Manual Therapy Techniques For The Lumbar Spine
Original Editors - Jenny Arnatt, Tabitha Eddleston, Victoria Jovcic, Lizzie Wakeham
Lead Editors - Your name will be added here if you are a lead editor on this page. Read more.
Introduction[edit | edit source]
This page is designed to look at .....
Low back Pain (LBP)
[edit | edit source]
Mobilisations[edit | edit source]
Joint mobilisation is a treatment technique which can be used to manage musculoskeletal dysfunction [1]Hertling et al (1996), by restoring the motion in the respective joint [2](Randall, 1992). The techniques are performed by physiotherapists, and fall under the category of manual therapy. Spinal mobilisation is described in terms of improving mobility in areas of the spine that are restricted [3](Korr 1977). Such restriction may be found in joints, connective tissues or muscles. By removing the restriction by mobilisation the source of pain is reduced and the patient experiences symptomatic relief. This results in gentle mobilisations being used for pain relief while more forceful, deeper mobilisations are effective for decreasing joint stiffness. [4] (Maitland 1986).
Definition: Mobilisations primarily consist of passive movements which can be classified as physiological or accessory [5](Porter, 2005). The purpose is to provide short term pain relief and to restore pain-free, functional movements by achieving full range at the joint [6](Maitland et al, 2005).
[edit | edit source]
Background[edit | edit source]
Contraindications/Precautions[edit | edit source]
• Neurological:
o D Patient with arm pain and neurological signs, from two nerve routes
o Disturbance of bladder and bowel function, or perineal anaesthesia
o Spinal cord symptoms
• Radiological changes
o D Patients with rheumatoid arthritis and osteoporosis are contraindications to forceful mobilizations.
• Patients with vertigo need close supervision
• Hypermobility
o If a vertebrae in the spine was hypermobile compared to the other vertebra, care must be taken to avoid putting excessive strain on the hypermobile joint
Effects[edit | edit source]
Mobilisations involving pressure onto the vertebra can be used to increase joint range of motion, and also to produce and analgesic effect.
Manual therapy and mobilisations can be used to treat 5 symptom groups:
• Pain
• Stiffness
• Pain associated with stiffness
• Momentary jabs of pain
• Disorders directly related to a specific diagnosis
Stiffness – patients whose joint stiffness is limiting normal function.
• Select movement that needs to be stretched, for physiological movements, then accessory movements should be used, all directions utilised.
• Pressure applied through the thumb or pisiform against the vertebrae in the direction of the movement that is stiff.
• Staccato techniques are used move a stiff joint through its maximum range before the bordering joints have time to start moving too. If there are no symptoms from the joint, then the speed of the staccato can be quicker, however, if symptoms are moderate, then the movements need to be more fluid.
• There is evidence to suggest that different segments of the lumbar spine will react slightly differently, for example; when a PA is performed on L3,4 and 5, then tend to move into extension, and all three segments will move in response to a PA on the neighbouring one. However with L1 and L2, the lower L3,4 and 5 segments moved into flexion. – need to be aware of the effect of a PA mobilisation on neighbouring vertebra segments (Powers et al, 2003)
Pain – patients who have severe pain that is limiting movement
• The joint being treated should be positioned in a symptom free way
• To decide between accessory movements and physiological movements, the one, which can be performed with the larges amplitude most comfortably for the patient, is used.
• If a joint is painful, oscillations in mobilisations should be smoothly and evenly so that changes between the on and off pressure cannot be detected.
• Accessory movements:
- Pressure is applied through the thumb or pisiform to produce large amplitude of movement, with very little pressure and without any degree of stiffness felt.
- The amplitude of the movement should be as large as possible without causing any pain. As symptoms improve, then the amplitude of the movements can increase gradually, although mobilisations have been shown to have a beneficial hypoalgesic regardless of amplitude. (Krouwel, Hebron and Willett, 2009)
• Physiological movements – when used should not cause any discomfort
- Any movements should be in the painless direction, in a large, slow, smooth manner, stopping before the onset of any discomfort. As the patient’s symptoms and ROM improve, the technique can be taken into a known and controlled degree of discomfort.
