Gastric Cancer: Difference between revisions
Corey Malone (talk | contribs) No edit summary |
No edit summary |
||
| Line 298: | Line 298: | ||
== Medical Management (current best evidence) == | == Medical Management (current best evidence) == | ||
Medical managment of stomach cancer is dependent on its stage. The most common form of intervention is surgery, mainly emphasizing removal or part or all of the stomach. Radiation or chemotherapy may also be indicated should the cancer have metastisized to lymph nodes or other structures. Three common surgical interventions include endoscopic mucosal resection, subtotal (partial) gastrectomy, and total gastrectomy. Endoscopic mucosal resection is indicated when the cancer has not spread beyond the inner lining of the stomach. The surgeon removes the cancerous cells via a long tube which travels down the esophagus and into the stomach. A subtotal or partial gastrectomy is when only part of the stomach is removed. In this case, the cancer has spread significantly to the point in which it cannot be treated endoscopically. In addition, removal of a portion of the esophagus, small intestine, or nearby lymph nodes may also be indicated with this procedure. A total gastrectomy is when the cancer has invaded the entire stomach and it needs to be removed completely. Patients that have underwent a total gastrectomy must eat more often and in very small amounts. Palliative treatment is often times indicated for patients in the more severe stages of gastric cancer (III and IV). The cancer has invaded the body to the point where a complete cure it is difficult. Palliative treatment aims to subside the effects of cancer as much as possible without actually curing it. For example, a stage III or IV tumor can put pressure against the esophagus, making eating difficult. A palliative treatment technique for this may involve the placement of a stent in the esophagus, or lazer beam therapy to vaporize that portion of the tumor. | |||
== Physical Therapy Management (current best evidence) == | == Physical Therapy Management (current best evidence) == | ||
Revision as of 05:39, 15 February 2013
Original Editors -Nick Goulooze & Corey Malone from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Lead Editors - Your name will be added here if you are a lead editor on this page. Read more.
Definition/Description[edit | edit source]
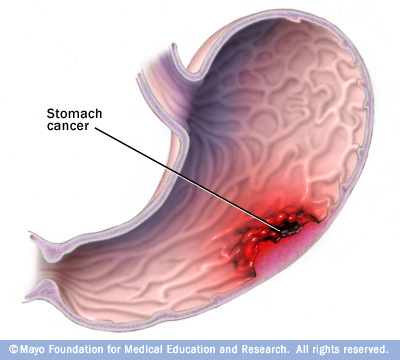
Gastric cancer (also known as stomach cancer) is characterized by rapid or abnormal cell growth within the lining of the stomach, forming a tumor.[1]
There are several different types of gastric cancer. This is because there are different types of cells which make up the stomach. Therefore each particular cell has its own type of cancer.
Adenocarcinoma
This is the most common type of gastric cancer (95% of gastric cancers[3]). This particular type of stomach cancer originates in the lining of the stomach, and effects the glandular cells of the stomach. It is believed that the majority of stomach cancer cases are caused by Heliobacter pylori bacteria.[3]
Carcinoid
This type of stomach cancer effects the stomach's hormone producing cells. Carcinoid cells reproduce very slowly, and are incredibly rare. After the cancer has progressed a significant amount, a patient may have symptoms such as flushing of the face and chest, trouble breathing, and diarrhea. This is believed to be caused by hormones from the stomach.[3]
Gastrointesinal Stromal Tumor
This type of stomach cancer originates in the nervous tissue surrounding the stomach, and is very rare.[3]
Lymphoma
Rarely, cancer will spread from the lymphnodes within and around the stomach, causing gastric cancer.[3]
As common with any type of cancer, gastric (stomach) cancer can present in various stages, ranging from mild to severe.
