypermobility disorder and the autoimmune disorder. It is hypothesized that the connection between MCAS and hEDS/HSD may be due to the presence of Tryptase and Histamine (as well as other mast cell mediators) who also play a role in promoting the proliferation of fibroblasts and collagen production. [24][25] There are also many shared clinical features between MCAS and hEDS/HSD. [24] The understanding of this connection may allow the physiotherapist to identify patients with unexplained symptoms and refer them for further diagnosis.
Urticaria[edit | edit source]
Urticaria is prevelant both in EDS and MCAS. Basophils and mast cells are most commonly responsible for the urticaria/flushing [24][26][27] but there is no direct cause found as of yet, and may be just a result of the mast cell disease alone.
Connections have also been drawn between Lupus erythematosus (SLE) and chronic spontaneous urticaria as a result of mast cell dysfunction.
Rheumatoid arthritis (RA)[edit | edit source]
Rheumatoid Arthritis is chronic autoimmune disease caused by the inflammation of the synovium surrounding joints. It commonly attacks smaller joint of the body, but can also affect larger joints). Various immune cells are found in the synovium including T cells, B cells, and mast cells leading to the synovitis and disease process.[28]
Studies have shown with histological evidence that there are increased numbers of mast cells in the joint synovium in people who present with RA versus those of a control group.[29]. Different phenotypes of synovitis have been found in relation to the density of mast cells in the synovium.[26] Other studies show the increased number of mast cells or IgE mediated cells in the synovium of joints in of people with RA. This contributes to the degradation of the synovium and in some cases the cartilage and bone. [30]
Multiple Sclerosis[edit | edit source]
There has also been a connection noted between MCAS and multiple sclerosis that would benefit from continued research.[31] [32][33]
Resources
[edit | edit source]
American Academy of Allergy, Asthma & Immunology
Case Study hosted by Jeannie Di Bon: Living with Mast Cell Activation Syndrome
What is Mast Cell Activation Syndrome: Dr. Arnold Deering
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 Akin C. Mast cell activation syndromes. J Allergy Clin Immunol. 2017 Aug;140(2):349-355. doi: 10.1016/j.jaci.2017.06.007. PMID: 28780942.
- ↑ Anvari S, Miller J, Yeh CY, Davis CM. IgE-Mediated Food Allergy. Clin Rev Allergy Immunol. 2019 Oct;57(2):244-260. doi: 10.1007/s12016-018-8710-3. PMID: 30370459.
- ↑ 3.0 3.1 3.2 https://tmsforacure.org/overview/mast-cell-activation-syndrome-variants/
- ↑ Moon TC, St Laurent CD, Morris KE, Marcet C, Yoshimura T, Sekar Y, Befus AD. Advances in mast cell biology: new understanding of heterogeneity and function. Mucosal Immunol. 2010 Mar;3(2):111-28. doi: 10.1038/mi.2009.136. Epub 2009 Dec 30. PMID: 20043008.
- ↑ 5.0 5.1 5.2 5.3 Valent P, Akin C, Arock M, Brockow K, Butterfield JH, Carter MC, et al. Definitions, criteria and global classification of mast cell disorders with special reference to mast cell activation syndromes: a consensus proposal. Int Arch Allergy Immunol. 2012;157(3):215-25.
- ↑ 6.0 6.1 Valent P. Mast cell activation syndromes: definition and classification. Allergy. 2013 Apr;68(4):417-24.
- ↑ Moon TC, St Laurent CD, Morris KE, Marcet C, Yoshimura T, Sekar Y, Befus AD. Advances in mast cell biology: new understanding of heterogeneity and function. Mucosal Immunol. 2010 Mar;3(2):111-28. doi: 10.1038/mi.2009.136. Epub 2009 Dec 30. PMID: 20043008.
- ↑ 8.0 8.1 Fong M, Crane JS. Histology, Mast Cells. [Updated 2022 May 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK499904/
- ↑ Galli SJ, Borregaard N, Wynn TA. Phenotypic and functional plasticity of cells of innate immunity: macrophages, mast cells and neutrophils. Nat Immunol. 2011 Oct 19;12(11):1035-44. doi: 10.1038/ni.2109. PMID: 22012443; PMCID: PMC3412172.
