Diversity of Private Physiotherapy Practice: Difference between revisions
No edit summary |
No edit summary |
||
| Line 439: | Line 439: | ||
Helps promote recovery within rehabilitation process<br>· Minimizes the side effects of long-term sickness absence, which can include physical, mental and social effects.<br>· Reduces long term incapacity<br>· Helps people feel like they contribute to society, maintain their independence and have autonomy.<br>· Improves quality of life (Getting vocational rehabilitation working for Scotland: education needs of staff supporting vocational rehabilitation 2008) | Helps promote recovery within rehabilitation process<br>· Minimizes the side effects of long-term sickness absence, which can include physical, mental and social effects.<br>· Reduces long term incapacity<br>· Helps people feel like they contribute to society, maintain their independence and have autonomy.<br>· Improves quality of life (Getting vocational rehabilitation working for Scotland: education needs of staff supporting vocational rehabilitation 2008) | ||
== Specializing in Occupational Health and Ergonomic Physiotherapy == | == Specializing in Occupational Health and Ergonomic Physiotherapy == | ||
The ACPOHE is the Association of Chartered Physiotherapists in Occupational Health and Ergonomics, which is a professional network of physiotherapists within the CSP. The ACPOHE has physiotherapists who work within a variety of settings including the NHS, service industries, public and private sectors. The ACPOHE also works within retail, healthcare, offices and manufacturing environments. The association originated in 1947. In order to become a member of the ACPOHE a physiotherapist is required to demonstrate specific specialist competency in the area of Occupational health and Ergonomics. To achieve registered membership a physiotherapist must demonstrate development in occupational health by providing:<br> | The ACPOHE is the Association of Chartered Physiotherapists in Occupational Health and Ergonomics, which is a professional network of physiotherapists within the CSP. The ACPOHE has physiotherapists who work within a variety of settings including the NHS, service industries, public and private sectors. The ACPOHE also works within retail, healthcare, offices and manufacturing environments. The association originated in 1947. In order to become a member of the ACPOHE a physiotherapist is required to demonstrate specific specialist competency in the area of Occupational health and Ergonomics. To achieve registered membership a physiotherapist must demonstrate development in occupational health by providing:<br> | ||
#Evidence of educational achievements | #Evidence of educational achievements | ||
#Evidence of meeting level B on the ACPOHE OH competency framework | #Evidence of meeting level B on the ACPOHE OH competency framework | ||
#Two professional references for work in occupational health and ergonomics | #Two professional references for work in occupational health and ergonomics | ||
<br> | |||
Achieving registered membership can be achieved in three different methods. | |||
Achieving registered membership can be achieved in three different methods. | |||
<br>Educational achievement – completing a UK based masters level course that focuses on knowledge and skills in work and health. The course must be in ergonomics, occupational health and safety, vocational or occupational rehabilitation.<br> <br>Short course – the ACPOHE offers 7 courses covering competencies in occupational health and ergonomics. Completing 4 of the 7 courses allows a member to apply for registered membership. All members following this route must complete introduction to occupational health and applied ergonomics and additionally two of the following:<br> | <br>Educational achievement – completing a UK based masters level course that focuses on knowledge and skills in work and health. The course must be in ergonomics, occupational health and safety, vocational or occupational rehabilitation.<br> <br>Short course – the ACPOHE offers 7 courses covering competencies in occupational health and ergonomics. Completing 4 of the 7 courses allows a member to apply for registered membership. All members following this route must complete introduction to occupational health and applied ergonomics and additionally two of the following:<br> | ||