| Stage 0 | Stage I | Stage II | Stage III | Stage IV |
| Abnormal cells discovered within inner lining (mucosa) of stomach wall, aka carcinoma in situ. |
A) Cancer has spread to submucosa, which is the stomach layer immediately following the inner lining or mucosa. B) Cancer has invaded submucosa as well as 1-2 lymph nodes near the stomach. |
A) Cancer may have spread through several layers of the stomach including the muscularis propria (main muscle layer) and subserosa and found in 3-6 nearby lymph nodes. B) Cancer continues to spread through layers of the stomach, potentially reaching all layers. It has invaded 7+ lymph nodes and may have begun to grow in other nearby organs or tissues. |
A) Similar to IIB, cancer continues to invade layers of stomach and nearby lymph nodes; can involve nearly all muscle layers and a few lymph nodes, or a couple muscle layers and many lymph nodes. B) Cancer growth in nearby organs or tissues really begins to accelerate. C) Cancer has spread through all layers of stomach and 7+ nearby lymph nodes, or cancer has invaded nearby organs and 3+ lymph nodes. |
Cancer has metastisized to distant organs or body parts. |
Prevalence
[edit | edit source]
Estimated new cases and deaths from stomach cancer in the United States in 2012:[6]
New cases: 21,320
Deaths: 10,540
Characteristics/Clinical Presentation
[edit | edit source]
| Localized |
25% |
| Regional |
31% |
| Distant Metastatic |
32% |
| Unstaged | 12% |
- Signs and symptoms tend to arise later in the disease process, time frame is variable.
- Subjective presentations: Indigestion, bloating, nausea, heartburn, blood in stool, unexplained weight loss, vomiting, difficulty swallowing
- Objective gatherings: Enlarged stomach, swollen lymph nodes, palpable mass, skin conditions, jaundice[7][8]
All of these signs and symptoms should be carefully examined by the physical therapist when treating a patient. Also, look for signs of referred pain. The stomach's referral pattern is in the epigastric region, the left upper quadrant, and within the midscapular region. You should stop treatment and refer your patient to a doctor immediately if you recognize a number of these signs and symptoms associated with these areas of pain.[9]
Associated Co-morbidities[edit | edit source]
- A Study conducted by Heemskerk et al investigated associated co-morbidities upon history intake of 235 patients diagnosed with gastric cancer between 1992-2004.
- 138 of the 235 patient had at least one co-morbidity
| Co-morbidity | No. of Patients | % |
| Cardiovascular | 87 | 37 |
| Pulmonary | 24 | 10 |
| Diabetes | 19 | 8 |
| Other carcinoma | 20 | 9 |
| Previous GI surgery | 18 | 8 |
| BMI > 30 | 12 | 5 |
| Clotting disorder | 2 | 1 |
| Other | 11 | 5 |
Medications[edit | edit source]
There are many medications that are used for gastric cancer, each one prescribed by the patient's physician. Before a specific medication is prescribed to the patient, the physician should go through an extensive overview of the history of the patient, looking for history of allergic reactions to certain drugs. The patient should also be warned of adverse side effects that could effect the patient's everyday activities.
