Hypercalcemia: Difference between revisions
No edit summary |
mNo edit summary |
||
| Line 6: | Line 6: | ||
== Definition/Description<br> == | == Definition/Description<br> == | ||
Hypercalcemia is characterized by elevated calcium levels in the blood. It may include symptoms associated with the musculoskeletal, neurological, cardiovascular, and gastrointestinal<sup></sup><sup></sup><sup></sup> systems. Hypercalcemia is often a sign or symptom of other disease occurring within the body. Normal calcium levels range from 8.2-10.2 mg/dL. Mild hypercalcemia occurs when this level raises to 12mg/dL and severe hypercalcemia is classified as serum calcium at 14mg/dL.<ref name=" | Hypercalcemia is characterized by elevated calcium levels in the blood. It may include symptoms associated with the musculoskeletal, neurological, cardiovascular, and gastrointestinal<sup></sup><sup></sup><sup></sup> systems. Hypercalcemia is often a sign or symptom of other disease occurring within the body. Normal calcium levels range from 8.2-10.2 mg/dL. Mild hypercalcemia occurs when this level raises to 12mg/dL and severe hypercalcemia is classified as serum calcium at 14mg/dL.<ref name="p1">Goodman CC, Snyder TEK. Differential Diagnosis for Physical Therapists: Screening for Referral. 5th ed. St. Louis, MO: Elsevier Saunders; 2013.</ref> | ||
== Prevalence == | == Prevalence == | ||
Hypercalcemia is a common medical emergency and between 20-40% of patients suffering from cancer can develop this during the course of their disease. It is considered the most common serious electrolyte presenting in adults with malignancies. This disorder often occurs in cases of metastatic bone disease with osteolytic lesion, breast cancer and myeloma. This is related to an increase in bone resorption caused by tumor cell production of parathyroid hormone-related protein that stimulates osteoclasts. It is also associated with primary hyperparathyroidism which occurs in 25 per 100,000 individuals and 75 per 100,000 hospitalized patients. This condition is the most common cause of mild hypercalcemia and can be treated through outpatient care. More than 50,000 cases occur in the U.S. each year.<span style="font-size: 11px;"> <ref name=" | Hypercalcemia is a common medical emergency and between 20-40% of patients suffering from cancer can develop this during the course of their disease. It is considered the most common serious electrolyte presenting in adults with malignancies. This disorder often occurs in cases of metastatic bone disease with osteolytic lesion, breast cancer and myeloma. This is related to an increase in bone resorption caused by tumor cell production of parathyroid hormone-related protein that stimulates osteoclasts. It is also associated with primary hyperparathyroidism which occurs in 25 per 100,000 individuals and 75 per 100,000 hospitalized patients. This condition is the most common cause of mild hypercalcemia and can be treated through outpatient care. More than 50,000 cases occur in the U.S. each year.<span style="font-size: 11px;"> <ref name="p2">Hypercalcemia in Emergency Medicine [Internet]. Medscape. 2010 [updated 2010 Sep 1]. Available from:fckLRfckLRhttp://emedicine.medscape.com/article/766373-overview#a0199</ref></span><br> | ||
<br> | <br> | ||
The incidence of hyperparathyroidism is considerably higher in women, thus suggesting women are at greater risk of developing hypercalcemia. The annual incidence in women older than 65 years is 250 per 100,000, although elevations in calcium levels related to cancer have no sex predominance. Also, with an increase in age, the incidence of hyperparathyroidism rises just as the rate of malignancy and the malignancy-associated hypercalcemia increases as well.<ref name=" | The incidence of hyperparathyroidism is considerably higher in women, thus suggesting women are at greater risk of developing hypercalcemia. The annual incidence in women older than 65 years is 250 per 100,000, although elevations in calcium levels related to cancer have no sex predominance. Also, with an increase in age, the incidence of hyperparathyroidism rises just as the rate of malignancy and the malignancy-associated hypercalcemia increases as well.<ref name="p2" /> | ||