#Office workstation ergonomics level 1 | #Office workstation ergonomics level 1 | ||
#Office workstation ergonomics level 2 | #Office workstation ergonomics level 2 | ||
#Assessing fitness for work and function | #Assessing fitness for work and function | ||
#Occupational rehabilitation and work hardening | #Occupational rehabilitation and work hardening | ||
#Communication for better outcomes: using a cognitive behavioural approach in occupational health | #Communication for better outcomes: using a cognitive behavioural approach in occupational health | ||
#Work relevant upper limb disorders; prevention and management | #Work relevant upper limb disorders; prevention and management | ||
#Moving and handling; preventing injury and ill health at work | #Moving and handling; preventing injury and ill health at work | ||
Case study assignment – this route is intended for full members of ACPOHE who have knowledge and skills through work and personal development without taking university accredited courses or ACPOHE courses. Two in depth case studies must be submitted with one in field of expertise and one in another area to prove knowledge across specialty.<br> <br>For further information on obtaining registered membership please see the ACPOHE website. | Case study assignment – this route is intended for full members of ACPOHE who have knowledge and skills through work and personal development without taking university accredited courses or ACPOHE courses. Two in depth case studies must be submitted with one in field of expertise and one in another area to prove knowledge across specialty.<br> <br>For further information on obtaining registered membership please see the ACPOHE website. | ||
Treatment Interventions | |||
One of the main therapy tools occupational physiotherapists utilize are work hardening exercises that either simulate or mimic tasks that are functional and would normally be performed within an individual’s work setting. Work hardening exercise protocols utilize graded exercise progression to improve physical, psychological and emotional tolerance to exercise that will translate to improve work feasibility. In order to meet a work hardening exercise protocol, its components must address three key elements, which include:<br>· Exercises that chosen to help restore deficits in neurological, musculoskeletal or cardiopulmonary function<br>· Clearly stated intent to improve a patient’s work status<br>· Clearly stated connection between job demands and the intervention<br> <br>Work hardening protocols can also include behavioral approaches, pain management and condition education along with return to work advice. | |||
= '''Oncology Physiotherapy''' = | = '''Oncology Physiotherapy''' = | ||
Revision as of 17:39, 24 November 2016
Diversity of Private Physiotherapy Practice[edit | edit source]
Introduction [edit | edit source]
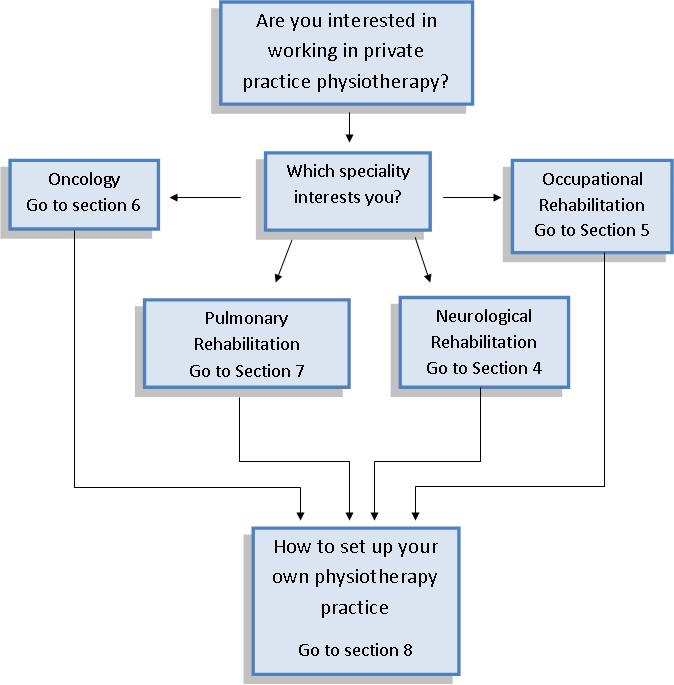
For many recently graduated physiotherapists the idea of working in private clinics is an attractive work opportunity. Many people are unaware of the various physiotherapy services offered in the private physiotherapy sector outside of musculoskeletal practices. This wiki is aimed to be a tool to assist in increasing newly graduated physiotherapists awareness of these specialties such as neurological rehabilitation, pulmonary rehabilitation, vocational/occupational rehabilitation and physiotherapy in oncology. Each section will give an in depth discussion surrounding the importance and need for these areas of physiotherapy, the efficacy and importance in providing care in private practice setting followed by an outline of steps to start up your own private physiotherapy clinic.