Doxorubicin Hydrochloride (DH)
Doxorubicin Hydrochloride is used in conjunction with a number of other medications in order to treat a number of cancers including gastric cancer. It is in the class of drugs called anthracyclines, and it works by stopping or slowing the growth of cancer cells in a person's body.[11]
There are many possible side effects of DH, but those that can effect PT are:[11]
- nausea
- vomiting
- stomach pain
- diarrhea
- increased thirst
- unusual tiredness or weakness
- dizziness
- pain, burning, or tingling in the hands or feet
Fluorouracil
Fluorouracil is a type of chemotherapy used in conjunction with other cancer medications which helps to slow/stop the growth of cancer cells. It is in the class of drugs called antimetabolites.[12]
Fluorouracil has many side effects, however some are more severe than others. There are a number of side effects that should be taken very seriosuly while on fluorouracil, and if your patient shows any of the following, you should stop treatment and send the pt. to their doctor:[12]
- sores in the mouth and throat
- diarrhea
- vomiting
- swelling, pain, redness, or peeling of skin on the palms and soles of the feet
- fever, chills, sore throat, or other signs of an infection
- hives
- rash
- itching
- difficulty breathing or swallowing
- nosebleeds
- coughing up or vomiting blood or material that looks like coffee grounds
- unusual bleeding or bruising
- pink, red, or dark brown urine
- red or tarry black bowel movements
- chest pain
Docetaxel
Docetaxel can be used with other treatments, or can be used alone, in order to treat stomach cancer. It is in the classification of taxanes, which stops the growth and spreading of cancer cells. [13]
Call the doctor immediately if you or your patient shows any of the following signs while on docetaxel:[13]
- blistering skin
- numbness, tingling, or burning sensation in the hands or feet
- weakness in the hands and feet
- unusual bleeding or bruising
- nosebleeds
Trastuzumab
Trastuzumab is used if a patient's stomach cancer has spread to other parts of the body. It is in the classification of medications called monoclonal antibodies, and helps stop the growth of cancer cells. Warning: may cause serious or life-threatening heart problems! [14]
Call the doctor immediately if you or your patient shows any of the following signs while on trastuzumab:[14]
- sore throat, fever, chills, difficulty urinating, pain when urinating, and other signs of infection
- nosebleeds and other unusual bruising or bleeding
- excessive tiredness
- pale skin
Mitomycin C
<uMitomycin is a type of antibiotic only used with patients going through chemotherapy.[15]
Call the doctor immediately if you or your patient shows any of the following signs while on mitomycin C:[15]
- unusual bruising or bleeding
- pain, redness, or swelling at the injection site
- fever
- chills
- sore throat
- cough
- rash
- itching
- difficulty urinating
- swelling of the ankles or feet
- dizziness
- shortness of breath or difficulty breathing
Diagnostic Tests/Lab Tests/Lab Values[edit | edit source]
All of the following tests are done in order to either to diagnose for gastric cancer or to determine what stage the cancer is in, in order to determine the best treatment approach for that patient. Following are a number of diagnostic and special tests.
Endoscopy[16]
This is a diagnostic procedure involving a thin tube with a camera inside of it that is passed through you esophagus into your stomach. This allows your doctor to find any suspicious tissue within your stomach that should be tested for cancer. If your doctor decides to send stomach tissue off to a lab to check for cancer, this is called a biopsy in which test can be done to determine if the suspicious tissue is malignant or benign.
Imaging[16]
-CT scan
-PET
-MRI
Exploratory Surgery[16]
This is performed should the doctor suspect your cancer has spread beyond just the stomach tissue. This procedure is done laparoscopically
Physical Exam[18]
The doctor may check for enlarged lymph nodes, an enlarged liver, increased fluid in the abdomen (ascites), or abdominal lumps felt during a rectal exam.
Upper GI Series[18]
These are X-rays of the esophagus, stomach, and first part of the intestine taken after you drink a barium solution. The barium outlines the stomach on the X-ray, which helps the doctor, using special imaging equipment, to find tumors or other abnormal areas
Etiology/Causes
[edit | edit source]
Research is still being conducted as to what actually causes stomach cancer. However, its has been shown to correlate with the following demographics and medical histories...[19][20]
- Diets high in sodium
- Men are two times more as risk than women
- African-Americans and Asians are at greater risk
- Blood group A
- Middle age to elderly
- Family history of stomach cancer
- Helicobacter pylori
- Any other past medical history of gastrointestinal complications or surgery
- Toxin exposure and smoking
Stomach conditions can often times serve as pre-cursors to cancer. For example,atrophic gastritis is when the stomach glands have decreased and are inflamed. Another disease contributing to the progression of stomach cancer may be intenstinal metaplasia. This occurs when cells within the lining of the intestine invade the stomach and take the place of stomach cells. Both conditions may occur secondary to the presence of the Helicobacter pylori infection, which is said to convert food particles into chemicals that cause mutations within the DNA of stomach cells, leading to cancer. Thus, consumption of foods high in antioxidants is said decrease the risk of stomach cancer by blocking the action of these chemicals on the stomach. [21]
Systemic Involvement[edit | edit source]
Surgery Side Effects
The major surgery that patients with gastric cancer recieve is called a gastrectomy, which is where part or all of the patient's stomach is removed. When this happens, many changes will occur in the patient's diet because their body starts to process food differently. For instance, when the entire stomach is removed, the patient will not be able to absorb the vitamin B12[22]. If this happens, the patient will become anemic[23], and therefore must recieve injections of B12. The patient must also slowly resume a normal solid diet, starting with intravenous feeding and progressing to solids. Often times these patients also have cramps, nausea, diarrhea, and dizziness shortly after eating because food and liquid enter the small intestine too quickly[22]. Finally, bile may back up from the small intestine to the esophagus or the part of the stomach that wasn't removed, and can cause stomach pain[22].
