Huntington's Disease Case Study
Introduction
What is Huntington's Disease?
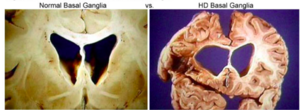
Huntington disease (HD) is an incurable, inherited disorder that occurs from gene mutation and results in the progressive degeneration of nerve cells in the brain[2].The basal ganglia is the primary location of degeneration, specifically the striatum located within it. The primary role of the basal ganglia is to coordinate movement so that it is smooth[3]. When the striatum degenerates, there is a decreased ability to inhibit unwanted movement[4]. This leads to an excessive amount of involuntary movement, known as chorea. HD affects the ability of individuals to move, think, and behave. HD typically first appears at the age of 30 to 40, however symptoms may present at any point in life[2]. HD that occurs before the age of 20 is called juvenile Huntington’s disease[2].
Pathophysiology[5]
HD has been found to occur from the mutation of the Huntington gene. The Huntington gene contains a repetition of the CAG trinucleotide protein that everyone is born with and is typically repeated anywhere between 10-35 times. The exact function of this gene is unknown, however it is believed to play a part in neural development. In HD, the mutated Huntington gene causes an increase in the number of repeats of the CAG trinucleotide, with more repetitions leading to a greater risk for the disease. It has been found that individuals with HD have the CAG trinucleotide repeat over 36 times, and in severe cases can be seen repeated over 120 times. This elongation of the protein is then fragmented into smaller sections, which accumulate on neurons within the brain and disrupt function. These neurons eventually die and the resulting neurodegeneration is associated with many of the symptoms commonly seen in Huntington’s.
Presentation
HD has been found to be heavily influenced by genetics. Everyone has the two copies of the Huntington gene, however those who have a mutation to at least one of these copies have a greater chance of experiencing the HD symptoms[6]. The inheritance of HD is autosomal dominant, which means that each child of a parent with HD has a 50% chance of inheriting the mutated copy, meaning that they have a 50% chance of inheriting the disease[7].
Signs & Symptoms[5]
Movement - chorea, dystonia, impaired gait/posture/balance, speech/swallowing, eye movement
Cognitive - difficulty organizing tasks, lack of impulse control, lack of awareness of their behaviours, troubles finding words, learning new information
Behavioural - depressive symptoms such as sadness, apathy, social withdrawal, insomnia, fatigue
Purpose of Discussing HD in a Case Study Format
The physiotherapy management of Huntington’s Disease is highly variable and highly dependent on the symptoms. This fictional case gives an opportunity for both physiotherapists and physiotherapy students to discuss and reflect about the route of assessment taken in order to prepare for clinical cases that may be observed. The discussions surrounding a simulated case allow for a significant learning opportunity for all involved, and overall an improvement in the approach to assessing and managing a case such as Huntington’s Disease.
Client Characteristics
The client in this case is a 45 year old, caucasian male, named Johnny Miller (he/him). Mr. Miller has been diagnosed with Huntington’s Disease following a consultation with a neurologist. The consultation with the neurologist occurred as a result of numerous concerning signs, including accidents within the workplace and during leisure activities. Mr. Miller is currently in the early stages of Huntington’s Disease, only showing relatively minor signs and symptoms. Mr. Miller has been referred to this outpatient rehabilitation physiotherapy clinic in order to address his current impairments, as well as prevent the progressive onset of future impairments associated with Huntington’s Disease. Overall, Mr. Miller is a pleasant man, who loves to talk about his involvement as the owner, manager, and head sushi chef at 241 sushi, as well as his dog Kenny, and his 9-year-old daughter's hockey team.
Examination Findings
Subjective
History of Present Illness (HPI)
Johnny has been experiencing an increase in accidents at work over the last couple of months, such as accidentally cutting his fingers with his knife and dropping plates. Two weeks ago on April 2nd, 2021, Johnny got a deep cut on his left thumb. He started bleeding aggressively, and decided to walk into the emergency department within the next hour. He was later seen by a physician who gave him 6 stitches. The physician had noticed that Johnny was stumbling often and had difficulty with his upper limb coordination. He told the physician that he has had a difficult time at work using his knife recently, and mentioned that “it must be due to being tired”. The physician also noted that Mr. Miller had a short temper and got angry with some of the other patients in the waiting room. The physician referred Mr Miller to a neurologist for an assessment later that month. After the neurologist performed a physical examination to look at his motor and sensory functioning, an MRI and genetic test was ordered based on symptoms that suggested Huntington’s disease. The results of the MRI and genetic testing lead to Mr. Miller’s diagnosis of Huntington’s disease on May 4th, 2021.