Table of Contents[edit | edit source]
- What is physiotherapy? Role of Physiotherapy
- Waitlists
- Development of scope of practice
- Neurological Physiotherapy
- Occupational Physiotherapy
- Oncology Physiotherapy
- Pulmonary Physiotherapy
- How to set up you own private physiotherapy practice
Learning Outcomes[edit | edit source]
What is physiotherapy? Role of a Physiotherapist [edit | edit source]
Physiotherapy is an internationally recognized profession where the physiotherapist works with service users to identify and encourage their ability to maximise their movement and function while ensuring treatment is patient centred, effective and ethical [1]). A physiotherapist has professional autonomy, allowing the physiotherapist to have the ability and freedom to use their professional judgement regarding assessment, diagnosis, treatment and care within their scope and limits of knowledge and competence [2]. The WCPT define physiotherapy as:
“Physical therapy is concerned with identifying and maximising quality of life and movement potential within the spheres of promotion, prevention, treatment/intervention, habilitation and rehabilitation. This encompasses physical, psychological, emotional, and social wellbeing. Physical therapy involves the interaction between the physical therapist, patients/clients, other health professionals, families, care givers and communities in a process where movement potential is assessed and goals are agreed upon, using knowledge and skills unique to physical therapists [3].”
The statement above demonstrates the use of a holistic approach to asses and treat service users. Many presenting symptoms can originate or be influenced by social or emotional factors therefore in order to provide truly patient centred care and improve quality of life, all aspects of the service users life such as emotional, social and physiological must be incorporated into assessment and treatment.
Physiotherapists can work in a variety of environments from hospitals, private practice clinics, community based rehabilitation centres, outpatient clinics, to schools and workplaces [4]. The scope of physiotherapy is not limited to the role in a clinic surround patient care but as well as influence public health strategies, advocating patient health, teaching, research and helping to develop health policy [5]
Further reading:
- CSP physiotherapy framework available here: https://v3.pebblepad.co.uk/v3portfolio/csp/Asset/View/6jqbh3GzhGWrrcGqpknwmZzh8Z
Waiting Times[edit | edit source]
The movement from acute to chronic conditions due to the ageing population has had a significant effect on the health care system and wait times. Waiting time is defined by the CSP as “the time between the date that a referral is received, and the date the patient attends for treatment [6]” The CSP conducted a survey of identify key points surrounding waitlist times within the UK, and found that for different specialties wait times have increased since 2010 [7]. The average waitlist times were around 6-8 weeks compared to 7 weeks in the previous survey conducted[8]
- For neurological services, the average wait time was reported to be 2-4 weeks with 83% of service users seen within 8 weeks [9].
- For occupational health services the average wait list times have improved from 3 weeks in 2010 to approximately 1 week 2011, with majority of referrals seen within 8 weeks [10].
- The full document is available online for further reading from: http://www.csp.org.uk/publications/survey-nhs-physiotherapy-waiting-times-workforce-caseloads-uk-2010-2011
As waitlist times vary in length for each specialty with patients can opt into using the private physiotherapy practices available therefore not having to wait for a long period of time for treatment.
Development of Scope of Practice[edit | edit source]
The movement from treating acute to chronic conditions due to the ageing population, the cost constraints this shift has on public services as well as impact of technology have an impact of health delivery internationally [11], and in turn an impact on the physiotherapy profession. The Canadian Physiotherapy Association state a change in scope of practice and development of physiotherapy profession is associated with this shift of treatment in healthcare; for example practices such as ordering X-rays and screening for orthopaedic surgery which were considered advance practices are now becoming under the scope of practice [12]. The recognition of advanced practitioners in specific areas such as pain and oncology is another development emerging as a result of changes in population and the demands on the healthcare system therefore broadening the scope of physiotherapy [13].
This plays an important role in the development of private physiotherapy practices as well as physiotherapy roles are changing and the scope of practice is broadening. Many people are unaware of the diverse nature of physiotherapy practice as it extends to neurological, oncology and vocational rehabilitation and is not limited to strictly musculoskeletal conditions. Therefore there is a need for increased awareness of these other specialities available to the public and to those who wish to work in these specialties.
Take a quick Quiz to Direct your Learning![edit | edit source]
Neurological Physiotherapy[edit | edit source]
You have navigated yourself to this portion of the Wiki by recognising an interest you have in Neurological physiotherapy within the private setting. This section is designed to give an introduction into neurological physiotherapy, highlight the prevalence of neurological conditions within the UK, briefly discuss neurological physiotherapy services offered by the NHS with emphasis placed on two common conditions, stroke and Parkinson's disease, and conclude by outlining the benefits of private neurological physiotherapy. This will hopefully trigger questions for thought and reflection on whether neurological physiotherapy in the NHS or private practice is suitable for the career pathway you have in mind.
