Introduction to Clubfoot: Difference between revisions
No edit summary |
No edit summary |
||
| Line 124: | Line 124: | ||
Many different treatment methodologies for clubfoot have been used but since the 1970’s the Ponseti Method of treatment has has grown in popularity and has completely replaced the previous methods of treating Clubfoot in many countries, which included a mix of surgical and conservative techniques. Ponseti Method consists of 2 equally important phases: the corrective phase and the maintenance phase. | Many different treatment methodologies for clubfoot have been used but since the 1970’s the Ponseti Method of treatment has has grown in popularity and has completely replaced the previous methods of treating Clubfoot in many countries, which included a mix of surgical and conservative techniques. Ponseti Method consists of 2 equally important phases: the corrective phase and the maintenance phase. | ||
{| class="wikitable" | {| class="wikitable" | ||
| | | colspan="2" |'''Ponseti Method Phases of Treatment''' | ||
|- | |||
|Corrective Phase | |Corrective Phase | ||
|During the corrective phase the position of the foot is gradually corrected using a series of manipulations and plaster of Paris casts, then finally a small outpatient procedure is performed to cut the Achilles tendon (tenotomy). The corrective phase usually takes 4–8 weeks and the baby is seen weekly for the treatment. | |During the corrective phase the position of the foot is gradually corrected using a series of manipulations and plaster of Paris casts, then finally a small outpatient procedure is performed to cut the Achilles tendon (tenotomy). The corrective phase usually takes 4–8 weeks and the baby is seen weekly for the treatment. | ||
| Line 145: | Line 146: | ||
The entire course of treatment can cost as little as US$150, which compared to many treatments for similar conditions is extremely economical. This is why many Ministries of Health, NGOs, and others see the value of providing Ponseti treatment as an early intervention in order to avoid preventable disability.<ref name=":0" /> | The entire course of treatment can cost as little as US$150, which compared to many treatments for similar conditions is extremely economical. This is why many Ministries of Health, NGOs, and others see the value of providing Ponseti treatment as an early intervention in order to avoid preventable disability.<ref name=":0" /> | ||
== References == | == References == | ||
<references /> <br> | <references /> <br> | ||
[[Category:Conditions]] [[Category:Foot]] [[Category:Clubfoot]] [[Category:Musculoskeletal/Orthopaedics]] | [[Category:Conditions]] [[Category:Foot]] [[Category:Clubfoot]] [[Category:Musculoskeletal/Orthopaedics]] | ||
Revision as of 18:38, 16 August 2017
Original Editor - Thomas Maeseele
Top Contributors - Naomi O'Reilly, Kudzanayi Ronald Muzenda, Kim Jackson, Rachael Lowe, Evan Thomas, Admin, Simisola Ajeyalemi, Robin Tacchetti, 127.0.0.1, Thomas Maeseele, Esraa Mohamed Abdullzaher, WikiSysop, Rucha Gadgil, Meaghan Rieke and Tony Lowe
Definition/Description[edit | edit source]
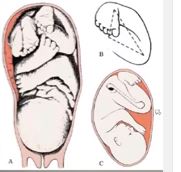
Clubfoot, also known as Congenital Talipes Equinovarus, is a congenital deformity of the foot, not an embryonic malformation, that left untreated can limit a person’s mobility by making it difficult and painful to walk. [1] It is defined as a deformity characterized by complex, malalignment of the foot involving soft and bony structures in the hindfoot, midfoot and forefoot [2] It is one of the most common serious congenital abnormalities to affect the foot. Most often it is an isolated abnormality, but occasionally it is associated with other congenital malformations or syndromes.
Talipes Equinovarus comes from the following: [3]
“Tali” means Ankle,
“Pes” means Foot
“Equinus” means foot pointing down (like a horse’s foot)
“Varus” means deviated towards midline
Global Burden of Disease[edit | edit source]
If Clubfoot is not treated or managed successfully, it can progress to a severe deformity causing lifelong impairment affecting participation in activities of daily living. As the child grows and puts weight on their feet they will bear weight through the sides, or even the tops of their feet. A large callus of thickened skin forms on the weight-bearing surface and the deformed position causes pain and leaves the feet open to injury and infection.
In an adult, this often means the individual is unable be able to wear normal footwear with most cases experiencing severe restriction in walking by the time they are in their 20's or 30's with visible deformity of the foot. This, in turn, often leads to discrimination and the inability to access education and employment, which further impacts the individual's capacity to contribute economically which may affect both the individual and their family members.
