Fibromyalgia
Original Editors - Amanda Collard from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Lead Editors - Elaine Lonnemann Gayatri Jadav Upadhyay
Definition/Description[edit | edit source]
Fibromyalgia is a syndrome characterized by widespread chronic unabated pain in addition to a host of several additional co-morbidities that can severely impact and disrupt a person’s daily life. The symptoms associated with fibromyalgia may originate from abnormal central nervous system output. Fibromyalgia isn't just one condition; it's a complex syndrome involving many different factors.
Fibromyalgia is characterized by sensitization of the central nervous system, which explains the wide variation in symptoms.
[edit | edit source]
Central sensitization is known as an increased central neuronal responsiveness and causes hyperalgesia, allodynia, and referred pain and hyperalgesia across multiple spinal segments, leading to chronic widespread pain[1].
Potential causes or triggers for central sensitization include wind-up or temporal summation, dysregulation of descenting inhibitory pathways, and upregulated facilitatory modulation.
Wind-up or temporal summation results from ongoing painful stimuli. This leads to an increase in electrical discharge in the dorsal horn.
Inhibitory modulation may be affected by central nervous system abnormalities.
Upregulated facilitatory pain pathways (increased activity in pain pathways) can be stimulated by certain behavioral and cognitive factors.
Central sensitization results in an increased responsiveness to a variety of peripheral stimuli, including mechanical pressure, chemical substances, light, sound, cold, heat, and electrical stimuli. Individuals with Fibromyalgia or chronic pain have decreased tolerance to sensory input within the neuromuscular system.
|
“not only a chronic pain syndrome but also consists of a whole range of symptoms referring to effort intolerance and stress intolerance, as well as hypersensitivity for pain and other sensory stimuli.[2]” Van Houdenhove
"Multiple system output that is activated by the brain. Each individual has his/her own pain map which is activated when there is a threat or action is required.[3]" Mosely
|
Prevalence[edit | edit source]
The prevalence of fibromyalgia ranges from 2-6% of the population.[4] Fibromyalgia is more prevalent among women and the vast majority of those with fibromyalgia are women. Below are the prevalence and percentage of fibromyalgia patients distributed between the sexes:
Prevalence: Women (3.4%) Men (0.5%)[4]
Percentage of Fibromyalgia Patients: Women (75-90%) Men (10-25)Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Although most diagnoses of fibromyalgia are made during middle-age, prevalence of the disorder increases with age.[4]
Characteristics/Clinical Presentation[edit | edit source]
Those with fibromyalgia can present with a host of symptoms that can make diagnosing the disorder difficult. Below is an extensive but not exclusive list of common patient symptoms and presentations created from several sources:
- Morning stiffness[4][5]
- Tingling or numbness in hands and feet[4][5]
- Headaches, migraines[4][5][6]
- Constipation, diarrhea[4][5][6]
- Thinking and memory abnormalities (“fibro fog”)[4][5][6][7]
- Painful menstrual periods[4][5][6]
- Fatigue[5][6][7]
- Trouble sleeping[5][6][7]
- Jaw Pain[5][6]
- Abnormal muscle pain and malaise after exercise[5][6]
- Dizziness or lightheadedness[5][6]
- Skin and chemical sensitivities[5][6]
- Deep, aching, throbbing, shooting, radiating, stabbing pain[6][7]
- Non-cardiac chest pain, heart palpitations, shortness of air, profuse sweating[6]
- Feeling of swollen extremities[6]
- Sensitivities to all the senses (loud noises, bright lights, some foods, odors, etc…)[6]
- Feelings of depression, anxiety[7]
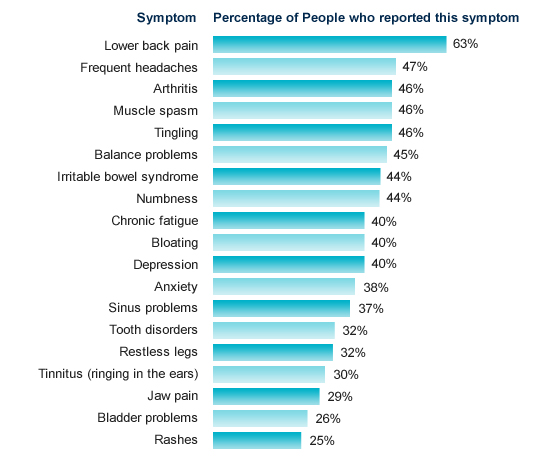
The percentage of people with fibromyalgia who have reported specific symptoms is illustrated below:
[Chart courtesy of Fibrocenter.com. Available at http://fibrocenter.com/fibromyalgia-symptoms.aspx.]