Firstly, we will aim to answer the basic question of "What is Neurological physiotherapy?"
Neurological Physiotherapy is a specialist area of physiotherapy focused on the treatment of individuals with neurological conditions. Neurological disorders affect the functioning of the brain, spinal cord, and nerves. Stroke, multiple sclerosis, spinal cord injury and Parkinson’s disease are common neurological conditions [14]. It also includes conditions of the peripheral nervous system such as Guillain Barre Syndrome. Neurological conditions can have a devastating impact on the lives of the sufferers, along with family and friends. Disturbances in the travelling of messages between the brain and the body can result in the loss of movement, sensation, co-ordination, and balance. Other aspects of bodily function, such as perception, speech, memory, cognition, and behaviour may also be effected. Therefore, it is important that neurological physiotherapists work in close partnership with other members of the multidisciplinary team including speech and language therapists, occupational therapist, dieticians, nurses, and doctors. Effective communication between patient, family members, and the multidisciplinary team is critical to positive healthcare outcomes following a neurological disorder [15].
The role of a Neurological Physiotherapist[edit | edit source]
Neurological physiotherapists are experienced and trained to treat neurological conditions with the aim to provide interventions which assist an individual to regain or maintain their maximum movement and functional independence. This is achieved by aiding in the development of new pathways through repetition and exercise.
Treatment Interventions[edit | edit source]
A number of treatment approaches are used, often incorporating a selection of the following as appropriate [16]
- Stretching
- Strengthening
- Balance re-education
- Gait re-education
- Joint mobilization
- Electrical stimulation
- Postural exercise
- Spasticity management
- Advice/Education on lifestyle, fatigue management, and exercise
<img src="/images/e/e8/Stop_2.jpg" _fck_mw_filename="Stop 2.jpg" _fck_mw_location="left" _fck_mw_width="400" _fck_mw_height="400" alt="" class="fck_mw_left" />
<img src="/images/c/c2/Time_to_reflect.jpg" _fck_mw_filename="Time to reflect.jpg" _fck_mw_width="400" _fck_mw_height="400" alt="" /> .
Reflection Questions:
1. Does the role of a neurological physiotherapist still interest me?
2. Do I want to further investigate if working in the private sector would interest me?
If you have answered "yes" to the above questions, continue reading below. If not return to the career pathway in the introduction section and select another specialty that may be of interest.
</p>
<p>
Prevalence of Neurological Conditions[edit | edit source]
The Neurological Alliance [17] reported the total number of neurological cases in England to be 12.5 million or 59,000 cases per CCG in 2013-14, with a further 1 million cases in Scotland reported in the NHS QIS Clinical Standards on Neurological Health Services [18].
<img src="/images/thumb/1/13/Prevalence_of_neurological_conditions.jpg/500px-Prevalence_of_neurological_conditions.jpg" _fck_mw_filename="Prevalence of neurological conditions.jpg" _fck_mw_location="left" _fck_mw_width="500" alt="Neurological Conditions cases." class="fck_mw_left" />
This table[19]represents the most common neurological conditions in England.
Within NHS Lothian, it is estimated 53,480 people are living with a neurological condition. The number of people disabled by the condition is 5,348 and an estimated 1,872 people will need assistance carrying out activities of daily living. Each year, a further 8,489 people in Lothian will be diagnosed with a neurological condition [20]. The illustration below represents the number of people affected by neurological conditions in Lothian [21].
<img src="/images/9/90/NHS_lothian.jpg" _fck_mw_filename="NHS lothian.jpg" _fck_mw_width="800" _fck_mw_height="600" alt="" />
Public perceptions of Neurological Conditions[edit | edit source]
A study conducted by Sue Ryder revealed that 45% of the UK population feared being impacted by a neurological condition the most which is compared to 36% who feared getting cancer. The study highlighted the beliefs of the public with regards to neurological conditions, showing that 26% of the public felt that “nothing much can be done” for people with neurological conditions [22]. It is understandable why the general public fear being effected by a neurological condition when one takes into consideration patients poor experience with neurological healthcare. The Neurological Alliance conducted a <a href="http://www.neural.org.uk/store/assets/files/495/original/Invisible_patients_-_revealing_the_state_of_neurology_services_final_14_January_2015_.pdf">neurological patient experience survey</a> in 2014 <span class="fck_mw_ref" _fck_mw_customtag="true" _fck_mw_tagname="ref" name="Neurological Conditions cases" />.