== Characteristics/Clinical Presentation<br> == | == Characteristics/Clinical Presentation<br> == | ||
| Line 73: | Line 73: | ||
|} | |} | ||
<ref name=" | <ref name="p1" /><br> | ||
== Associated Co-morbidities == | == Associated Co-morbidities == | ||
Hypercalcemia can lead to many other complications such as:<ref name=" | Hypercalcemia can lead to many other complications such as:<ref name="p3">Hypercalcemia [Internet]. MayoClinic. 2012 [updated 2012 Aug 10]. Available from:fckLRfckLRhttp://www.mayoclinic.com/health/hypercalcemia/DS00976/DSECTION=causes</ref><br> | ||
*'''Osteoporosis''': if the bones continue to release calcium into the blood, it could lead to this disease. | *'''Osteoporosis''': if the bones continue to release calcium into the blood, it could lead to this disease. | ||
| Line 92: | Line 92: | ||
{| width="90%" border="1" cellpadding="1" cellspacing="1" | {| width="90%" border="1" cellpadding="1" cellspacing="1" | ||
|- | |- | ||
| Medication<ref name=" | | Medication<ref name="p4">Hypercalcemia Treatments and Drugs [Internet]. MayoClinic. 2012 [updated 2012 Aug 10]. Available from:fckLRfckLRhttp://www.mayoclinic.com/health/hypercalcemia/DS00976/DSECTION=treatments%2Dand%2Ddrugs</ref> | ||
| Treatment Effect | | Treatment Effect | ||
| Side Effects | | Side Effects | ||
| Line 98: | Line 98: | ||
| Loop Diuretics (ex; furosemide) | | Loop Diuretics (ex; furosemide) | ||
| Flushes out excess calcium from system | | Flushes out excess calcium from system | ||
| Frequent urination, arrythmias, electrolyte imbalances, dizziness, muscle cramps/weakness, extreme fatigue, blurred vision, confusion, headache, dehydration, fever, sore throat, cough, skin rash, loss of appetite, nausea, vomiting<ref name=" | | Frequent urination, arrythmias, electrolyte imbalances, dizziness, muscle cramps/weakness, extreme fatigue, blurred vision, confusion, headache, dehydration, fever, sore throat, cough, skin rash, loss of appetite, nausea, vomiting<ref name="p6">Diuretics and High Blood Pressure: Uses, Side Effects, and More [Internet]. WebMD 2013. Available from:fckLRfckLRhttp://www.webmd.com/hypertension-high-blood-pressure/guide/diuretic-treatment</ref> | ||
|- | |- | ||
| Intravenous Biphosphonates | | Intravenous Biphosphonates | ||
| Prevent bone breakdown, reduce bone pain, reduce the number of pathologic fractures | | Prevent bone breakdown, reduce bone pain, reduce the number of pathologic fractures | ||
| Heartburn, headache, constipation, diarrhea, muscle and joint pain<ref name=" | | Heartburn, headache, constipation, diarrhea, muscle and joint pain<ref name="p7">Biphosphonates Uses, Side Effects, Types, Effectiveness [Internet]. WebMD. 2013. Available from:fckLRfckLRhttp://www.webmd.com/osteoporosis/bisphosphonates-for-osteoporosis</ref> | ||
|- | |- | ||
| Calcitonin | | Calcitonin | ||
| Reduce bone reabsorption and slow bone loss | | Reduce bone reabsorption and slow bone loss | ||
| Warmth/redness of the skin, itching of the skin, nausea, loss of appetite, stomach pain, vomiting, skin rash, increased urination, eye pain, swelling in the feet, swelling or irritation at injection site (if injection was given)<ref name=" | | Warmth/redness of the skin, itching of the skin, nausea, loss of appetite, stomach pain, vomiting, skin rash, increased urination, eye pain, swelling in the feet, swelling or irritation at injection site (if injection was given)<ref name="p8">Calcitonin Side Effects [Internet]. Drugs.com. 2013. Available from:fckLRfckLRhttp://www.drugs.com/sfx/calcitonin-side-effects.html</ref> | ||
|- | |- | ||
| Glucocorticoids | | Glucocorticoids | ||
| Help to counter the effect of excess Vitamin D | | Help to counter the effect of excess Vitamin D | ||
| Elevated pressure in the eyes, fluid retention that may cause swelling in the legs, increased blood pressure, mood swings, weight gain<ref name=" | | Elevated pressure in the eyes, fluid retention that may cause swelling in the legs, increased blood pressure, mood swings, weight gain<ref name="p9">Prednisone and other corticosteroids: Balance the risks and benefits [Internet]. MayoClinic. 2012 [updated 2012 Aug 10]. Available from:fckLRfckLRwww.mayoclinic.com/health/steroids/HQ01431</ref> | ||