• Mobilisations can significantly decrease localised pain in the short term, about 24 hours, and can potentially lead to a greater decrease of pain long term compared to no treatment [7]
Grades of movement
• Mobilisation techniques can be performed in different positions of the range, using small or large amplitudes of movements, which are divided into four grades:
Grade Amplitude of movement
I A small-amplitude movement near the starting position of the range
II A large-amplitude of movement that carries well into the range. It can occupy any part of the range that is free of any stiffness or muscle spasm that does move into stiffness or muscle spasm
III Also a large-amplitude movement, but one that does move into stiffness or muscle spasm
IV A small-amplitude movement stretching into stiffness or muscle spasm
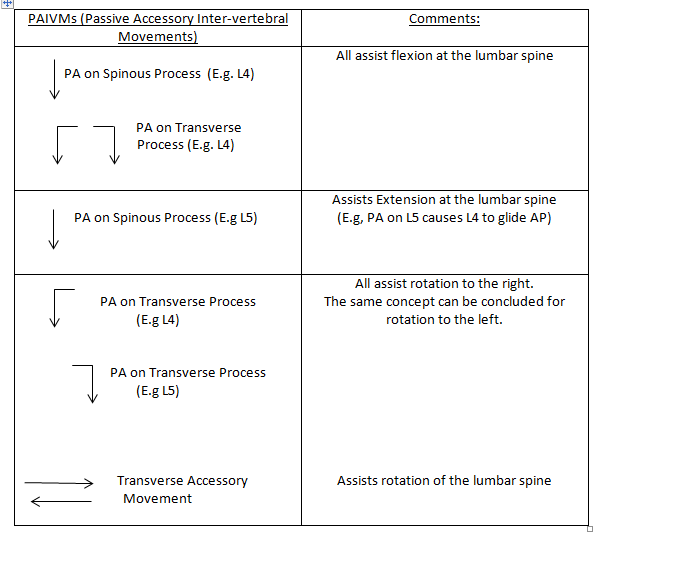
Mobilisations of the Lumbar Spine
[edit | edit source]
Central Posteroanterior (PA) Mobilisation Technique[edit | edit source]
For this manual therapy technique, the patient is often positioned in prone with their arms by their side and a pillow under their abdomen for comfort [8] (Powers et al, 2009). A PA mobilization is then performed by a physiotherpist by placing their thumb or pisiform over the spinous process of a vertebrae and applying a posteroanterior force.
PAs are a commonly used manual therapy technique that has shown to be effective at reducing pain in patients with low back pain (LBP) (Shum, Tsung and Lee, 2012). So far, evidence suggests immediate pain relief following treatment, and also some evidence suggests an increased range of movement (ROM) of lumbar extention (McCollam and Benson, 1993, Shum, Tsung and Lee, 2012, and Powers et al, 2009). However, literature is still variable on the overall effects of ROM and pain[9].
Mobilisations to increase lumbar flexion[edit | edit source]
During flexion, the superior vertebral body moves relatively forward and up on the vertebral body inferiorly[10]. Therefore, to aid flexion the mobilisation needs to be applied to the vertebra above the stiff/painful vertebra to facilitate the anterior-superior translation of the facet joints.
'Central Posteroanterior (PA) mobilisation': With the patient lying in prone, the therapist stands to the side of the patient and places their pisiform/ ulnar surface of their hand over the spinous process (SP) of the selected vertebra with their wrist in full extension. The other hand is then placed on top to reinforce. The therapist’s shoulders should be directly above the SP with the elbows slightly bent. The therapist then uses their body weight to apply a PA force to the selected SP by leaning their body over their arms and performing rocking movements to provide oscillatory movements of the vertebra.
On initial assessment and treatment, if the patient has very limited movement, a pillow can be placed underneath their abdomen, or the head end of plinth can be raised to position the Lumbar spine in relative extension. Similarly, if the patient cannot tollerate pressure directly through the spinous process, the therapist can apply pressure either side of the SP with either thumb on the transverse processes.
Equally, as the patient’s pain and stiffness reduces the position of the patient can be altered to increase flexion nearer to end of range. This can be done by either lowering the foot section of the plinth or kneeling the patient on the floor by the foot of the plinth with his trunk flexed over the plinth ( approx. 20 degrees flexion) [11]
Mobilisations with Movement (MWMs)[edit | edit source]
Definition: It is a manual therapy technique which was developed by Brian Mulligan, for the treatment of musculoskeletal dysfunction [12] (Jonas 2005). It involves performing a sustained force (accessory glide) while a previously painful (problematic) movement is performed[13] (Vicenzino 2009).
Usually, the technique is indicated if, during its application the technique enables the impaired joint to move more freely without pain or impediment[14] (Mulligan, 1993). Mulligan does not prescribe grades of movement or oscillatory movements. He prescribes taking the joint through its full range of movement and this entails taking it into resistance. When performing MWMs, the direction of the applied force is typically perpendicular to the plane of movement or impaired action and in some instances it is parallel to the treatment plane [15][16](Mulligan, 1992, 1993, 1996).