<img src="/images/thumb/9/9f/Neurological_patient_experience_survey_profile.jpg/400px-Neurological_patient_experience_survey_profile.jpg" _fck_mw_filename="Neurological patient experience survey profile.jpg" _fck_mw_location="left" _fck_mw_width="400" _fck_mw_height="400" alt="" class="fck_mw_left" />
<img src="/images/7/7e/Neurological_conditions_in_the_survey.jpg" _fck_mw_filename="Neurological conditions in the survey.jpg" _fck_mw_location="right" _fck_mw_width="500" _fck_mw_height="400" alt="" class="fck_mw_right" />Figure 1 illustrates the population responding to this survey
Figure 2 indicates the neurological conditions represented in the survey.
The survey stated that 58.1% (n=3402) of NHS England respondents (n=6916) have experienced difficulty accessing the service/treatment they require, 39.8% (n= 2357) of respondents had a 12-month waiting period from the time of observation of the first symptom to seeing a neurologist specialist, 31.5% of respondents (n=2140) had 5 or more GP visits related to the health problems experienced due to their condition prior to being referred to a neurological specialist, and 71.5% (n=4603) of respondents were not provided with a care plan to help manage their condition <span class="fck_mw_ref" _fck_mw_customtag="true" _fck_mw_tagname="ref" name="Neurological Conditions cases" />
Waiting times for NHS Neurological Services[edit | edit source]
The 2005 <a href="https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/198114/National_Service_Framework_for_Long_Term_Conditions.pdf">National Service Framework for Long-term Conditions</a> [23] identified the need for prioritising an accurate and rapid diagnosis of neurological conditions, highlighting the importance of early diagnosis within this clinical population to reduce neurological damage, delay disease progression, elevate survival numbers, and enhance patient’s quality of life. However, it appears in 2014 that this call to action had not been achieved with 3,402 respondents to the neurological patient experience survey <span class="fck_mw_ref" _fck_mw_customtag="true" _fck_mw_tagname="ref" name="Neurological Conditions cases" /> voicing concerns regarding challenges experienced trying to access the treatment and services they needed.
<img src="/images/thumb/c/c5/Quote_1.png/291px-Quote_1.png" _fck_mw_filename="Quote 1.png" _fck_mw_location="left" _fck_mw_width="300" _fck_mw_height="300" alt="" class="fck_mw_left" />
Respondents opinions emphasized the concern of long waiting times especially transitioning from general practice to specialist care settings.
In December 2011, a survey of NHS Physiotherapy waiting times [24] in the UK was published, showing that in neurology departments, the longest wait reported was 2-4 weeks and 83% of neurological patients were seen in 8 weeks or less. The shortest wait was less than a week and the longest wait was 18-20 weeks.
NHS patient involvement in decision making [edit | edit source]
Only 34.1% of Clinical commissioning groups which responded to the quality of commissioning audit, utilise mechanisms to involve patients in decision-making processes and only 33% obtain important feedback on the services they provide. Taking into consideration the NHS principle of “<a href="https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/216980/Liberating-the-NHS-No-decision-about-me-without-me-Government-response.pdf">no decision about me without me</a>” [25], the NHS must actively incorporate patient views in the design and provision of services. The chart below <span class="fck_mw_ref" _fck_mw_customtag="true" _fck_mw_tagname="ref" name="Neurological Conditions cases" /> highlights the high number of neurological patients receiving no information from healthcare professionals on various aspects of patient care. Without crucial information, how is it possible for patients to make educated, informed decisions about their healthcare?