|- | |- | ||
| Hemodialysis | | Hemodialysis | ||
| Remove excess waste and calcium from the bloodstream | | Remove excess waste and calcium from the bloodstream | ||
| Hypotension, muscle cramps, itching, difficulty sleeping, anemia, pericarditis, hyperkalemia, infection, depression<ref name=" | | Hypotension, muscle cramps, itching, difficulty sleeping, anemia, pericarditis, hyperkalemia, infection, depression<ref name="p0">Hemodialysis: Risks [Internet]. MayoClinic. 2012 [updated 2012 Aug 10]. Available from:fckLRfckLRhttp://www.mayoclinic.com/health/hemodialysis/MY00281/DSECTION=risks</ref> | ||
|} | |} | ||
| Line 121: | Line 121: | ||
== Diagnostic Tests/Lab Tests/Lab Values == | == Diagnostic Tests/Lab Tests/Lab Values == | ||
Hypercalcemia is diagnosed by blood tests revealing increased serum calcium levels. However, other tests may need to be done in order to determine the underlying cause of hypercalcemia. These may include: <ref name=" | Hypercalcemia is diagnosed by blood tests revealing increased serum calcium levels. However, other tests may need to be done in order to determine the underlying cause of hypercalcemia. These may include: <ref name="p3" /> | ||
*Chest X-Ray | *Chest X-Ray | ||
| Line 128: | Line 128: | ||
*Mammogram | *Mammogram | ||
These tests may help determine whether you have lung cancer, breast cancer, other malignancies, or sarcoidosis (a granulomatous disease of the lungs). <ref name=" | These tests may help determine whether you have lung cancer, breast cancer, other malignancies, or sarcoidosis (a granulomatous disease of the lungs). <ref name="p3" />[[Image:TH 2011 01 pp13 t01 LG-1.jpg]] | ||
http://www.the-hospitalist.org/SpringboardWebApp/userfiles/hosp/image | http://www.the-hospitalist.org/SpringboardWebApp/userfiles/hosp/image | ||
| Line 134: | Line 134: | ||
== Etiology/Causes == | == Etiology/Causes == | ||
Common causes of hypercalcemia include: <ref name=" | Common causes of hypercalcemia include: <ref name="p5">Hypercalcemia: Causes [Internet]. MayoClinic. 2012 [updated 2012 Aug 10]. Available from:fckLRfckLRhttp://www.mayoclinic.com/health/hypercalcemia/DS00976/DSECTION=treatments%2Dand%2Ddrugs</ref> | ||
*'''Overactivity''' of parathyroid glands | *'''Overactivity''' of parathyroid glands | ||
| Line 145: | Line 145: | ||
== Systemic Involvement == | == Systemic Involvement == | ||
As stated in the chart above, hypercalcemia can present with symptoms in multiple systems. Usually, the first signs and symptoms are noticed in the nervous/musculoskeletal system causing some kind of muscle pain, weakness, and/or dysfunction. However, each patient will present differently depending on the severity and organ system involved. <ref name=" | As stated in the chart above, hypercalcemia can present with symptoms in multiple systems. Usually, the first signs and symptoms are noticed in the nervous/musculoskeletal system causing some kind of muscle pain, weakness, and/or dysfunction. However, each patient will present differently depending on the severity and organ system involved. <ref name="p1" /> | ||
The primary systems effects and the mechanisms of involvement are described below:<br> | The primary systems effects and the mechanisms of involvement are described below:<br> | ||
'''Neurological<ref name=" | '''Neurological<ref name="p2" />''' | ||
*Increased calcium levels decrease neuromuscular excitability, which leads to hypotonicity in smooth and striated muscle. | *Increased calcium levels decrease neuromuscular excitability, which leads to hypotonicity in smooth and striated muscle. | ||
| Line 157: | Line 157: | ||
*Has been documented to increase cerebrospinal fluid protein, which may be associated with headache | *Has been documented to increase cerebrospinal fluid protein, which may be associated with headache | ||
'''Cardiovascular<ref name=" | '''Cardiovascular<ref name="p2" />''' | ||
*Associated with increased myocardial contractility and irritability. | *Associated with increased myocardial contractility and irritability. | ||
