Lesser Occipital Nerve: Difference between revisions
No edit summary |
Kim Jackson (talk | contribs) No edit summary |
||
| (10 intermediate revisions by one other user not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original Editor '''- [[User: | '''Original Editor '''- [[User:Wendy Snyders|Wendy Snyders]] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Description == | == Description == | ||
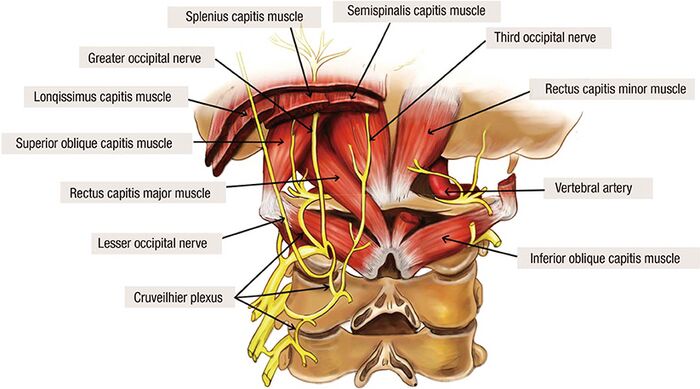
The lesser occipital nerve (LON), together with the greater occipital nerve (GON) and third occipital nerve innervate the occipital scalp<ref name=":0">Lee M, Brown M, Chepla K, Okada H, Gatherwright J, Totonchi A, Alleyne B, Zwiebel S, Kurlander D, Guyuron B. [https://www.drjeffreyjanis.com/wp-content/uploads/2017/02/Lee.pdf An anatomical study of the lesser occipital nerve and its potential compression points: implications for surgical treatment of migraine headaches.] Plastic and reconstructive surgery. 2013 Dec 1;132(6):1551-6.</ref>. Its location is highly variable but it reliably emerges from the posterior border of the sternocleidomastoid muscle<ref name=":1">Dash KS, Janis JE, Guyuron B. [https://www.migraine-surgery-centre.com/ae/assets/downloads/international_publications/ip5_lesser.pdf The lesser and third occipital nerves and migraine headaches.] Plastic and reconstructive surgery. 2005 May 1;115(6):1752-8.</ref><ref name=":2">Yu M, Wang SM. Anatomy, Head and Neck, Occipital Nerves. [Updated 2022 Oct 31]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK542213/</ref>. It then penetrates the deep cervical fascia and superior to the occiput, it communicates with the GON and innervates the skin<ref name=":2" />. The LON has been implicated in patients with occipital headaches<ref name=":0" /><ref>Peled ZM, Pietramaggiori G, Scherer S. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4874283/pdf/gox-4-e639.pdf Anatomic and compression topography of the lesser occipital nerve]. Plastic and Reconstructive Surgery Global Open. 2016 Mar;4(3).</ref>. | |||
[[File:ON anatomy.jpg|center|thumb|700x700px|<ref>Choi I, Jeon SR. Neuralgias of the head: occipital neuralgia. Journal of Korean Medical Science. 2016 Apr 1;31(4):479-88.</ref>]] | |||
=== Root === | === Root === | ||
The root is the lateral branch of the dorsal rami of the C2 and/or C3 spinal nerves<ref name=":0" /><ref name=":1" /><ref name=":2" />. | |||
=== Branches === | === Branches === | ||
It has three branches<ref name=":2" />: | |||
# auricular | |||
# mastoid | |||
# occipital | |||
== Function == | == Function == | ||
=== Sensory === | === Sensory === | ||
It provides the sensory innervation to the skin of the lateral neck, superior ear and postauricular skin<ref name=":1" />. | |||
== Clinical relevance == | == Clinical relevance == | ||
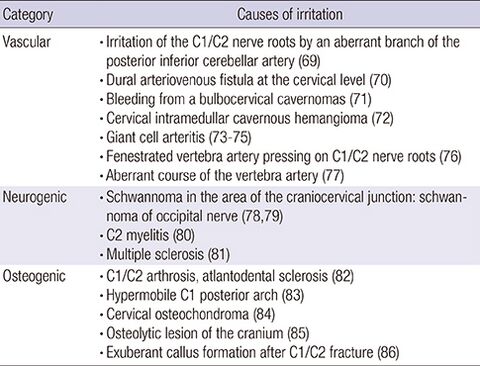
Compression of the LON can lead to occipital neuralgia. Occipital neuralgia (C2 neuralgia) presents with paroxysmal shooting/stabbing pain in the dermatomes of the occipital nerves<ref name=":3">Choi I, Jeon SR. [https://synapse.koreamed.org/articles/1023238 Neuralgias of the head: occipital neuralgia.] Journal of Korean Medical Science. 2016 Apr 1;31(4):479-88.</ref><ref name=":4">''13.4 occipital neuralgia'' (2018) ''ICHD''. International Headache Society. Available at: [https://ichd-3.org/13-painful-cranial-neuropathies-and-other-facial-pains/13-4-occipital-neuralgia/ https://ichd-3.org/13-painful-cranial-neuropathies-and-other-facial-pains/13-4-occipital-neuralgia]/ (Accessed: March 21, 2023).</ref>. The LON is involved in 10% of cases and GON is involved in 90% of cases<ref name=":3" />. Compression of the GON and/or LON can be due to various things. The table below summarises the possible etiologies: | |||