- ↑ Cardamone C, Parente R, Feo GD, Triggiani M. Mast cells as effector cells of innate immunity and regulators of adaptive immunity. Immunol Lett. 2016 Oct;178:10-4. doi: 10.1016/j.imlet.2016.07.003. Epub 2016 Jul 5. PMID: 27393494.
- ↑ 1.Valent P, Akin C, Bonadonna P, Hartmann K, Brockow K, Niedoszytko M, Nedoszytko B, Siebenhaar F, Sperr WR, Oude Elberink JNG, Butterfield JH, Alvarez-Twose I, Sotlar K, Reiter A, Kluin-Nelemans HC, Hermine O, Gotlib J, Broesby-Olsen S, Orfao A, Horny HP, Triggiani M, Arock M, Schwartz LB, Metcalfe DD. Proposed Diagnostic Algorithm for Patients with Suspected Mast Cell Activation Syndrome. J Allergy Clin Immunol Pract. 2019 Apr;7(4):1125-1133.e1. doi: 10.1016/j.jaip.2019.01.006. Epub 2019 Feb
- ↑ 12.0 12.1 Theoharides TC, Valent P, Akin C. Mast cells, mastocytosis, and related disorders. New England Journal of Medicine. 2015 Jul 9;373(2):163-72.
- ↑ 13.0 13.1 Matito A, Escribese MM, Longo N, Mayorga C, Luengo-Sánchez O, Pérez-Gordo M, Matheu V, Labrador-Horrillo M, Pascal M, Seoane-Reula ME; Comité de Inmunología de la Sociedad Española de Alergología e Inmunología Clínica (SEAIC). Clinical Approach to Mast Cell Activation Syndrome: A Practical Overview. J Investig Allergol Clin Immunol. 2021 Dec 21;31(6):461-470. doi: 10.18176/jiaci.0675. Epub 2020 Feb 5. PMID: 33541851.
- ↑ Valent P, Akin C, Bonadonna P, Hartmann K, Brockow K, Niedoszytko M, Nedoszytko B, Siebenhaar F, Sperr WR, Oude Elberink JNG, Butterfield JH, Alvarez-Twose I, Sotlar K, Reiter A, Kluin-Nelemans HC, Hermine O, Gotlib J, Broesby-Olsen S, Orfao A, Horny HP, Triggiani M, Arock M, Schwartz LB, Metcalfe DD. Proposed Diagnostic Algorithm for Patients with Suspected Mast Cell Activation Syndrome. J Allergy Clin Immunol Pract. 2019 Apr;7(4):1125-1133.e1. doi:
- ↑ Niedoszytko M., Bonadonna P., Elberink J.N.G.O., Golden D.B.K. Epidemiology, diagnosis, and treatment of hymenoptera venom allergy in mastocytosis patients. Immunol. Allergy Clin. North Am. 2014;34:365–381. doi: 10.1016/j.iac.2014.02.004.
- ↑ Bonadonna P., Bonifacio M., Lombardo C., Zanotti R. Hymenoptera allergy and mast cell activation syndromes. Curr. Allergy Asthma Rep. 2016;16 doi: 10.1007/s11882-015-0582-5.
- ↑ Bonadonna P., Bonifacio M., Lombardo C., Zanotti R. Hymenoptera allergy and mast cell activation syndromes. Curr. Allergy Asthma Rep. 2016;16 doi: 10.1007/s11882-015-0582-5.
- ↑ 18.0 18.1 Valent P, Akin C, Nedoszytko B, Bonadonna P, Hartmann K, Niedoszytko M, Brockow K, Siebenhaar F, Triggiani M, Arock M, Romantowski J, Górska A, Schwartz LB, Metcalfe DD. Diagnosis, Classification and Management of Mast Cell Activation Syndromes (MCAS) in the Era of Personalized Medicine. Int J Mol Sci. 2020 Nov 27;21(23):9030. doi: 10.3390/ijms21239030. PMID: 33261124; PMCID: PMC7731385.
- ↑ 19.0 19.1 Valent P., Akin C., Hartmann K., George T.I., Sotlar K., Peter B., Gleixner K.V., Blatt K., Sperr W.R., Manley P.W., et al. Midostaurin: A magic bullet that blocks mast cell expansion and activation. Ann. Oncol. 2017;28:[[1]]. doi: 10.1093/annonc/mdx290.