| Line 163: | Line 163: | ||
*Incomplete or complete atrioventricular block may develop and progress to complete heart block, a systole, and/or cardiac arrest. | *Incomplete or complete atrioventricular block may develop and progress to complete heart block, a systole, and/or cardiac arrest. | ||
'''Gastrointestinal<ref name=" | '''Gastrointestinal<ref name="p2" />''' | ||
*Symptoms related to the depressive action of hypercalcemia on the autonomic nervous system, resulting smooth-muscle hypotonicity. | *Symptoms related to the depressive action of hypercalcemia on the autonomic nervous system, resulting smooth-muscle hypotonicity. | ||
| Line 171: | Line 171: | ||
*Abdominal pain may progress to obstipation (can be confused with acute abdominal obstruction). | *Abdominal pain may progress to obstipation (can be confused with acute abdominal obstruction). | ||
'''Renal<ref name=" | '''Renal<ref name="p2" />''' | ||
*Loss of urinary concentrating ability and polyuria due to tubular defect in the kidney. | *Loss of urinary concentrating ability and polyuria due to tubular defect in the kidney. | ||
| Line 178: | Line 178: | ||
*Renal insufficiency may occur as a result of diminished glomerular filtration. | *Renal insufficiency may occur as a result of diminished glomerular filtration. | ||
'''Musculoskeletal<ref name=" | '''Musculoskeletal<ref name="p2" />''' | ||
*Hypercalcemia of malignancy ([[Multiple Myeloma|multiple myeloma]]) can result from osteolytic metastases or humerally mediated bone resorption. | *Hypercalcemia of malignancy ([[Multiple Myeloma|multiple myeloma]]) can result from osteolytic metastases or humerally mediated bone resorption. | ||
| Line 185: | Line 185: | ||
== Medical Management (current best evidence) == | == Medical Management (current best evidence) == | ||
'''Mild Hypercalcemia '''(defined as corrected total serum calcium level lower than 12 mg/dL (<6 mEq/L or 3.0 mmol/L)<ref name=" | '''Mild Hypercalcemia '''(defined as corrected total serum calcium level lower than 12 mg/dL (<6 mEq/L or 3.0 mmol/L)<ref name="p2">Hypercalcemia(PDQ)[Internet]. National Cancer Institute.[updated 2013 Jan 9]Available from:fckLRfckLRhttp://www.cancer.gov/cancertopics/pdq/supportivecare/hypercalcemia/HealthProfessional/page1/AllPages</ref> | ||
*Hydration (IV fluids) followed by observation; this option should be considered for asymptomatic patients who are about to be treated for tumors that are likely to respond to antineoplastic treatment (ex: lymphoma, breast cancer, ovarian cancer, head and neck carcinoma, and multiple myeloma). | *Hydration (IV fluids) followed by observation; this option should be considered for asymptomatic patients who are about to be treated for tumors that are likely to respond to antineoplastic treatment (ex: lymphoma, breast cancer, ovarian cancer, head and neck carcinoma, and multiple myeloma). | ||
| Line 191: | Line 191: | ||
*Minimal use of sedating medications. | *Minimal use of sedating medications. | ||
<br> '''Moderate to Severe Hypercalcemia''' (defined as corrected total serum calcium equal to 12 to 14 mg/dL (6–7 mEq/L or 3.0–3.5 mmol/L)<ref name=" | <br> '''Moderate to Severe Hypercalcemia''' (defined as corrected total serum calcium equal to 12 to 14 mg/dL (6–7 mEq/L or 3.0–3.5 mmol/L)<ref name="p2" /> | ||
*Rehydration is the essential first step replenishing extracellular fluid, restoring intravascular volume, and saline diuresis | *Rehydration is the essential first step replenishing extracellular fluid, restoring intravascular volume, and saline diuresis | ||
| Line 200: | Line 200: | ||
'''Prevention''' | '''Prevention''' | ||
Preventive measures include:<ref name=" | Preventive measures include:<ref name="p2" /> | ||
*Ensuring adequate fluid intake of 3 to 4 L (100–140 fl oz per day if not contraindicated) | *Ensuring adequate fluid intake of 3 to 4 L (100–140 fl oz per day if not contraindicated) | ||
| Line 218: | Line 218: | ||
*Patient and Family Education | *Patient and Family Education | ||
<ref name=" | <ref name="p2" /> | ||
== Alternative/Holistic Management (current best evidence) == | == Alternative/Holistic Management (current best evidence) == | ||