The following have been associated with aggravating the above symptoms:[6]
- Changes in weather
- Cold environments
- Hormonal fluctuations
- Stress, depression, anxiety
- Physical over-exertion
In addition to the above physical symptoms associated with fibromyalgia, the patient’s quality of life of is also a consideration as quality of life outcome measures can add to the clinical presentation. It has been reported that those with fibromyalgia have scored the lowest on 7 of 8 subscales on the SF-36 outcome measure in contrast to patients with other chronic diseases.[4] More information on the SF-36 is available at http://www.sf-36.org/. The same source revealed that fibromyalgia patients reported an average score of 4.8/10 with 1 being the lowest and 10 being the highest regarding their perceived “present quality of life.”[4]
Associated Co-morbidities[edit | edit source]
Those with fibromyalgia are likely to present with several co-morbidities. In fact, the vast majority of those with the disorder report the presence of overlapping conditions. Because the presence of additional disorders is so common in those with fibromyalgia it is important that a diagnosis of fibromyalgia not be overlooked given the presence of additional co-morbidities that are more predictable and much easier to diagnose. Below is a list of common co-morbidities associated with fibromyalgia:
Adults with fibromyalgia are 3.4 times more likely to suffer from depression than those without the disorder.[4]
- Interstitial Cystitis[7]
- Dysregulation Spectrum Syndrome(DSS): A term developed by Dr. Muhammad Yunis to include and describe the most common co-morbidities associated with fibromyalgia and how they are all inter-related. DSS includes the following:[5]
-Chronic Fatigue Syndrome (CFS)
-Multiple Chemical Sensitivity Syndrome (MCS)
-Myofascial Pain Syndrome (MPS)
-Periodic Limb Movement during Sleep (PLMS)
-Restless Legs Syndrome
-Irritable Bowel Syndrome (IBS)
-Irritable Bladder
-Primary Dysmenorrhea
-Migraines
-Tension Headaches
-Temporomandibular Joint Dysfunction (TMJD)
Medications[edit | edit source]
Prescription medication therapies are available for those with fibromyalgia. Lyrica, Cymbalta and Savella are FDA-approved to treat the disorder. However, because fibromyalgia includes an array of co-morbidities, there are several additional prescription medication options:
- Ambien, Lunesta and other sleep aids are prescribed to help with the sleep disorders common in those with fibromyalgia
- Amitriptyline, Cyclobenzaprine and others are prescribed to improve sleeping patterns, decrease pain and improve the effectiveness of the immune system.
- Opiods (Oxycontin/Oxycodon, Vicodin, Demerol, etc...) are prescribed to modulate moderate to severe pain.