- ↑ Krauth M.T., Mirkina I., Herrmann H., Baumgartner C., Kneidinger M., Valent P. Midostaurin (PKC412) inhibits immunoglobulin E-dependent activation and mediator release in human blood basophils and mast cells. Clin. Exp. Allergy. 2009;39:1711–1720. doi: 10.1111/j.1365-2222.2009.03353.x. [PubMed] [CrossRef] [Google Scholar]
- ↑ Boyden SE, Desai A, Cruse G, Young ML, Bolan HC, Scott LM, et al. Vibratory Urticaria Associated with a Missense Variant in ADGRE2. N Engl J Med. 2016 Feb 18;374(7):656-63. http://www.ncbi.nlm.nih.gov/pubmed/26841242
- ↑ Akin C, Metcalfe DD. Mastocytosis and mast cell activation syndromes presenting as anaphylaxis. In: Castells MC, editor. Anaphylaxis and hypersensitivity reactions. New York: Humana Press; 2011. p. 245-56. http://dx.doi.org/10.1007/978-1-60327-951-2_15
- ↑ Jennings S, Russell N, Jennings B, Slee V, Sterling L, Castells M, et al. The Mastocytosis Society survey on mast cell disorders: patient experiences and perceptions. J Allergy Clin Immunol Pract. 2014 Jan-Feb;2(1):70-6. http://www.ncbi.nlm.nih.gov/pubmed/24565772
- ↑ 24.0 24.1 24.2 Monaco A, Choi D, Uzun S, Maitland A, Riley B. Association of mast-cell-related conditions with hypermobile syndromes: a review of the literature. Immunol Res. 2022 Aug;70(4):419-431. doi: 10.1007/s12026-022-09280-1. Epub 2022 Apr 21. PMID: 35449490; PMCID: PMC9022617.
- ↑ Seneviratne SL, Maitland A, Afrin L. Mast cell disorders in Ehlers-Danlos syndrome. Am J Med Genet C Semin Med Genet. 2017;175:226–236. doi: 10.1002/ajmg.c.31555. [PubMed] [CrossRef] [Google Scholar]
- ↑ 26.0 26.1 Szalewski RJ, Davis BP. Ehlers-Danlos Syndrome is associated with Idiopathic Urticaria-a retrospective study [abstract]. J Allergy Clin Immunol. 2019;143. 10.1016/j.jaci.2018.12.204.
- ↑ Greiwe J. An index case of a rare form of inducible urticaria successfully treated with omalizumab [abstract] Ann Allergy Asthma Immunol. 2018;121:S84. doi: 10.1016/j.anai.2018.09.273.
- ↑ Pitzalis C, Kelly S, Humby F. New learnings on the pathophysiology of RA from synovial biopsies. Curr Opin Rheumatol. 2013;25:334–344.
- ↑ Malmstrom V, Catrina AI, Klareskog L. The immunopathogenesis of seropositive rheumatoid arthritis: from triggering to targeting. Nat Rev Immunol. 2017;17:60–75. [PubMed] [Google Scholar]
- ↑ Crisp AJ, Chapman CM, Kirkham SE, Schiller AL, Krane SM. Articular mastocytosis in rheumatoid arthritis. Arthritis Rheum. 1984;27:845–851. [PubMed] [Google Scholar]
- ↑ Conti P, Shaik-Dasthagirisaheb Mast cell serotonin immunoregulatory effects impacting on neuronal function: implications for neurodegenerative and psychiatric disorders. Neurotox Res. 2015;28:147–53. doi: 10.1007/s12640-015-9533-0. [PubMed] [CrossRef] [Google Scholar]
- ↑ Kolkhir PV, Olisova OY, Kochergin NG, Sulaimanov SA. Chronic urticaria: diagnostic approach practiced by medical specialists and general practitioners of Russia. Russ J Skin Vener Dis. 2015;18:45–51. doi: 10.17816/dv36963. [CrossRef] [Google Scholar]
- ↑ Min HK, Kim K, Lee S, Kim H. Roles of mast cells in rheumatoid arthritis. Korean J Intern Med. 2020;35:12–24. doi: 10.3904/kjim.2019.271. [PMC free article] [PubMed] [CrossRef] [Google Scholar]