| Line 228: | Line 228: | ||
*Probiotics | *Probiotics | ||
<ref name=" | <ref name="p1">Hypercalcemia, causes, symptoms, remedies [Internet]. Growyouthful.com. 2013. Available from:fckLRfckLRhttp://growyouthful.com/ailment/hypercalcemia-high-calcium.php</ref> | ||
== Differential Diagnosis == | == Differential Diagnosis == | ||
Evaluation of a patient should include: history, physical examination focusing on clinical manifestations of hypercalcemia, risk factors for malignancy, causative medications, and a family history of hypercalcemia-associated conditions to help clinically determine effectively and accurately a differential diagnosis. <ref name=" | Evaluation of a patient should include: history, physical examination focusing on clinical manifestations of hypercalcemia, risk factors for malignancy, causative medications, and a family history of hypercalcemia-associated conditions to help clinically determine effectively and accurately a differential diagnosis. <ref name="p3">A Practical Approach to Hypercalcemia [Internet]. Am Fam Physician. 2003 May 1;67(9):1959-1966. Available from:fckLRfckLRhttp://www.aafp.org/afp/2003/0501/p1959.html</ref> | ||
*Hyperparathyroidism | *Hyperparathyroidism | ||
| Line 244: | Line 244: | ||
'''Prognosis''': | '''Prognosis''': | ||
The prognosis of patients with hypercalcemia depends upon the etiology of the elevation:<ref name=" | The prognosis of patients with hypercalcemia depends upon the etiology of the elevation:<ref name="p2" /> | ||
*Prognosis is very poor with malignancy that has progressed into development of hypercalcemia. | *Prognosis is very poor with malignancy that has progressed into development of hypercalcemia. | ||
Revision as of 12:44, 6 June 2017
Original Editors - Whitney Browning & Natalie Elliott from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Whitney Browning, Natalie Elliott, Elaine Lonnemann, Admin, Lucinda hampton, 127.0.0.1, WikiSysop and Kim Jackson
Definition/Description
[edit | edit source]
Hypercalcemia is characterized by elevated calcium levels in the blood. It may include symptoms associated with the musculoskeletal, neurological, cardiovascular, and gastrointestinal systems. Hypercalcemia is often a sign or symptom of other disease occurring within the body. Normal calcium levels range from 8.2-10.2 mg/dL. Mild hypercalcemia occurs when this level raises to 12mg/dL and severe hypercalcemia is classified as serum calcium at 14mg/dL.[1]
Prevalence[edit | edit source]
Hypercalcemia is a common medical emergency and between 20-40% of patients suffering from cancer can develop this during the course of their disease. It is considered the most common serious electrolyte presenting in adults with malignancies. This disorder often occurs in cases of metastatic bone disease with osteolytic lesion, breast cancer and myeloma. This is related to an increase in bone resorption caused by tumor cell production of parathyroid hormone-related protein that stimulates osteoclasts. It is also associated with primary hyperparathyroidism which occurs in 25 per 100,000 individuals and 75 per 100,000 hospitalized patients. This condition is the most common cause of mild hypercalcemia and can be treated through outpatient care. More than 50,000 cases occur in the U.S. each year. [2]
The incidence of hyperparathyroidism is considerably higher in women, thus suggesting women are at greater risk of developing hypercalcemia. The annual incidence in women older than 65 years is 250 per 100,000, although elevations in calcium levels related to cancer have no sex predominance. Also, with an increase in age, the incidence of hyperparathyroidism rises just as the rate of malignancy and the malignancy-associated hypercalcemia increases as well.[2]
Characteristics/Clinical Presentation
[edit | edit source]
| System | Signs/symptoms |
|
Musculoskeletal |
|
| Central Nervous System |
|
|
Gastrointenstinal
|
|
| Cardiovascular |
|
Associated Co-morbidities[edit | edit source]
Hypercalcemia can lead to many other complications such as:[3]
- Osteoporosis: if the bones continue to release calcium into the blood, it could lead to this disease.
