Fibromyalgia
Original Editors - Students from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Lead Editors - Your name will be added here if you are a lead editor on this page. Read more.
Definition/Description[edit | edit source]
Fibromyalgia is a syndrome characterized by widespread chronic unabated pain in addition to a host of several additional co-morbidities that can severely impact and disrupt a person’s daily life. The symptoms associated with fibromyalgia stem from abnormal sensory processing believed to originate in the muscle and ultimately lead to the chronic pain and paresthesias experienced by those with the disorder.[1]
Prevalence[edit | edit source]
The prevalence of fibromyalgia ranges from 2-6% of the population.[2] Fibromyalgia is more prevalent among women and the vast majority of those with fibromyalgia are women. Below are the prevalence and percentage of fibromyalgia patients distributed between the sexes:
Prevalence: Women (3.4%) Men (0.5%) [2]
Percentage of Fibromyalgia Patients: Women (75-90%) Men (10-25) [1]
Although most diagnoses of fibromyalgia are made during middle-age, prevalence of the disorder increases with age. [2]
Characteristics/Clinical Presentation[edit | edit source]
Those with fibromyalgia can present with a host of symptoms that can make diagnosing the disorder difficult. Below is an extensive but not exclusive list of common patient symptoms and presentations created from several sources:
- Morning stiffness [2][3]
- Tingling or numbness in hands and feet [2][3]
- Headaches, migraines [2][3][4]
- Constipation, diarrhea [2][3][4]
- Thinking and memory abnormalities (“fibro fog”) [2][3][4][5]
- Painful menstrual periods [2][3][4]
- Fatigue [3][4][5]
- Trouble sleeping [3][4][5]
- Jaw Pain [3][4]
- Abnormal muscle pain and malaise after exercise [3][4]
- Dizziness or lightheadedness [3][4]
- Skin and chemical sensitivities [3][4]
- Deep, aching, throbbing, shooting, radiating, stabbing pain [4][5]
- Non-cardiac chest pain, heart palpitations, shortness of air, profuse sweating [4]
- Feeling of swollen extremities [4]
- Sensitivities to all the senses (loud noises, bright lights, some foods, odors, etc…) [4]
- Feelings of depression, anxiety [5]
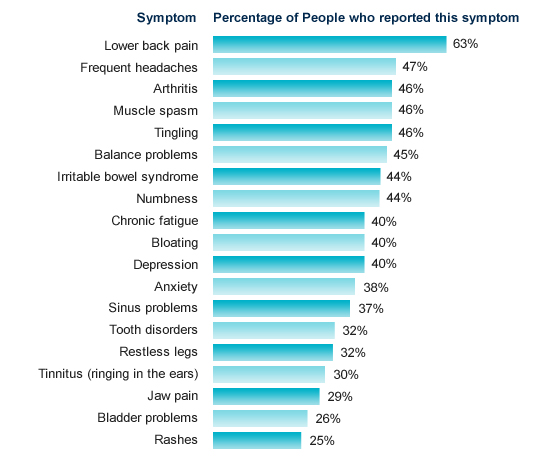
The percentage of people with fibromyalgia who have reported specific symptoms is illustrated below:
[Chart courtesy of Fibrocenter.com. Available at http://fibrocenter.com/fibromyalgia-symptoms.aspx.]