There have been reports of clinical cases and case serieswhich have described the success of MWMs in the management of various musculoskeletal conditions[17][18][19][20][21][22][23] (Stephens, 1995; Vicenzino and Wright, 1995; Hetherington, 1996; O’Brien and Vicenzino, 1998; Miller, 2000; Exelby, 2001; Folk, 2001). See Exelby, (2001) for success in MWMs in the lumbar spine.
MWMs to increase Flexion of the Lumbar Spine
[edit | edit source]
Technique 1[edit | edit source]
Starting position:
- Patient in side lying facing therapist.
- The patient's knees should be bent towards their chest in mid lumbar flexion and rested on the therapists hips.
- Therapist places forearms along the patients back to palpate between adjacent spinous processes.
Method:
- The therapist produces flexion and extension of the lumbar spine by swaying hips left to right (and vise versa)
- To isolate flexion, the problematic level is palpated and when passively moving the spine into flexion a sustained PA force is applied to the spinous process throughout the movement of flexion and then released.
N.B *Correct plinth height is essential for this technique.
** It may take multiple attempts of the MWMs to find the correct level of the lumbar spine to decrease pain and/or stiffness.
Technique 2[edit | edit source]
Starting Position:
- Patient in standing perpendicular to therapist.
- Therapist's need to stabilise pelvis via placing cup of hand other the ASIS.
- Therapist to palpate between adjacent spinous processes.
Method:
- The patient actively flexes lumbar spine and then extends to return to the neurtal position.
- To isolate flexion, again, the problematic level is palpated and when the patient actively moves into flexion, a sustained PA force is applied to the spinous process throughout the movement.
Technique 3[edit | edit source]
Starting Position:
- Patient in sitting, facing away from therapist.
- The pelvis is stabilised via a belt being placed around the patients ASIS's and around the therapist's ischeal tuberosity.
- Therapist to palpate between adjacent spinous processes.
Method:
- The patient actively flexes the lumbar spine and extends to a neutral position.
- The therapist maitains the tension on the belt throughout all movement.
- The problematic level is palpated and when the patient actively moves into flexion, a sustained PA force is applied throughout the whole movement of flexion to the spinous process.
N.B * The therapist should have bent knees and be able to lean onto the belt to increase the tension of the belt.
[24] Mulligan (1995)
Recording[edit | edit source]
Prescription of Mobilisations[edit | edit source]
Thus far, there is no definitive evidence for the optimum duration, frequency or amplitude for mobilisation techniques. Most researchers have investigated subject responces' to 3 cycles of 60 second mobilisation which have shown to have immeditate effects of local and widespread analgeia[25] [26][27]. However, the duration, rate and frequency of mobilsations should be tailored to the patient's irritability and the preference of both patient and therapist[28].Current guidlines suggest that non-specific LBP patients should recieve a 12 week course of manual therapy[29]
Moreover, it is generally agreed that the oscilliation depth and amplitude of movement is dependent on the patients symptoms.
If the patient's main symptom is pain then oscillation depth should remain shallow (<55%) and should be maintained within a pain free range (e.g. Grade I and II). However, if the patient's main complaint is of stiffness then the depth of oscillation can progress to end of range providing pain is tolerable (e.g. Grade III and IIII)
Maitland Scale of Mobilisations[30]:
Grade I - Small amplitude + slow oscillations in pain free zone (<25% ROM)
Grade II- Large amplitude + slow oscillations in pain free zone (<55% ROM)
Grade III- Large amplitude + slow oscillations mid to end of range
Grade IIII- Small amplitude + slow oscillations at end of range
References[edit | edit source]
- ↑ Hertling D., and R.M. Kessler. Management of Common Musculoskeletal Disorders. Baltimore: Lippincott, Williams &amp;amp;amp;amp;amp;amp;amp;amp; Wilkins, 1996.
- ↑ Randall et al, 1992
- ↑ Korr IM (1977): The neurobiologic mechanisms in manipulative therapy. New York, Plenum Press.
- ↑ Maitland GD (1986): Vertebral manipulation, 5th ed. Sydney, Butterworths.
- ↑ Porter, S., (2005) Dictionary of Physiotherapy. Elsevier. London.