Diagnostic Tests/Lab Tests/Lab Values[edit | edit source]
A diagnosis of fibromyalgia is generally made based upon the results of a physical examination and ruling out other similar conditions. It takes an average of 5 years from the time a person begins experiencing symptoms to the time they are diagnosed with fibromyalgia.[7]First, a candidate for the diagnosis has to be diagnosed with chronic pain. Chronic pain is described as pain that lasts for at least three months, pain that is both above and below the waist and pain that is present on both sides of the body.[7]
The introduction of the American College of Rheumatology (ACR) fibromyalgia classification criteria 20 years ago began an era of increased recognition of the syndrome. The criteria required tenderness on pressure (tender points) in at least 11 of 18 specified sites and the presence of widespread pain for diagnosis. Widespread pain was defined as axial pain, left- and right-sided pain, and upper and lower segment pain.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
The New ACR 2010 consists of 2 scales, the Widespread Pain Index (WPI) and the Symptom Severity (SS) scale. The modified ACR 2010 criteria eliminated the physician's estimate of the extent of somatic symptoms and substituting the sum of 3 specific self-reported symptoms. It also has a 0-31 FM Symptom scale (FS) by adding the WPI to the modified SS scale. The questionnaire was administered to 729 patients previously diagnosed with FM, 845 with osteoarthritis (OA) or with other noninflammatory rheumatic conditions, 439 with systemic lupus erythematosus (SLE), and 5210 with rheumatoid arthritis (RA).Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Causes[edit | edit source]
The etiology of fibromyalgia is still being researched and exactly what causes the disorder remains unknown. There are, however, several potential causes and risk factors that are currently associated with the condition.
- Heredity: Current research indicates that those with a family history of fibromyalgia are more likely to develop the condition than those without a genetic predisposition.[4][7]
- Stressful and/or Traumatic Events: Psychological stress including but not limited to post traumatic stress disorder in addition to a myriad of other stressful events has been linked to the onset of fibromyalgia.[4][7]
- Bodily Injury: The onset of fibromyalgia has been linked with repetitive injuries as well as severe motor vehicle accidents and war injuries.[4][7]
- Infection: Several infections have been potentially associated with the onset of fibromyalgia including hepatitis C, the Epstein-Barr virus, parovirus and Lyme disease.[4][7]
- Disease: The presence of autoimmune disorders has been associated with fibromyalgia, including Rheumatoid arthritis and Lupus.[4][7]
Systemic Involvement[edit | edit source]
Fibromyalgia has the potential to involve several systems as mentioned previously under the Characteristics/Clinical Presentation section. Fibromyalgia may involve any or all of the following systems:
- Musculoskeletal
- Urogenital
- Gastrointestinal
- Neurological/Cognitive
- Immune
Medical Management (current best evidence)[edit | edit source]
As there is currently no cure or definitive treatment protocol for the disorder, fibromyalgia research and support organizations offer those with the disease several recommendations for minimizing the negative impact fibromyalgia may bestow on patient's daily lives. The following list offers suggestions for those with fibromyalgia:[8]
- Minimize stressful situations
- Incorporate deep breathing exercise into daily routines, especially during stressful encounters
- Partake in massages or other relaxing activities
- Eat healthy and include a variety of fruits and vegetables
- Lightly exercise regularly
- Make sleep a priority and make sure to get plenty of rest
There are several additional means of medical management for those with fibromyalgia. The following are all prescribed treatment methods for those with the disorder:[5]
- Physical therapy
- Occupational therapy
- Chiropractic care
- Therapeutic massage
- Exercise programs
- Osteopathic manipulation
- Trigger point injections with lidocaine
- Relaxation techniques
- Acupuncture
Current research has produced mixed results regarding the success of the therapies listed above. One study found that behavioral insomnia therapy for patients with fibromyalgia may have a promising impact.[9] The study incorporated patient education on sleeping habits and proper sleeping schedules to reduce the bouts of insomnia experienced by those with fibromyalgia. The researchers concluded that patients who received the behavioral therapy experienced improvement in how long they slept and in their general condition compared to other groups.
Another study looked at the effect of an aquatic-based respiratory exercise program on those with fibromyalgia.[10] The researchers concluded that an aquatic respiratory exercise-based program offered several significant quality of life improvements in the participants. The program involved patients jogging, running and walking forward, backward and sideways in shoulder height water for a warm-up. Following the warm-up patients participated in respiratory exercises which included physical exercise synchronized with breathing. The session ended with relaxation exercises as a cool down.