Epidemiology[edit | edit source]
Clubfoot is more common in males with a 2.5 to 2.8:1 Male:Female ratio.[4] Various incidences have been noted between countries and regions ranging from 1-1.50 per 1000 live births, rising up to 3 per 1000 live births.[4][5][6] Similarly, ethnic differences in occurrence have been reported with the lowest incidence (0.6%) among the Chinese Population, while the highest incidence (6.8%) in the Polynesian Region. The accumulative incidence is approximately 1 per 1000 live births among Caucasians.[7] Worldwide 80% of children born with clubfoot are in low-and middle-income countries. [3]
Etiology[edit | edit source]
The causes of Clubfoot are not clearly understood. In some countries and cultures there are different beliefs about what causes a child to be born with Clubfoot. These include include spiritual influences, spells, or curses often leading to mothers being blamed for the deformity. These ideas can cause the child with Clubfoot to be excluded from society, so therefore it is important to explain to families that children with Clubfoot are a valuable part of the community. [3]
Several theories have been proposed to explain the origin of Clubfoot, considering both intrinsic and extrinsic causes, including: intrauterine position of the fetus, mechanical compression or increased hydraulic pressure, interruption in fetal development, viral infections, vascular deficiencies, muscular alterations, neurological alterations, defect in the development of the bones structures and genetic defects.[2][8] Researchers believe there are both genetic and environmental influences.
Neurogenic Theory[edit | edit source]
Reduced motor unit, which counts in the distribution of the common peroneal nerve, may be responsible for clinically demonstrable muscle weakness.[7]
Myogenic Theory[edit | edit source]
Suggested by the presence of anomalous muscles, e.g. accessory soleus muscle and flexor digitorum accessorious longus muscles, which can produce equinovarus deformity.[7][8]
Vascular Theory[edit | edit source]
Diminution of blood flow in the anterior tibial artery and its derivatives.[7][8]
Embyonic Theory[edit | edit source]
Developmental defect occurring up to 12 weeks of intrauterine life.[8]
Chromosonal Theory[edit | edit source]
Presence of some chromosonal defects in unfertilized germ cells.[7][8]
Osteogenic Theory[edit | edit source]
Due to some unknown cause, temporary arrest of development occurs in the 7- to 8- week-old embryo, which can lead to clubfoot or other deformities.[7][8]
Mechanical Block Theory[edit | edit source]
Due to some mechanical obstruction during the intrauterine development period, e.g. intrauterine fibrotic bands, less amniotic fluid, disproportionate uterine cavity, etc, talipes equinovarus can occur.[8]
Clinically Relevant Anatomy & Clinical Presentation[edit | edit source]
The foot consists of 26 bones. Most relevant for this congenital deformity are the Talus, Calcaneus and Navicular. The underlying deformity of clubfoot can be most easily understood if it is divided into four components, whose first letters make up the word CAVE. These components are: Cavus, Adductus, Varus, and Equinus. The Cavus and Adductus deformities occur in the midfoot, while the Varus and Equinus deformities occur in the hindfoot.[3]
Cavus in the midfoot is the first part of the deformity of clubfoot. The arch of the foot is higher than normal.as a result of the first metatarsal being plantarflexed in relation to the calcaneum and hindfoot. [3]
Adductus is movement towards the midline. Adductus is the second part of the clubfoot deformity. The forefoot is adducted towards the midline. This is the second part of the deformity of clubfoot. The navicular moves medially and starts to dislocate off the talus. The calcaneum also rotates medially under the talus as part of the adductus deformity.[3]
Varus means movement towards the midline. Varus of the hindfoot is the third part of the deformity of clubfoot. The heel is in varus in relation to the tibia.[3]
Equinus means an increase in the plantarflexion of the foot. The entire foot points downwards in relation to the tibia. Equinus of the hindfoot is therefore the fourth part of the clubfoot deformity.[3]
The deformity consists of equinus/plantarflexion at the ankle combined with adduction and inversion at the subtalar, midtarsal and anterior tarsal joints[9]. Clubfoot can be described as “congenital dislocation of the Talo-Calcaneal-Navicular (TCN) Joint” [10]. The navicular moves medially on the talus in clubfoot while the calcaneum rotates under the talus in clubfoot
The foot is held in adduction and inversion by ligaments and muscles. Muscles that are contracted are triceps surae, tibialis posterior, flexor digitorum longus and flexor hallucis longus. Further there is an imbalance between the inverter-plantarflexor muscles and the everter-dorsiflexor muscles. The calf and peroneal muscles are usually poorly developed.[9] Weak peroneal muscles allow the foot to be inverted. The ligaments of the posterior and medial aspect of the ankle are thick and taut.[11].