Medical Management (current best evidence)[edit | edit source]
Medical managment of stomach cancer is dependent on its stage. The most common form of intervention is surgery, mainly emphasizing removal or part or all of the stomach. Radiation or chemotherapy may also be indicated should the cancer have metastisized to lymph nodes or other structures. Three common surgical interventions include endoscopic mucosal resection, subtotal (partial) gastrectomy, and total gastrectomy. Endoscopic mucosal resection is indicated when the cancer has not spread beyond the inner lining of the stomach. The surgeon removes the cancerous cells via a long tube which travels down the esophagus and into the stomach. A subtotal or partial gastrectomy is when only part of the stomach is removed. In this case, the cancer has spread significantly to the point in which it cannot be treated endoscopically. In addition, removal of a portion of the esophagus, small intestine, or nearby lymph nodes may also be indicated with this procedure. A total gastrectomy is when the cancer has invaded the entire stomach and it needs to be removed completely. Patients that have underwent a total gastrectomy must eat more often and in very small amounts. Palliative treatment is often times indicated for patients in the more severe stages of gastric cancer (III and IV). The cancer has invaded the body to the point where a complete cure it is difficult. Palliative treatment aims to subside the effects of cancer as much as possible without actually curing it. For example, a stage III or IV tumor can put pressure against the esophagus, making eating difficult. A palliative treatment technique for this may involve the placement of a stent in the esophagus, or lazer beam therapy to vaporize that portion of the tumor.
Physical Therapy Management (current best evidence)[edit | edit source]
-Lymph therapy
-Exercises during chemo treatment to prevent atrophy of musculoskeletal system due to side effects of treament
-PT post cancer to restore loss of function that may have occured during medical management of cancer
Alternative/Holistic Management (current best evidence)[edit | edit source]
add text here
Differential Diagnosis[edit | edit source]
Differential Diagnoses[24]
Esophageal Cancer
Esophageal Stricture
Esophagitis
Gastric Ulcers
Gastritis, Acute
Gastritis, Atrophic
Gastritis, Chronic
Gastroenteritis, Bacterial
Gastroenteritis, Viral
Lymphoma, Non-Hodgkin
Malignant Neoplasms of the Small Intestine
http://emedicine.medscape.com/article/278744-differential
Case Reports/ Case Studies[edit | edit source]
add links to case studies here (case studies should be added on new pages using the case study template)
Resources
[edit | edit source]
add appropriate resources here
Recent Related Research (from Pubmed)[edit | edit source]
see tutorial on Adding PubMed Feed
References[edit | edit source]
see adding references tutorial.
