Electronic Medical Records: Difference between revisions
mNo edit summary |
Kim Jackson (talk | contribs) mNo edit summary |
||
| Line 24: | Line 24: | ||
<br> | <br> | ||
== References == | == References == | ||
Revision as of 23:41, 4 August 2019
Original Editor - Your name will be added here if you created the original content for this page.
Top Contributors - Ahmet Kocyigit, Admin, Laura Ritchie, WikiSysop and Kim Jackson
Introduction[edit | edit source]
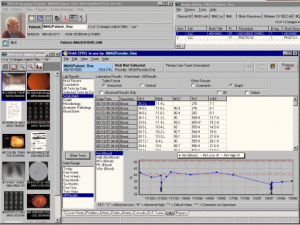
An electronic health record (EHR) (also electronic patient record (EPR) or computerised patient record) is an evolving concept defined as a systematic collection of electronic health information about individual patients or populations.[1] It is a record in digital format that is capable of being shared across different health care settings, by being embedded in network-connected enterprise-wide information systems. Such records may include a whole range of data in comprehensive or summary form, including demographics, medical history, medication and allergies, immunization status, laboratory test results, radiology images, vital signs, personal stats like age and weight, and billing information.
Purpose[edit | edit source]
Its purpose can be understood as a complete record of patient encounters that allows the automation and streamlining of the workflow in health care settings and increases safety through evidence-based decision support, quality management, and outcomes reporting.[2]
Advantages
[edit | edit source]
Disadvantages
[edit | edit source]
Governance, privacy and legal issues[edit | edit source]
References[edit | edit source]
References will automatically be added here, see adding references tutorial.
- ↑ Gunter, T.D. and Terry, N.P. 2005 The Emergence of National Electronic Health Record Architectures in the United States and Australia: Models, Costs, and Questions in J Med Internet Res 7(1)
- ↑ HIMSS - Electronic Health Record (EHR)