[[File:Occipital Nerve 1.jpg|thumb|480x480px|<ref>Choi I, Jeon SR. Neuralgias of the head: occipital neuralgia. Journal of Korean Medical Science. 2016 Apr 1;31(4):479-88.</ref>|alt=|none]] | |||
== Assessment == | == Assessment == | ||
According to the International Classification of Headache Disorder (ICHD-III), occipital neuralgia (ON) falls in to the Neuropathies & Facial Pains and other headaches category<ref name=":4" />. | |||
The <u>diagnostic criteria</u> for ON can be found [https://ichd-3.org/13-painful-cranial-neuropathies-and-other-facial-pains/13-4-occipital-neuralgia/ here] (International Classification of Headache Disorder (ICHD-III) website). | |||
<u>Physical examination</u><ref name=":3" /><u>:</u> | |||
* Tenderness with palpation along the LON. The tenderness is usually about 3 cm superomedially to the tip of the mastoid process. | |||
* Tinel's sign may be present over the nerve. | |||
* The "pillow sign" may be present. This sign occurs when the patient experiences pain when the patient hyperextends or rotates their neck while lying with their head on a pillow. | |||
<u>Other assessment methods</u><ref name=":3" />: | |||
* MRI is a helpful tool in diagnosing this disorder. | |||
* Local anaesthetic diagnostic block - diagnosis can be confirmed is there is temporary relief in symptoms together with the correct clinical picture. | |||
== Treatment == | == Treatment == | ||
There is no consensus on the ideal management of ON and there is rarity of well-designed studies<ref name=":3" />. Some treatment options are discussed below. | |||
=== Conservative management === | |||
# Physiotherapy<ref name=":3" /> | |||
#* Education, patient support, and reassurance | |||
#* Postural advice | |||
# Pharmacological<ref name=":3" /> | |||
#* Tricyclic antidepressants | |||
#* Serotonin selective reuptake inhibitors | |||
#* Anticonvulsants | |||
#* NSAIDs - transient effect | |||
== | === Interventional managament === | ||
# Local anesthetic agent injection with or without steroid<ref name=":3" /> | |||
# Botulinum toxin infiltrations<ref name=":3" /> | |||
# Pulsed radiofrequency treatment<ref name=":3" /> | |||
=== Surgery === | |||
# Neurolysis<ref name=":3" /> | |||
# Occipital nerve stimulation<ref name=":3" /> - electrodes are place subcutaneously in the C1 and C2 regions of the posterior spine | |||
== References == | == References == | ||
| Line 29: | Line 73: | ||
[[Category:Anatomy]] [[Category:Nerves]] | [[Category:Anatomy]] [[Category:Nerves]] | ||
Latest revision as of 10:46, 27 March 2023
Original Editor - Wendy Snyders
Top Contributors - Wendy Snyders, Kim Jackson and Dilawar Singh Maan
Description[edit | edit source]
The lesser occipital nerve (LON), together with the greater occipital nerve (GON) and third occipital nerve innervate the occipital scalp[1]. Its location is highly variable but it reliably emerges from the posterior border of the sternocleidomastoid muscle[2][3]. It then penetrates the deep cervical fascia and superior to the occiput, it communicates with the GON and innervates the skin[3]. The LON has been implicated in patients with occipital headaches[1][4].