Additional studies have focused on relaxation techniques as treatment for those with fibromyalgia and other chronic musculoskeletal pain. Progressive muscle relaxation techniqes, breathing exercises, guided imagery and mental imaginations were used for interventions and have shown some promise, especially in combination with light exercise or other treatments, however, more research is needed.[11]
Physical Therapy Management (current best evidence)[edit | edit source]
Activity Management[edit | edit source]
Exercise[edit | edit source]
According to the most recent Cochrane Review[12] (2007) assessing the benefits of Exercisel in the management of Fibromyalgia "There is 'gold' level evidence (www.cochranemsk.org) that supervised aerobic exercise training has beneficial effects on physical capacity and FM symptoms. Strength training may also have benefits on some FM symptoms. Further studies on muscle strengthening and flexibility are needed. Research on the long-term benefit of exercise for FM is needed."
- Light aerobic exercise most days of the week is highly recommended for those with fibromyalgia. In a systematic review published in theJournal of Rheumatology it was concluded that aerobic exercise training only offers those with fibromyalgia significant beneficial effects on physical function, well-being and potentiallly pain. Strength training and flexibility, however, have yet to be studied in depth.[13]
- Another study found that structured physiotherapy alone, not including aerobic exercise, as well as amitriptyline medications alone significantly decreased disability of those with fibromyalgia as measured by the Fibromyalgia Impact Questionnaire (FIQ). Physiotherapy consisted of the following[14]:
-Relaxation techniques
-Stretching
-Strengthening
- Manual lymph drainage therapy and connective tissue massage have also been studied in women with fibromyalgia. Researchers used the Fibromyalgia Impact Questionnaire and the Nottingham Health Profile to measure the impact of the treatment. Their research suggests that both manual lymph drainage therapy and connective tissue massage show improvements in both the FIQ and the Nottingham Health Profile. However, there were significantly greater improvements in the group that received manual lymph drainage therapy, suggesting that manual lymphatic drainage therapy may be preferred over connective tissue massage.[15]
Education[edit | edit source]
Education in Pain Science
Alternative/Holistic Management [edit | edit source]
No evidence to support alternative/holistic management
Differential Diagnosis[edit | edit source]
The following are all differential diagnoses for fibromyalgia. It is possible for several to be present concurrently with fibromyalgia. It is important to determine the presence of all potential facets and diagnoses in order to successfully treat a patient with suspected fibromyalgia.
- Serotonin Syndrome[16]
- Chronic Fatigue Syndrome[5]
- Hypothyroidism[17]
- Myofascial Pain Syndrome[17]
- Polymyalgia rheumatic/giant cell arteritis[17]
- Systemic lupus erythematosus[17]
- Lyme Disease[17]
- Neurosis[17]
- Metastatic Cancer[17]
- Temporomandibular Joint Dysfunction[17]
- Multiple Sclerosis[8]
Case Reports[edit | edit source]
Misdiagnosis of serotonin syndrome as fibromyalgia and the role of physical therapists. (Full Text Here)
A case-control study examining the role of physical trauma in the onset of fibromyalgia syndrome (Full Text Here)
Tailored cognitive-behavioral therapy for fibromyalgia: Two case studies. (Abstract Here)
The effect of a 4-week aerobic exercise program on muscle performance in patients with fibromyalgia . (Abstract Here)
Insular hypometabolism in a patient with Fibromyalgia: A case study. (Abstract Here)
Resources
[edit | edit source]
'Fibromyalgia Syndrome: Practical Strategies for Improving Diagnosis and Patient Outcomes' is an official and free CE/CPD activity from the American Journal of Medicine.
National Fibromyalgia Association
The American Fibromyalgia Syndrome Association
Recent Related Research (from Pubmed)[edit | edit source]
Failed to load RSS feed from http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1zA4h3Qg-ND2LumX1tyVekpGt7BR2e554efcyaSJbq7L7-0s55|charset=UTF-8|short|max=10: Error parsing XML for RSS
References[edit | edit source]
- ↑ Meeus M, Nijs J. Central sensitization: a biopsychosocial explanation for chronic widespread pain in patients with fibromyalgia and chronic fatigue syndrome. 2007 April; 26(4): 465–473.