- Kidney stones: this could be caused by too much calcium accumulation in the urine, leading to crystal formation in the kidneys.
- Kidney failure: Severe hypercalcemia can lead to damage in the kidneys and possibly cause permanent loss of kidney function.
- Nervous system deficits: Severe hypercalcemia can lead to dementia and confusion.
- Arrythmias: Hypercalcemia can affect the electrical impulses of cardiac muscle, causing irregular heartbeats.
- Primary Hyperparathyroidism: This is often associated with hypercalcemia because it causes an increased release of parathyroid hormone (PTH) which raises serum calcium levels.
Medications[edit | edit source]
| Medication[4] | Treatment Effect | Side Effects |
| Loop Diuretics (ex; furosemide) | Flushes out excess calcium from system | Frequent urination, arrythmias, electrolyte imbalances, dizziness, muscle cramps/weakness, extreme fatigue, blurred vision, confusion, headache, dehydration, fever, sore throat, cough, skin rash, loss of appetite, nausea, vomiting[5] |
| Intravenous Biphosphonates | Prevent bone breakdown, reduce bone pain, reduce the number of pathologic fractures | Heartburn, headache, constipation, diarrhea, muscle and joint pain[6] |
| Calcitonin | Reduce bone reabsorption and slow bone loss | Warmth/redness of the skin, itching of the skin, nausea, loss of appetite, stomach pain, vomiting, skin rash, increased urination, eye pain, swelling in the feet, swelling or irritation at injection site (if injection was given)[7] |
| Glucocorticoids | Help to counter the effect of excess Vitamin D | Elevated pressure in the eyes, fluid retention that may cause swelling in the legs, increased blood pressure, mood swings, weight gain[8] |
| Hemodialysis | Remove excess waste and calcium from the bloodstream | Hypotension, muscle cramps, itching, difficulty sleeping, anemia, pericarditis, hyperkalemia, infection, depression[9] |
Diagnostic Tests/Lab Tests/Lab Values[edit | edit source]
Hypercalcemia is diagnosed by blood tests revealing increased serum calcium levels. However, other tests may need to be done in order to determine the underlying cause of hypercalcemia. These may include: [3]
- Chest X-Ray
- CT Scan
- MRI
- Mammogram
These tests may help determine whether you have lung cancer, breast cancer, other malignancies, or sarcoidosis (a granulomatous disease of the lungs). [3]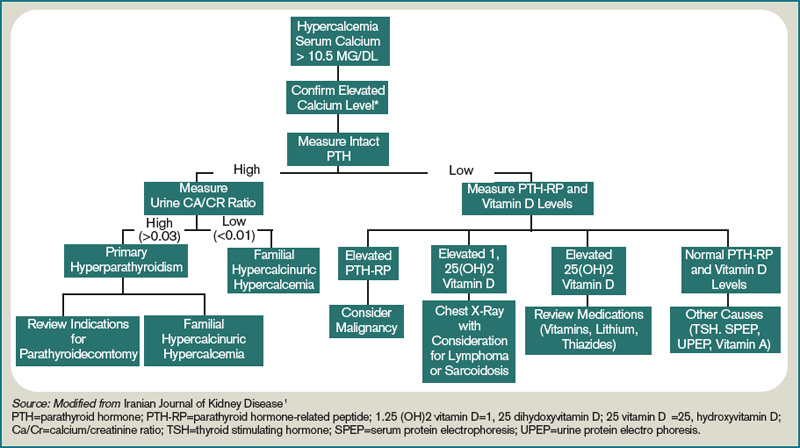
http://www.the-hospitalist.org/SpringboardWebApp/userfiles/hosp/image
Etiology/Causes[edit | edit source]
Common causes of hypercalcemia include: [10]
- Overactivity of parathyroid glands
- Cancer-specifically lung and breast cancer as well as multiple myeloma can increase the risk of hypercalcemia. This is considered to be due to the fact that some malignant tumors can produce a protein that acts similar to the parathyroid hormone which stimulates the release of calcium from the bones into the bloodstream.
- Other disease effects-some people with cancer that causes them to spend increased time lying down or in bed may cause bones to release calcium into the blood due to the lack of weight-bearing.