- ↑ The Free Dictionary. Stomach Cancer. http://medical-dictionary.thefreedictionary.com/stomach+cancer (accessed 2 Feb 2013)
- ↑ http://www.riversideonline.com/source/images/image_popup/c7_stomach_cancer.jpg
- ↑ 3.0 3.1 3.2 3.3 3.4 Livestrong. What are different types of gastric cancer. http://www.livestrong.com/article/102412-different-types-gastric-cancer/ (accessed Feb 13 2013)
- ↑ National Cancer Institute. Stages of gastric cancer. http://www.cancer.gov/cancertopics/pdq/treatment/gastric/Patient/page2#Keypoint9 (Accessed 2/14/13)
- ↑ Cancer. How is stomach cancer staged. http://www.cancer.org/cancer/stomachcancer/detailedguide/stomach-cancer-staging (Accessed 2/14/13)
- ↑ National Cancer Institute at the National Institutes of Health. Stomach (Gastric) Cancer. http://cancer.gov/cancertopics/types/stomach (accessed 2 Feb 2013)
- ↑ Medscape. Gastric Cancer Clinical Presentation. http://emedicine.medscape.com/article/278744-clinical#a0217 (accessed 2 Feb 2013)
- ↑ National Cancer Institute at the National Institutes of Health. General Information About Gastric Cancer. http://www.cancer.gov/cancertopics/pdq/treatment/gastric/Patient/page1 (accessed 2 Feb 2013)
- ↑ Anatomy Notes. Referred Pain. http://anatomynotes.blogspot.com/2006/10/referred-pain.html (accessed Feb 13 2013)
- ↑ Vincent H., Fanneke L., Karel H., Anton H. Gastric carcinoma: review of the results of treatment in a community teaching hospital. World Journal of Surgical Oncology 2007; 5:81
- ↑ 11.0 11.1 MedlinePlus. Doxorubicin. http://www.nlm.nih.gov/medlineplus/druginfo/meds/a682221.html (accessed Feb 12 2013)
- ↑ 12.0 12.1 Medline Plus. Fluorouracil Injection. http://www.nlm.nih.gov/medlineplus/druginfo/meds/a682708.html (accessed Feb 13 2013)
- ↑ 13.0 13.1 Medline Plus. Docetaxel Injection. http://www.nlm.nih.gov/medlineplus/druginfo/meds/a696031.html (accessed Feb 13 2013)
- ↑ 14.0 14.1 Medline Plus. Trastuzumab Injection. http://www.nlm.nih.gov/medlineplus/druginfo/meds/a699019.html (accessed Feb 13 2013)
- ↑ 15.0 15.1 Medline Plus. Mitomycin. http://www.nlm.nih.gov/medlineplus/druginfo/meds/a682415.html (accessed Feb 13 2013)
- ↑ 16.0 16.1 16.2 Mayo Clinic. Stomach Cancer Tests and Diagnosis. http://www.mayoclinic.com/health/stomach-cancer/DS00301/DSECTION=tests-and-diagnosis (accessed 2 Feb 2013)
- ↑ http://www.newcastlesurgery.com.au.php53-22.ord1-1.websitetestlink.com/wp-content/uploads/2012/06/gastroscopy.gif
- ↑ 18.0 18.1 WebMD. How is Stomach Cancer Diagnosed. http://www.webmd.com/cancer/stomach-gastric-cancer?page=2 (accessed 2 Feb 2013)
- ↑ Mayo clinic. Stomach cancer causes. http://www.mayoclinic.com/health/stomach-cancer/DS00301/DSECTION=causes (accessed 2/13/13)
- ↑ WebMD. Stomach cancer. http://www.webmd.com/cancer/stomach-gastric-cancer (Accessed 2/13/13)
- ↑ Cancer. Stomach cancer causes, risk factors, and prevention topics. http://www.cancer.org/cancer/stomachcancer/detailedguide/stomach-cancer-what-causes (Accessed 2/14/14)
- ↑ 22.0 22.1 22.2 Cancer Compass. Stomach Cancer. http://www.cancercompass.com/stomach-cancer-information/side-effects.htm (accessed Feb 14 2013)
- ↑ WebMD. Vitamin B12 Deficiency Anemia. http://www.webmd.com/a-to-z-guides/vitamin-b12-deficiency-anemia-topic-overview (accessed Feb 14 2013)
- ↑ Medscape. Gastric Cancer Differential Diagnoses. http://emedicine.medscape.com/article/278744-differential (Accessed 2/13/13)