- ↑ Van Houdenhove B, Egle UT. Fibromyalgia: a stress disorder: piecing the biopsychosocial puzzle together. Psychother Psychosom. 2004;73:267–275
- ↑ Moseley GL. Is successful rehabilitation of complex regional pain syndrome due to sustained attention to the affected limb? A randomised clinical trial. Pain 2005;114:54–61
- ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 4.11 4.12 4.13 4.14 4.15 4.16 Centers for Disease Control and Prevention Website. Fibromyalgia. Available at: http://www.cdc.gov/arthritis/basics/fibromyalgia.htm. Accessed on 3/1/2010
- ↑ 5.00 5.01 5.02 5.03 5.04 5.05 5.06 5.07 5.08 5.09 5.10 5.11 5.12 5.13 5.14 Fibromyalgia Network Website. Available at: http://www.fmnetnews.com. Accessed on 3/1/2010.
- ↑ 6.00 6.01 6.02 6.03 6.04 6.05 6.06 6.07 6.08 6.09 6.10 6.11 6.12 6.13 6.14 6.15 The American Fibromyalgia Syndrome Association, Inc. Website. What is Fibromyalgia. Available at: http://afsafund.org/fibromyalgia.html. Accessed on: 3/1/2010.
- ↑ 7.00 7.01 7.02 7.03 7.04 7.05 7.06 7.07 7.08 7.09 7.10 7.11 7.12 7.13 Fibrocenter.com Website. Available at: http://fibrocenter.com. Accessed on: 3/1/2010.
- ↑ 8.0 8.1 MayoClinic.com Website. Fibromyalgia symptoms or Not? Understand the fibromyalgia diagnosis process. Available at: http://mayclinic.com/health/fibromyalgia-symptoms/AR00054. Accessed on 3/1/2010.
- ↑ Edinger JD. Behavioral insomnia therapy for fibromyalgia patients: a randomized clinical trial. Arch Intern Med. 28 Nov 2005; 165(21): 2527-35.
- ↑ Ritomy M. Effect of aquatic respiratory exercise-based program in patients with fibromyalgia. International Journal of Rheumatic Diseases 2008; 11: 131-140.
- ↑ Persson A. Relaxation as treatemnt for chronic musculoskeletal pain-a systematic review of randomised controlled studies. Physical Therapy Reviews. 2008; 13(5): 355-363
- ↑ Busch AJ, Barber KA, Overend TJ, Peloso PMJ, Schachter CL. Exercise for treating fibromyalgia syndrome. Cochrane Database of Systematic Reviews 2007, Issue 4. Art. No.: CD003786. DOI: 10.1002/14651858.CD003786.pub2.
- ↑ Busch AJ, Schacter CL, Overend TH, Peloso PM, Barber KA. Exercise for Fibromyalgia: a Sytematic Review. The Journal of Rheumatology. 35 no. 1130-1144.
- ↑ Joshi MN, Joshi R, Jain AP. Effect of amitriptyline vs physiotherapy in treatment of fibromyalgia syndrome: What predicts a clinical benefit? J Postgrad Med 2009;55:185-9.
- ↑ Ekici G, Bakar Y, Akbayrak T, Yuksel I. Comparison of Manual Lymph Drainage Therapy and Connective Tissue Massage in Women with Fibromyalgia: a Randomized Controlled Trial. Journal of Manipulative and Physiological Therapeutics. 2009 Feb;32(2):127-33.
- ↑ Alnwick G. Misdiagnosis of Serotonin Syndrome as Fibromyalgia and the Role of Physical Therapists. Physical Therapy. Vol 88(6) June 2008.
- ↑ 17.0 17.1 17.2 17.3 17.4 17.5 17.6 17.7 Goodman, Snyder. Differential Diagnosis for Physical Therapists: Screening for Referral. St. Louis Missouri. 2007.