Classification[edit | edit source]
Not all Clubfeet are the same and it is important that all people treating Clubfoot use the same terms to describe the different types. Each type of clubfoot has unique characteristics and may need specific treatment. Early recognition of the type of clubfoot one is dealing with can help guide appropriate treatment. Although there is no universal classification system for clubfoot, clubfoot can be classified according to the nature of the deformity: [12]
Idiopathic Clubfoot[edit | edit source]
Most commonly, Clubfoot is classified as “Idiopathic Clubfoot” meaning there is no known cause for the deformity. In Idiopathic Clubfoot, there can also be a definite hereditary influence, in that if a person has a relative, parent, or sibling has Clubfoot, then they are more likely to have Clubfoot or have a child with it (3-10% chance). Within the group of Idiopathic Clubfeet there is a wide spectrum of impairment depending on severity, as well as whether the Clubfoot has been untreated, partially treated, poorly treated, or successfully treated.[3]
Untreated Clubfoot[edit | edit source]
All clubfeet from birth up to 2 years of age that have had very little or no treatment can be considered as untreated clubfeet.[3]
If clubfoot is not treated successfully, it can progress to a severe deformity causing lifelong disability.As the child grows and puts weight on their feet they will bear weight through the sides, or even the tops of their feet. A large callus of thickened skin forms on the weight-bearing surface and the deformed position causes pain and leaves the feet open to injury and infection. The person will not be able to wear normal footwear and in most cases will experience severe difficulty in walking by the time they are in their 20s or 30s. Having such a visible deformity can cause people with clubfoot to be discriminated against, and they may not be able to access education and employment. As well as being very difficult for the individual and their family, this has an effect on society as a whole, as it means that people born with clubfoot may not be able to work and contribute economically. [3]
Treated Clubfoot[edit | edit source]
Untreated clubfeet that have been corrected with Ponseti treatment are termed “treated clubfeet”. Treated clubfeet are usually braced full-time for 3 months and at night up to age 4 or 5 years.[3]
Recurrent Clubfoot[edit | edit source]
This is a Clubfoot which has achieved a good result with Ponseti treatment, but the deformity has recurred. Recurrence means the reappearance of any or all of the components of the original clubfoot deformity after successful treatment. It is common in the first and second years after treatment especially if bracing has not been continued, but can happen at any time until skeletal maturity is reached. The most common reason is due to abandoning the braces early. [3]
Neglected Clubfoot[edit | edit source]
The Neglected Clubfoot is in a child older than 2 years, where little or no treatment has been performed. The Neglected Clubfoot may respond to Ponseti Treatment, but also may have bony deformity that requires surgical correction.[3]
Complex Clubfoot[edit | edit source]
Any foot with deformity that has received any type of treatment other than the Ponseti method may have added complexity because of additional pathology or scarring from surgery.[3]
Resistant Clubfoot[edit | edit source]
This is a Clubfoot where Ponseti Treatment has been correctly performed but there has been no significant improvement. It is often found that this type of Clubfoot is not in fact idiopathic after all and is secondary or syndromic.[3]
Atypical Clubfoot[edit | edit source]
This is a Clubfoot which involves a foot that is often swollen, has a plantar flexed first metatarsal and an extended big toe. Some children are born with atypical clubfoot, but we believe others become atypical because of poor treatment, most often occurring as a result of slippage of a cast.[3]
Secondary Clubfoot[edit | edit source]
Secondary Clubfoot, on the other hand, occurs when there is another disease or condition that is causing or linked to the development of Clubfoot. Such conditions are usually Neurological such as Spina Bifida associated with concurrent sensory and or motor impairments or Syndromic Disorders such as Arthrogryposis associated with more global findings and involvement of other musculoskeletal issues.