- Medications-Lithium, a drug used to treat bipolar disorder, may increase the release of parathyroid hormone and cause hypercalcemia. Also, Thiazie diuretics can cause elevated calcium levels by decreasing the amount of calcium excreted in the urine.
- Supplements-eating or drinking too much calcium or Vitamin D
- Dehydration-less fluid in your blood causes the calcium levels to increase
Systemic Involvement[edit | edit source]
As stated in the chart above, hypercalcemia can present with symptoms in multiple systems. Usually, the first signs and symptoms are noticed in the nervous/musculoskeletal system causing some kind of muscle pain, weakness, and/or dysfunction. However, each patient will present differently depending on the severity and organ system involved. [1]
The primary systems effects and the mechanisms of involvement are described below:
Neurological[2]
- Increased calcium levels decrease neuromuscular excitability, which leads to hypotonicity in smooth and striated muscle.
- Neuromuscular symptoms include weakness and diminished deep-tendon reflexes.
- Muscle strength is impaired, and respiratory muscular capacity may be decreased.
- Central nervous system impairment may portray as delirium, personality change, cognitive dysfunction, disorientation, hallucinations and delusions.
- Has been documented to increase cerebrospinal fluid protein, which may be associated with headache
Cardiovascular[2]
- Associated with increased myocardial contractility and irritability.
- Electrocardiographic changes are characterized by slowed conduction, including prolonged P-R interval, widened QRS complex, shortened Q-T interval, shortened or absent S-T segments.
- Incomplete or complete atrioventricular block may develop and progress to complete heart block, a systole, and/or cardiac arrest.
Gastrointestinal[2]
- Symptoms related to the depressive action of hypercalcemia on the autonomic nervous system, resulting smooth-muscle hypotonicity.
- Increased gastric acid secretion often accompanies hypercalcemia.
- Anorexia, nausea, and vomiting are made worse by increased gastric residual volume.
- Constipation is worse due to dehydration associated with hypercalcemia.
- Abdominal pain may progress to obstipation (can be confused with acute abdominal obstruction).
Renal[2]
- Loss of urinary concentrating ability and polyuria due to tubular defect in the kidney.
- Decreased fluid intake and polyuria lead to symptoms associated with dehydration.
- Decreased reabsorption of sodium, magnesium, and potassium occur as a result of salt and water depletion
- Renal insufficiency may occur as a result of diminished glomerular filtration.
Musculoskeletal[2]
- Hypercalcemia of malignancy (multiple myeloma) can result from osteolytic metastases or humerally mediated bone resorption.
- Secondary fractures, skeletal deformities, and/or pain may be symptoms present.
Medical Management (current best evidence)[edit | edit source]
Mild Hypercalcemia (defined as corrected total serum calcium level lower than 12 mg/dL (<6 mEq/L or 3.0 mmol/L)[2]
- Hydration (IV fluids) followed by observation; this option should be considered for asymptomatic patients who are about to be treated for tumors that are likely to respond to antineoplastic treatment (ex: lymphoma, breast cancer, ovarian cancer, head and neck carcinoma, and multiple myeloma).
- Additional interventions should be directed toward controlling nausea and vomiting, encouraging mobility, noting febrile episodes.
- Minimal use of sedating medications.
Moderate to Severe Hypercalcemia (defined as corrected total serum calcium equal to 12 to 14 mg/dL (6–7 mEq/L or 3.0–3.5 mmol/L)[2]
- Rehydration is the essential first step replenishing extracellular fluid, restoring intravascular volume, and saline diuresis
- Hypocalcemic agents
- Moderate doses of furosemide (20–40 mg every 12 hours) increase saline-induced urinary calcium excretion and are useful in preventing or managing fluid overload in adequately rehydrated patients.
- Surgery; resulting from primary hyperparathyroidism, urgent parathyroidectomey.