The following have been associated with aggravating the above symptoms [4]:
- Changes in weather
- Cold environments
- Hormonal fluctuations
- Stress, depression, anxiety
- Physical over-exertion
In addition to the above physical symptoms associated with fibromyalgia, the patient’s quality of life of is also a consideration as quality of life outcome measures can add to the clinical presentation. It has been reported that those with fibromyalgia have scored the lowest on 7 of 8 subscales on the SF-36 outcome measure in contrast to patients with other chronic diseases.[2] More information on the SF-36 is available at http://www.sf-36.org/. The same source revealed that fibromyalgia patients reported an average score of 4.8/10 with 1 being the lowest and 10 being the highest regarding their perceived “present quality of life.” [2]
Associated Co-morbidities[edit | edit source]
Those with fibromyalgia are likely to present with several co-morbidities. In fact, the vast majority of those with the disorder report the presence of overlapping conditions. Because the presence of additional disorders is so common in those with fibromyalgia it is important that a diagnosis of fibromyalgia not be overlooked given the presence of additional co-morbidities that are more predictable and much easier to diagnose. Below is a list of common co-morbidities associated with fibromyalgia:
- Gulf War Syndrome[4]
- Depression, anxiety[5]
Adults with fibromyalgia are 3.4 times more likely to suffer from depression than those without the disorder.[2]
- Interstitial Cystitis[5]
- Dysregulation Spectrum Syndrome(DSS): A term developed by Dr. Muhammad Yunis to include and describe the most common co-morbidities associated with fibromyalgia and how they are all inter-related. DSS includes the following: [3]
-Chronic Fatigue Syndrome (CFS)
-Multiple Chemical Sensitivity Syndrome (MCS)
-Myofascial Pain Syndrome (MPS)
-Periodic Limb Movement during Sleep (PLMS)
-Restless Legs Syndrome
-Irritable Bowel Syndrome (IBS)
-Irritable Bladder
-Primary Dysmenorrhea
-Migraines
-Tension Headaches
-Temporomandibular Joint Dysfunction (TMJD)
Medications[edit | edit source]
Prescription medication therapies are available for those with fibromyalgia. Lyrica, Cymbalta and Savella are FDA-approved to treat the disorder. However, because fibromyalgia includes an array of co-morbidities, there are several additional prescription medication options:
- Ambien, Lunesta and other sleep aids are prescribed to help with the sleep disorders common in those with fibromyalgia
- Amitriptyline, Cyclobenzaprine and others are prescribed to improve sleeping patterns, decrease pain and improve the effectiveness of the immune system.
- Opiods (Oxycontin/Oxycodon, Vicodin, Demerol, etc...) are prescribed to modulate moderate to severe pain.
Diagnostic Tests/Lab Tests/Lab Values[edit | edit source]
A diagnosis of fibromyalgia is generally made based upon the results of a physical examination and ruling out other similar conditions. It takes an average of 5 years from the time a person begins experiencing symptoms to the time they are diagnosed with fibromyalgia.[5] First, a candidate for the diagnosis has to be diagnosed with chronic pain. Chronic pain is described as pain that lasts for at least three months, pain that is both above and below the waist and pain that is present on both sides of the body.[5] In addition to the presence of chronic pain, as defined above, a patient should have at least 11 of 18 tender points illustrated below:
[Diagram courtesy of MayoClinic.com. Available at http://mayoclinic.com/health/medical/IM02372]
Administering the Physical Exam: To determine whether or not a patient has any of the tender points illustrated above, a clinician will palpate the specified areas of the body with a force that is described as the amount of pressure that “causes the nail bed to blanch or start to become white”. If the patient reports pain, that point is deemed positive for one of the eighteen tender points. [3]
Causes[edit | edit source]
The etiology of fibromyalgia is still being researched and exactly what causes the disorder remains unknown. There are, however, several potential causes and risk factors that are currently associated with the condition.
- Heredity: Current research indicates that those with a family history of fibromyalgia are more likely to develop the condition than those without a genetic predisposition.[2][5]
- Stressful and/or Traumatic Events: Psychological stress including but not limited to post traumatic stress disorder in addition to a myriad of other stressful events has been linked to the onset of fibromyalgia. [2][5]
- Bodily Injury: The onset of fibromyalgia has been linked with repetitive injuries as well as severe motor vehicle accidents and war injuries. [2][5]
- Infection: Several infections have been potentially associated with the onset of fibromyalgia including hepatitis C, the Epstein-Barr virus, parovirus and Lyme disease. [2][5]
- Disease: The presence of autoimmune disorders has been associated with fibromyalgia, including Rheumatoid arthritis and Lupus. [2][5]
Systemic Involvement[edit | edit source]
add text here
Medical Management (current best evidence)[edit | edit source]
add text here
Physical Therapy Management (current best evidence)[edit | edit source]
add text here
Alternative/Holistic Management (current best evidence)[edit | edit source]
add text here
Differential Diagnosis[edit | edit source]
add text here
Case Reports[edit | edit source]
add links to case studies here (case studies should be added on new pages using the case study template)
Resources
[edit | edit source]
add appropriate resources here
Recent Related Research (from Pubmed)[edit | edit source]
see tutorial on Adding PubMed Feed
Extension:RSS -- Error: Not a valid URL: Feed goes here!!|charset=UTF-8|short|max=10
References[edit | edit source]
see adding references tutorial.
- ↑ National Fibromyalgia Association Website. About Fibromyalgia. Available at: http://www.fmaware.org/site/PageServer?pagename=fibromyalgia_affected. Accessed 3/1/2010.