Spina Bifida[edit | edit source]
A congenital, neurological condition where there is failure of the formation of the bone or skin or both to cover the lower end of the spinal cord and nerves. It is often associated with neurological problems in the legs, and clubfoot. If cases present to the clubfoot clinic it is important to find out what the long-term prognosis is, and whether the child is likely to walk. If the child is likely to survive and walk then it is worth trying Ponseti Clubfoot Treatment. The success rate with simple manipulation is not high and surgery may be considered. Even if the child has a low likelihood of walking the parents might still like to try to get the feet corrected so that shoes can be worn.[13]
Arthrogryposis[edit | edit source]
A congenital condition where the child is born with a number of deformities of the joints. A severe case can have stiffness of the elbows, wrists, hips, knees, and feet. People with severe cases are often unable to walk. Clubfoot is a relatively common association. Ponseti treatment can be tried and is often partially successful.[13]
Amniotic Band Syndrome[edit | edit source]
The cause of amniotic band syndrome is not fully clear, but children with this condition are born with tight skin and soft tissue bands around their limbs, constricting blood and lymph flow and causing swelling. Some cases are associated with clubfoot although in the one illustrated here it is only mild. Treatment of the tight band often involves surgery. If there is a clubfoot associated, then Ponseti treatment should only be done with extreme care as blood supply to the foot can be affected and there is a risk of gangrene. These cases are best referred to a centre with surgical experience.[13]
Tibial Agenesis[edit | edit source]
Failure in the formation of the tibia. There is a spectrum of presentations from complete absence to a slightly short tibia. In this case there is only a very short tibia and the foot therefore adopts a varus deformity pointing to the midline. This is not a clubfoot deformity even though there is a similarity in the appearance. If there is doubt about the diagnosis, an X-ray should be taken. Treatment is very complicated and many surgeons recommend an amputation with below-knee prosthesis. There is little benefit in starting clubfoot treatment.[13]
Positional Clubfoot[edit | edit source]
Positional Clubfoot refers to a flexible foot that was held over time in an abnormal position in utero. When the child is born, due to the prolonged positioning, they may present with one or both feet in an atypical resting position. Children with Positional Clubfoot typically exhibit unrestricted passive range of motion of forefoot and ankle. The foot at the time of birth has some deformity but bony alignment is not impacted and foot position is likely corrected through conservative treatment involving a comprehensive program of stretching, range of motion, and weight bearing. In a small number of cases post conservative treatment the foot needs 1 or 2 Casts to ensure they are maintained in a corrected position although in the majority of cases these feet usually correct well and do not lead to any long lasting, significant impairment.[3] [14]
Diagnosis[edit | edit source]
Talipes Equinovarus is usually detected at birth. The examination after birth consists of taking the foot and manipulate it gently to see if it can be brought into normal position. If this examination is positive the condition is considered to be correctable[15]
Prognosis[edit | edit source]
The prognosis depends mostly on the time the treatment started. When treatment is started within the first week after birth, the chances of healing without relapse in further life are high. Persistence in wearing the abduction bar also contributes to a good prognosis .[9]
Outcome Measures[edit | edit source]
The most common used outcome measure is the scoring system of Pirani. This scoring system assesses the severity of clubfoot deformity and response to treatment[16]. It has a predictive value concerning the number of casts needed to correct the foot. A high score, 4 or more, predicts the use of at least 4 casts. A score less than 4 predicts the need of 3 or fewer casts. Each component is scored as 0 (normal), 0.5 (mildly abnormal) or 1 (severely abnormal) [11]
Treatment[edit | edit source]
Many different treatment methodologies for clubfoot have been used but since the 1970’s the Ponseti Method of treatment has has grown in popularity and has completely replaced the previous methods of treating Clubfoot in many countries, which included a mix of surgical and conservative techniques. Ponseti Method consists of 2 equally important phases: the corrective phase and the maintenance phase.