Root[edit | edit source]
The root is the lateral branch of the dorsal rami of the C2 and/or C3 spinal nerves[1][2][3].
Branches[edit | edit source]
It has three branches[3]:
- auricular
- mastoid
- occipital
Function[edit | edit source]
Sensory[edit | edit source]
It provides the sensory innervation to the skin of the lateral neck, superior ear and postauricular skin[2].
Clinical relevance[edit | edit source]
Compression of the LON can lead to occipital neuralgia. Occipital neuralgia (C2 neuralgia) presents with paroxysmal shooting/stabbing pain in the dermatomes of the occipital nerves[6][7]. The LON is involved in 10% of cases and GON is involved in 90% of cases[6]. Compression of the GON and/or LON can be due to various things. The table below summarises the possible etiologies:
Assessment[edit | edit source]
According to the International Classification of Headache Disorder (ICHD-III), occipital neuralgia (ON) falls in to the Neuropathies & Facial Pains and other headaches category[7].
The diagnostic criteria for ON can be found here (International Classification of Headache Disorder (ICHD-III) website).
Physical examination[6]:
- Tenderness with palpation along the LON. The tenderness is usually about 3 cm superomedially to the tip of the mastoid process.
- Tinel's sign may be present over the nerve.
- The "pillow sign" may be present. This sign occurs when the patient experiences pain when the patient hyperextends or rotates their neck while lying with their head on a pillow.
Other assessment methods[6]:
- MRI is a helpful tool in diagnosing this disorder.
- Local anaesthetic diagnostic block - diagnosis can be confirmed is there is temporary relief in symptoms together with the correct clinical picture.
Treatment[edit | edit source]
There is no consensus on the ideal management of ON and there is rarity of well-designed studies[6]. Some treatment options are discussed below.
Conservative management[edit | edit source]
- Physiotherapy[6]
- Education, patient support, and reassurance
- Postural advice
- Pharmacological[6]
- Tricyclic antidepressants
- Serotonin selective reuptake inhibitors
- Anticonvulsants
- NSAIDs - transient effect
Interventional managament[edit | edit source]
- Local anesthetic agent injection with or without steroid[6]
- Botulinum toxin infiltrations[6]
- Pulsed radiofrequency treatment[6]
Surgery[edit | edit source]
- Neurolysis[6]
- Occipital nerve stimulation[6] - electrodes are place subcutaneously in the C1 and C2 regions of the posterior spine
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Lee M, Brown M, Chepla K, Okada H, Gatherwright J, Totonchi A, Alleyne B, Zwiebel S, Kurlander D, Guyuron B. An anatomical study of the lesser occipital nerve and its potential compression points: implications for surgical treatment of migraine headaches. Plastic and reconstructive surgery. 2013 Dec 1;132(6):1551-6.
- ↑ 2.0 2.1 2.2 Dash KS, Janis JE, Guyuron B. The lesser and third occipital nerves and migraine headaches. Plastic and reconstructive surgery. 2005 May 1;115(6):1752-8.
- ↑ 3.0 3.1 3.2 3.3 Yu M, Wang SM. Anatomy, Head and Neck, Occipital Nerves. [Updated 2022 Oct 31]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK542213/
- ↑ Peled ZM, Pietramaggiori G, Scherer S. Anatomic and compression topography of the lesser occipital nerve. Plastic and Reconstructive Surgery Global Open. 2016 Mar;4(3).
- ↑ Choi I, Jeon SR. Neuralgias of the head: occipital neuralgia. Journal of Korean Medical Science. 2016 Apr 1;31(4):479-88.
- ↑ 6.00 6.01 6.02 6.03 6.04 6.05 6.06 6.07 6.08 6.09 6.10 6.11 Choi I, Jeon SR. Neuralgias of the head: occipital neuralgia. Journal of Korean Medical Science. 2016 Apr 1;31(4):479-88.
- ↑ 7.0 7.1 13.4 occipital neuralgia (2018) ICHD. International Headache Society. Available at: https://ichd-3.org/13-painful-cranial-neuropathies-and-other-facial-pains/13-4-occipital-neuralgia/ (Accessed: March 21, 2023).
- ↑ Choi I, Jeon SR. Neuralgias of the head: occipital neuralgia. Journal of Korean Medical Science. 2016 Apr 1;31(4):479-88.