- ↑ Maitland, G., Hengeveld. E., Banks, K. and English, K., (2005). Maitland's Vertebral Manipulation. 7th Edition. Elsevier. London
- ↑ Hanrahan S, Bonnie L, et al (2005) The short-term effects of joint mobilizations on acute mechanical low back dysfunction in collegiate athletes. Journal of athletic training 40(2)
- ↑ Powers, C.M., Beneck, G.J., Kulig, K., Landel, R.F. and Fredericson, M., 2008, "Effects of a Single Session of Posterior-to-Anterior Spinal Mobilization and Press-up Exercise on Pain Response and Lumbar Spine Extension in People with Nonspecific Low Back Pain", Journal of the American Physical Therapy Association
- ↑ Rubinstein, S.M., Assendelft, T.C.M., de Boer,M.R. and van Tulder, M.W., 2012, "Spinal Manipulative therapy for acute low-back pain (Review),Cochrane,Issue.12
- ↑ Palastanga, N., Soames, R. and Palastanga, Dot.,2008, Anatomy and human movement pocketbook, London, Churchill Livingstone.
- ↑ Maitland, G.D., Hengeveld. E., Banks, K. and English, K.eds., 2005,Vertebral Manipulation, Edition 7, London, Butterworth Heinsmann.
- ↑ Jonas. (2005). Mosby's Dictionary of Complementary and Alternative Medicine, Elsevier.. Available: http://medical-dictionary.thefreedictionary.com/mobilization+with+movement. Last accessed 11th Jan 2013.
- ↑ Vicenzino. (2009). Mulligans: Mobilisations with movement. Available: http://www.bmulligan.com/conference/downloads/vicenzino_keynote1_MUllConf09.pdf. Last accessed 11th Jan 2013.
- ↑ Mulligan B. Mobilisation with movement (MWM’s). Journal offckLRManual and Manipulative Therapy 1993;1:154–6.
- ↑ Mulligan B. Extremity joint mobilisations combined with movements.fckLRNew Zealand Journal of Physiotherapy 1992;20:28–9.
- ↑ Mulligan B. Mobilisations with movement (MWM’S) for the hip jointfckLRto restore internal rotation and flexion. Journal of Manual andfckLRManipulative Therapy 1996;4:35–6.
- ↑ Stephens G. Lateral epicondylitis. Journal of Manual and ManioulativefckLRTherapy 1995;3:50–8.
- ↑ Vicenzino B, Wright A. Effects of a novel manipulative physiotherapyfckLRtechnique on tennis elbow: a single case study. Manual TherapyfckLR1995;1(1):30–5.
- ↑ Hetherington B. Lateral ligament strains of the ankle: do they exist?fckLRManual Therapy 1996;1(5):274–5.
- ↑ O’Brien T, Vicenzino B. A study of the effects of Mulligan’sfckLRmobilization with movement treatment of lateral ankle pain usingfckLRa case study design. Manual Therapy 1998;3(2):78–84.
- ↑ Miller J. Case study: Mulligan concept management of ‘‘tennis elbow’’.fckLROrthopaedic Division Review 2000;3:45–7.
- ↑ Exelby L. The locked lumbar facet joint: intervention using mobilizationsfckLRwith movement. Manual Therapy 2001;6(2):116–21.
- ↑ Folk B. Traumatic thumb injury management using mobilization withfckLRmovement. Manual Therapy 2001;6(3):178–82.
- ↑ Mulligan. (1995). Spinal Mobilisations with Leg Movement (Further Mobilisations with Movement). Journal of Manipulative Therapy. 3 (1), pg25-7.
- ↑ Krouwel, O., Hebron, C. and Willett, E., 2010, "An investigation into the potential hypoalgesic effects of PA mobilisations on the lumbar spine as measured by pressure pain thresholds (PPT)",Manual Therapy, Vol. 15, Pp. 7-12
- ↑ Goodsell, M., Lee, M and Latimer, J., 2000, "Short-Term Effects of Lumbar Posteroanterior Mobilization in Individuals With Low-Back Pain",Journal of Manipulative and Physiological Theraputics, Vol. 23, No. 5.
- ↑ Willett, E., Hebron,C. and Krouwel, O., 2009, "The initial effects of different rates of mobilisations on pressure pain thresholds in asymptomatic subjects", Manual Therapy, Vol.15, Pp.173-178
- ↑ Maitland, G.D., Hengeveld. E., Banks, K. and English, K.eds., 2005,Vertebral Manipulation, Edition 7, London, Butterworth Heinsmann.
- ↑ N.I.C.E guidelines, 2009, Low back pain: Early management of persistent non-specific low back pain, National Institute for Health and Clinical Excellence, Manchester.
- ↑ Cenage, G., 2002, "Joint Mobilization and Manipulation", Encylopedia of Nursing &amp;amp;amp;amp;amp;amp;amp;amp;amp; Allied Health, Vol.3, accessed 8 January 2013 at [www.enotes.com/joint-mobilization-manipulation-reference/]