Goal Attainment Scaling: Difference between revisions
No edit summary |
No edit summary |
||
| Line 52: | Line 52: | ||
2. Weight goals | 2. Weight goals | ||
Done by patient ranking goals by importance or using a weighting scale. Here the team may rank or weigh goals by the expected difficulty in achieving them. | * Done by patient ranking goals by importance or using a weighting scale. Here the team may rank or weigh goals by the expected difficulty in achieving them. | ||
Weight = importance × difficulty | Weight = importance × difficulty | ||
[[File:GAS weighing .png|center|frameless|603x603px]] | |||
3. Define the expected outcome | |||
* Assign descriptors of results in each case of -2 up to +2. Each level should be as objective and observable as possible. | |||
* This is an opportunity to address unrealistic expectations which may be held by the patient and/or caregivers. | |||
4. Scoring baseline | |||
* Usually baseline scores are rated at -1, unless there is no clinically plausible worse condition. In this case -2 is rated. | |||
5. Goal attainment scaling | |||
Goals are reviewed at appointed dates. Here, actual performance is judged at defined levels. The ideal is to have this is performed with the team - including the family. | |||
Baseline scores are compared with currently performed tasks. | |||
The use of weighted values are used within a formula in order to get a standardised score. | |||
== Resources == | == Resources == | ||
Revision as of 20:46, 16 November 2022
Original Editor - User Name
Top Contributors - Lauren Heydenrych
Introduction[edit | edit source]
Goal Attainment Scaling or GAS is a goal setting technique which has a mathematical basis.[1] GAS was first introduced in the 1960s by Kirusek and Sherman. This was originally for the mental health setting. Since then it has been adapted and modified to include a variety of areas and settings.[2]
GAS is important, as it allows the various stakeholders in the rehabilitation process - and primarily the patient - involvement in measurement and scoring of goals. GAS gives individuals the ability to construct their own outcome measures; this is in contrast to measures which are based on a standard set of tasks. Scoring, however, is performed in a standardised way which in turn allows for statistical analysis.
Advantages in using GAS[edit | edit source]
- Encourages communication and collaboration between multidisciplinary team members.[1]
- Promotes patient involvement. In research cited by Turner-Stokes (2009) goals for rehabilitation are more likely achieved with the involvement of the patient and their family. In addition, more information sharing is noted at the beginning of a rehabilitation process when formalised goal setting is introduced. This in turn allows for negotiation of realistic goals.[1]
Definition[edit | edit source]
The Shirley Ryan Abilitylab defines GAS as "an individualized outcome measure involving goal selection and goal scaling that is standardized in order to calculate the extent to which a patient's goals are met."[3]
Assessment type[edit | edit source]
Patient-reported outcomes
Diagnosis/Conditions[edit | edit source]
- Brain injury
- Cerebral Palsy
- Pain management
- Parkinson's' Disease
- Neurologic Rehabilitation
- Sports and Musculoskeletal
Description[edit | edit source]
GAS comprises of goals divided into a 5-point scale from -2 to +2.
- Achievement of goal = 0
- Achieved somewhat more than expected outcome = +1
- Achievement of much more than expected goal = +2
- Achievement of somewhat less than expected goal = -1
- Achievement of much less than expected goal = -2
As some goals may be more difficult to achieve than others and some may be more important than others, the option of weighing different goals is a possibility. A spreadsheet to help calculate goals scores, including their weighting can be found at various sites, including Assesschild.com (found in the resources list at the bottom of the page).
There is no set limit to how many or how few goals can be set at any one time.
Procedure[edit | edit source]
- Identify goals
- 1. Interview patient and/or caregivers to identify a) problem areas and b) priority areas.
- Decide on a date of achievement
- Note: Goals should follow the SMART principle
2. Weight goals
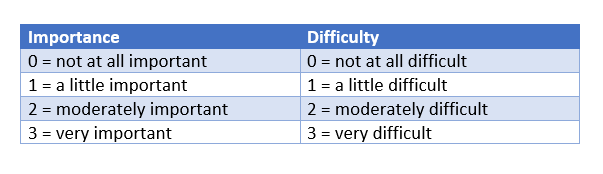
- Done by patient ranking goals by importance or using a weighting scale. Here the team may rank or weigh goals by the expected difficulty in achieving them.
Weight = importance × difficulty
3. Define the expected outcome
- Assign descriptors of results in each case of -2 up to +2. Each level should be as objective and observable as possible.
- This is an opportunity to address unrealistic expectations which may be held by the patient and/or caregivers.
4. Scoring baseline
- Usually baseline scores are rated at -1, unless there is no clinically plausible worse condition. In this case -2 is rated.
5. Goal attainment scaling
Goals are reviewed at appointed dates. Here, actual performance is judged at defined levels. The ideal is to have this is performed with the team - including the family.
Baseline scores are compared with currently performed tasks.
The use of weighted values are used within a formula in order to get a standardised score.
Resources[edit | edit source]
or
- numbered list
- x
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Turner-Stokes L. Goal attainment scaling (GAS) in rehabilitation: a practical guide. Clinical rehabilitation. 2009 Apr;23(4):362-70.
- ↑ Turner-Stokes L. Goal Attainment Scaling (GAS) in rehabilitation: A practical guide. Clinical Rehabilitation. 2009 Feb [cited 2022 Nov 15];23: 362. Available from: DOI: 10.1177/0269215508101742
- ↑ Shirley Ryan Ability Lab. Goal Attainment Scale. Available from: https://www.sralab.org/rehabilitation-measures/goal-attainment-scale (accessed 09/11/2022)