Past Medical History (PMHx)
Diagnosed with hypertension 5 years ago, likely due to the stress of running his business. Otherwise, relatively healthy.
Family History
Mother passed away at the age of 35 due to a motor vehicle accident. His father is a relatively healthy 68 year old and lives independently in Montreal. Mr. Miller has 1 older sister who is a chemical engineer living independently in Smith Falls; she had breast cancer 3 years ago which was resolved after a mastectomy. No other relevant family history.
Medications
Atorvastastin (15 mg per day) to lower his blood pressure.
Social History (SHx)
Mr. Miller currently lives in Kingston, Ontario in a two story detached home. He lives with his wife and 4 kids who range from 4-12 years old. Mr. Miller’s house consists of 3 stairs to get inside, and 15 stairs to get to the second floor where his bedroom is located. Additionally, Mr. Miller spends much of his day at 241 Sushi where he is the Owner, Manager, and Head Chef. 241 Sushi has 10 stairs to the basement where the refrigerator and freezer are located. When not working, Mr. Miller enjoys watching the Kingston Frontenacs, with whom he is a season ticket holder, as well as coaching his 9-year-old daughter's hockey team.
Health Habits (HH)
Mr Miller does not smoke or use recreational drugs. He drinks alcohol occasionally (1-2 drinks/week). His drink of choice is rum & coke.
Current Functional Status (FnSt)
| Basic Activities of Daily Living (BADL’s) | Instrumental Activities of Daily Living (IADL’s) | Physical Activity (PA) |
|---|---|---|
| Dressing: Independent
Eating: Independent Ambulating: Independent, but reduced sense of balance as of recently when walking. Toileting: Independent Hygiene: Independent |
Shopping: Independent
Housework: Shared responsibilities with wife; lack of motivation and confidence due to symptoms Accounting: Shared responsibilities with wife; recently having difficulties with mathematics Food Preparation: Independent but more difficult due to “random jerky movements”; several incidents at work have occurred in last few months Transportation: Independent driver but becoming more anxious that one of these “jerky movements” will cause a dangerous situation. He has reduced his driving because of this unless it is necessary. |
Able to skate on ice and coach hockey, but has experienced a few falls more recently from losing balance. Mr Miller reports feeling less confident running drills and puck handling recently.
Workouts out at home in his garage 2x/week, primarily with body weight exercises and resistance bands. |
Functional History (FnHx)
**Prior to December 7th, 2020**
- Independent in all ADL’s and IADL’s.
- Able to skate on ice rink to help coach hockey for ~2 hour practice twice per week
Objective
Observation
Vital Signs
HR: 98 bpm
RR: 16 breaths per minute
BP: 127/78 (while on medication)
Pulse: Strong radial pulse, regular-regular.
AROM & PROM
All of the following movements were assessed bilaterally:
| Cervical Spine | Flexion, Extension, Side-Flexion, Rotation, Protraction, Retraction |
| Shoulder (Glenohumeral) | Flexion, Extension, Abduction, Adduction, Internal Rotation, External Rotation |
| Elbow | Flexion, Extension, Pronation, Supination |
| Wrist | Flexion, Extension, Pronation, Supination |
| Hip | Flexion, Extension, Abduction, Adduction, Internal Rotation, External Rotation |
| Knee | Flexion, Extension |
| Ankle | Dorsiflexion, Plantarflexion, Inversion, Eversion |
All joints had full active ROM, however chorea (involuntary contractions) was noted globally, with distal joints being the most affected.
All movements assessed for AROM were also assessed for PROM. All measurements were within normal limits, bilaterally. Following full and pain free PROM, therapist overpressure was applied to assess end feel. No abnormal end feels were reported at any of the assessed joints.