| Ponseti Method Phases of Treatment | |
| Corrective Phase | During the corrective phase the position of the foot is gradually corrected using a series of manipulations and plaster of Paris casts, then finally a small outpatient procedure is performed to cut the Achilles tendon (tenotomy). The corrective phase usually takes 4–8 weeks and the baby is seen weekly for the treatment. |
| Maintenance Phase | Once the corrective phase has achieved a good position for the foot, the treatment is not over as the foot will tend to return to its deformed position, so the aim of the maintenance phase involves keeping the corrected position for the next 4–5 years. This is achieved by putting the child’s feet into a brace for:
|
The Ponseti Method is a simple, cost-effective treatment that has become widely used around the world. Numerous research studies in countries across the globe in the last 20 years have shown that in more than 90% of cases of newborn children with idiopathic clubfoot it be treated effectively with the Ponseti technique. The Ponseti Method’s efficacy is backed up by a large and growing body of evidence, and has now become the treatment of choice for Clubfoot. [4][5][6][11][16][17]
The goals of treatment are:
· To have functional, pain-free feet
· To wear normal shoes
· To avoid permanent disability
The entire course of treatment can cost as little as US$150, which compared to many treatments for similar conditions is extremely economical. This is why many Ministries of Health, NGOs, and others see the value of providing Ponseti treatment as an early intervention in order to avoid preventable disability.[3]
References[edit | edit source]
- ↑ Amanda Marie De Hoedt, Clubfoot Image Classification, University of Iowa, Iowa Research Online, 2013 [Available from Iowa Research Online /ir.uiowa.edu/etd/4836 http://ir.uiowa.edu/etd/4836]
- ↑ 2.0 2.1 Daniel Augusto Carvalho Maranho, Jose Batista Volpon, Congenital Clubfoot , 2011;19(3):163-9.
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 3.13 3.14 3.15 3.16 3.17 3.18 Africa Clubfoot Training Project. Chapter 2 Africa Clubfoot Training Basic & Advanced Clubfoot Treatment Provider Courses - Participant Manual. University of Oxford: Africa Clubfoot Training Project, 2017.
- ↑ 4.0 4.1 4.2 Boden, R.A., Nuttall, G.H., & Paton, R.W. (2011). A 14-year longitudinal comparison study of two treatment methods in clubfoot: Ponseti versus traditional. Acta Orhopaedica Belgica, 77(4), pp. 522-528.
- ↑ 5.0 5.1 Harnett, P., Freeman, R., Harrison, W.J., Brown, L.C., ; Beckles, V. (2011). An accelerated Ponseti versus the standard Ponseti method. The Journal of Bone ; Joint Surgery, 93, pp. 404-408.
- ↑ 6.0 6.1 Jowett, C.R., Morcuende, J.A., ; Ramachandran, M. (2011). Management of congenital talipes equinovarus using the Ponseti method. The Journal of Bone & Joint Surgery, 93, pp. 1160-1164.
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 Henrik M. Wallander, Congenital Clubfoot (Aspects on Epidemiology, Residual Deformity and Patient Reported Outcome), ACTA University, 2009.
- ↑ 8.0 8.1 8.2 8.3 8.4 8.5 8.6 Pandey, S., & Pandey, A.K. (2003). The classification of clubfoot a practical approach. The Foot, 13, pp. 61-65.
- ↑ 9.0 9.1 9.2 Adams, J.C., & Hablen, D.L. (2001). Outline of Orthopaedics. London: Churchill Livingstone.
- ↑ Anand, A., & Sala, D.A. (2008). Clubfoot: Etiology and treatment. Indian Journal of Orthopaedics, 42(1), pp. 22-28.
- ↑ 11.0 11.1 11.2 Staheli, L. (2009). Clubfoot: Ponseti Management Third Editon. Seattle: Global Help.
- ↑ Clubfoot,http://emedicine.medscape.com/article/1237077-overview#a4 (accessed 28 June 2017)
- ↑ 13.0 13.1 13.2 13.3 Africa Clubfoot Training Project. Chapter 15 Africa Clubfoot Training Basic & Advanced Clubfoot Treatment Provider Courses - Participant Manual. University of Oxford: Africa Clubfoot Training Project, 2017.
- ↑ Africa Clubfoot Training Project. Chapter 1 Africa Clubfoot Training Basic & Advanced Clubfoot Treatment Provider Courses - Participant Manual. University of Oxford: Africa Clubfoot Training Project, 2017.
- ↑ Goldie, B.S. (1992). Orthopaedic Diagnosis and Management. A guide to the care of orthopaedic patients. Oxford: Blackwell Scientific Publications.
- ↑ 16.0 16.1 Docker, C.E.J., Lewthwaite, S., & Kiely, N.T. (2007). Ponseti treatment in the management of clubfoot deformity – a continuing role for paediatric orthopaedic services in secondary care centres. The Royal College of Surgeons of England, 89, pp. 510-512.
- ↑ Suzann, K.C., Vander Linden, D.W., & Plisano, R.J. (2005). Physical Therapy for Children. Missouri: Elsevier.