Prevention
Preventive measures include:[2]
- Ensuring adequate fluid intake of 3 to 4 L (100–140 fl oz per day if not contraindicated)
- Salt intake
- Nausea and vomiting control
- Encouraging patient mobility
- Attention to febrile episodes
- Cautious use or elimination of drugs that may complicate management ( ex: drugs that inhibit urinary calcium excretion or decrease renal blood flow, contain calcium, vitamin D, vitamin A, or other retinoids)
Physical Therapy Management (current best evidence)[edit | edit source]
- Weightbearing exercises to prevent osteoporosis and immobility
- Prevention of fractures
- Ensure adequate hydration
- Quality of life measures
- Strength/ROM
- Patient and Family Education
Alternative/Holistic Management (current best evidence)[edit | edit source]
- Increase fluid intake
- Substitute with sea salt in diet
- Decease consumption of dietary calcium and Vitamin D
- Avoid pasteurized dairy products, low-fat dairy products, and processed foods high in polyunsaturated fats and low in saturated fats
- Probiotics
Differential Diagnosis[edit | edit source]
Evaluation of a patient should include: history, physical examination focusing on clinical manifestations of hypercalcemia, risk factors for malignancy, causative medications, and a family history of hypercalcemia-associated conditions to help clinically determine effectively and accurately a differential diagnosis. [3]
- Hyperparathyroidism
- Malignancy
- Sarcoidosis
- Lithium, Salicylate, Theophylline Toxicity
- Thyroid Toxicity
- Vitamin Toxicity
- Tuberculosis
Prognosis:
The prognosis of patients with hypercalcemia depends upon the etiology of the elevation:[2]
- Prognosis is very poor with malignancy that has progressed into development of hypercalcemia.
- Prognosis is excellent when the underlying cause is treatable and treatment is initiated promptly.
Case Reports/ Case Studies
[edit | edit source]
http://www.aapsus.org/articles/6.pdf
http://annonc.oxfordjournals.org/content/11/1/97.full.pdf
Resources
[edit | edit source]
American Academy of Family Physicians
Recent Related Research (from Pubmed)
[edit | edit source]
References
[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Goodman CC, Snyder TEK. Differential Diagnosis for Physical Therapists: Screening for Referral. 5th ed. St. Louis, MO: Elsevier Saunders; 2013. Cite error: Invalid
<ref>tag; name "p1" defined multiple times with different content - ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 Hypercalcemia in Emergency Medicine [Internet]. Medscape. 2010 [updated 2010 Sep 1]. Available from:fckLRfckLRhttp://emedicine.medscape.com/article/766373-overview#a0199 Cite error: Invalid
<ref>tag; name "p2" defined multiple times with different content - ↑ 3.0 3.1 3.2 3.3 Hypercalcemia [Internet]. MayoClinic. 2012 [updated 2012 Aug 10]. Available from:fckLRfckLRhttp://www.mayoclinic.com/health/hypercalcemia/DS00976/DSECTION=causes Cite error: Invalid
<ref>tag; name "p3" defined multiple times with different content - ↑ Hypercalcemia Treatments and Drugs [Internet]. MayoClinic. 2012 [updated 2012 Aug 10]. Available from:fckLRfckLRhttp://www.mayoclinic.com/health/hypercalcemia/DS00976/DSECTION=treatments%2Dand%2Ddrugs
- ↑ Diuretics and High Blood Pressure: Uses, Side Effects, and More [Internet]. WebMD 2013. Available from:fckLRfckLRhttp://www.webmd.com/hypertension-high-blood-pressure/guide/diuretic-treatment
- ↑ Biphosphonates Uses, Side Effects, Types, Effectiveness [Internet]. WebMD. 2013. Available from:fckLRfckLRhttp://www.webmd.com/osteoporosis/bisphosphonates-for-osteoporosis
- ↑ Calcitonin Side Effects [Internet]. Drugs.com. 2013. Available from:fckLRfckLRhttp://www.drugs.com/sfx/calcitonin-side-effects.html
- ↑ Prednisone and other corticosteroids: Balance the risks and benefits [Internet]. MayoClinic. 2012 [updated 2012 Aug 10]. Available from:fckLRfckLRwww.mayoclinic.com/health/steroids/HQ01431
- ↑ Hemodialysis: Risks [Internet]. MayoClinic. 2012 [updated 2012 Aug 10]. Available from:fckLRfckLRhttp://www.mayoclinic.com/health/hemodialysis/MY00281/DSECTION=risks
- ↑ Hypercalcemia: Causes [Internet]. MayoClinic. 2012 [updated 2012 Aug 10]. Available from:fckLRfckLRhttp://www.mayoclinic.com/health/hypercalcemia/DS00976/DSECTION=treatments%2Dand%2Ddrugs
see adding references tutorial.