Strength
Manual Muscle Testing for both the upper and lower limbs was assessed. The upper limbs were assessed in order to better understand potential deficits that may be contributing to the hand dysfunction that Mr. Miller is experiencing. Lower limb assessment provided guidance as to potential causes with regards to ambulatory issues that have recently arisen for Mr. Miller.
Upon assessment, Mr. Miller presented with the following concerning outcomes:
- Grip Strength significantly reduced bilaterally (3+/5)
- Knee Extensors significantly reduce bilaterally (4-/5)
- Knee Flexors significantly reduced bilaterally (4-/5)
All other muscle groups assessed scored at least a 4+/5 at minimum. These findings provide an objective finding that can be addressed through a strengthening program to target and prevent degenerative changes associated with Huntington’s Disease.
Neurological Scan
Balance
Ambulation
Cognitive Functioning
Outcome Measures
Berg Balance Scale (BBS)
Timed Up and Go (TUG) Test
Unified Huntington's Disease Rating Scale (UHDRS)
Montreal Cognitive Assessment (MoCA)
Short Form 36 (SF-36)
Clinical Impression
Problem List
Diagnosis
Interventions
Patient Centered Goals
Intervention Approaches & Techniques
Interdisciplinary Care Team Management
Physiotherapy
Occupational Therapy
Social Worker
Psychologist
Speech Language Pathologist
Physician
Outcome Reassessment - 6 Months Post-Referral
Berg Balance Scale (BBS)
Timed Up and Go (TUG) Test
Referrals
Discharge Planning
Discussion
Case Summary
Broader Implications
Self-Study Questions
1. What is the anatomical location of neurological degeneration for an individual with Huntington’s Disease?
- Pons
- Midbrain
- Basal Ganglia
- Cerebral Cortex
2. Complete the following statement:
The inheritance of Huntington’s Disease is _____________, which means that each child of a parent with HD has a ____ chance of inheriting the disease
- Autosomal recessive, 25%
- Autosomal dominant, 50%
- Autosomal dominant, 75%
- Autosomal dominant, 100%
3. Which of the following signs, symptoms, and observations may point to suspicion of Huntington’s Disease?
- Chorea
- Depression/Sadness
- Impaired balance
- A & C
- All of the Above
Answers: 1: 3, 2: 2, 3: 5
Explanations:
- 3 is correct. Specifically, the striatum within the basal ganglia is the primary site of degeneration in the brain for individuals with HD. When degeneration of the stratum occurs, there is a decreased ability to inhibit excessive movement (2, 3).
- 2 is correct. The inheritance of HD is autosomal dominant, which means that each child of a parent with HD has a 50% chance of inheriting the mutated copy, meaning that they have a 50% chance of inheriting the disease (6).
- 5 is correct. There are many cognitive, behavioral, and movement signs and symptoms which may indicate HD. Potential signs, symptoms, and observations could include chorea (excessive involuntary movement), depressive symptoms, and impaired gait posture, and balance.
References
- ↑ (4)
- ↑ 2.0 2.1 2.2 Folstein SE. Huntington's Disease: A Disorder of Families. The Johns Hopkins University Press. 1989
- ↑ Reiner A, Dragatsis I, Dietrich P. Genetics and neuropathology of Huntington's disease. Int Rev Neurobiol. 2011;98:325-72. Doi 10.1016/B978-0-12-381328-2.00014-6.
- ↑ Waldvogel HJ, Kim EH, Tippett LJ, Vonsattel JP, Faull RL. The Neuropathology of Huntington's Disease. Curr Top Behav Neurosci. 2015;22:33-80. doi: 10.1007/7854_2014_354.
- ↑ 5.0 5.1 Roos RA. Huntington's disease: a clinical review. Orphanet J Rare Dis. 2010 Dec 20;5:40. doi: 10.1186/1750-1172-5-40
- ↑ Myers RH. Huntington's disease genetics. NeuroRx. 2004 Apr;1(2):255-62. doi: 10.1602/neurorx.1.2.255
- ↑ Conneally PM. Huntington disease: genetics and epidemiology. Am J Hum Genet. 1984 May; 36(3): 506-26. Doi: https://doi.org/10.1016/0888-7543(89)90062-1