<img src="/images/thumb/9/93/Quality_of_information_.png/573px-Quality_of_information_.png" _fck_mw_filename="Quality of information .png" _fck_mw_width="600" _fck_mw_height="400" alt="Patient satisfaction with the provision of information" />
Neurology Quiz [edit | edit source]
<img src="/images/thumb/2/22/Quiz_time.jpg/200px-Quiz_time.jpg" _fck_mw_filename="Quiz time.jpg" _fck_mw_location="left" _fck_mw_width="200" _fck_mw_height="200" alt="" class="fck_mw_left" />
Please click on the link to test your basic <a href="https://www.proprofs.com/quiz-school/story.php?title=mtc2mja0mao9u0">neurology knowledge</a>. As a newly graduated physiotherapist, you should be competent in this information and scoring 100%, but you may find the quiz helpful to refresh your memory before we discuss the provision of stroke and Parkinson's disease services.
Stroke[edit | edit source]
Stroke prevalence in the UK[edit | edit source]
A stroke is a type of cerebrovascular disease. A stroke occurs when the blood supply to part of the brain is disrupted, depriving brain cells of oxygen and nutrients. Below the left scan shows an infarct represented by the black areas and the right scan shows a haemorrhage indicated by the white areas.
<img src="/images/e/e5/Scans.jpg" _fck_mw_filename="Scans.jpg" _fck_mw_location="center" _fck_mw_width="500" _fck_mw_height="400" alt="" class="fck_mw_center" />
A stroke occurs every 3 minutes and 27 seconds in the UK, totalling approximately 152,000 strokes a year [26] . There is a high prevalence of stroke in Scotland due to the risk factors linked with the condition, including hypertension, smoking, inadequate exercise, high levels of alcohol consumption, and a poor diet. The Scottish Health survey 2014 revealed a shocking figure of 3.3% of males and 3.1% of females reported to have suffered from a stroke. In 2014/2015, 10,306 females and 10,310 males were discharged from hospital with stroke in Scotland. The percentage of stroke patients surviving 30 days or more after first emergency admission has improved very slightly from 81.6% in 2005/2006 to 84.9% in 2014/2015.[27] Scotland has the highest percentage of stroke survivors, meaning a large population of people requiring support and therapy post-stroke. This places addtitional stress on resources within NHS Scotland [28] .
<img src="/images/4/4f/Stroke_survivors_in_Scotland_2016.jpg" _fck_mw_filename="Stroke survivors in Scotland 2016.jpg" alt="" />
Within Lothian, it is estimated that there are 1,698 first or recurrent strokes per year, along with a further 340 people experiencing a transient ischemic attack, and 6,112 people living with stroke <span class="fck_mw_ref" _fck_mw_customtag="true" _fck_mw_tagname="ref" name="Lothian Improvement Plan" />.
NHS Stroke services[edit | edit source]
The NHS Physiotherapy waiting times, workforce and caseloads survey in the UK in 2010-2011 asked the question “Do you provide a stroke service?”. Sixty-seven respondents answered the question to show overall that 42% provided an inpatient stroke service, 34% did not provide any physiotherapy for stroke, 16% provided both community and inpatient stroke services, and 8% only provided a community stroke service.
The Scottish Stroke Care Audit 2015 [29] identified clear standards for stroke services in Scottish hospitals to achieve. Standard one states that at least 90% of stroke patients should be admitted to the stroke unit on the day they arrive or the day after. The table below shows the Scottish hospitals that did not meet standard one in 2014.
<img src="/images/6/63/HOSPITALS_2.jpg" _fck_mw_filename="HOSPITALS 2.jpg" _fck_mw_location="center" _fck_mw_width="500" _fck_mw_height="500" alt="" class="fck_mw_center" />A large systemic review of organised stroke unit care showed evidence to indicate that stroke patients have better clinical outcomes in terms of independence, survival, and returning home. Stroke Unit care can decrease the risk of death and disability following a stroke. Admission to a stroke unit is the optimum choice of treatment, however it is not always feasible due to Scotland’s geographically scattered population. Suspected stroke patients can often present to rural, remote hospitals which lack a stroke physician. Smaller hospital may have generic rehabilitation services rather than an organised stroke unit. Research favours a stroke specific ward over a general medical ward or mixed rehabilitation ward, with fewer patient deaths and less patients remaining dependent [30]
Deficits of neurological physiotherapy in the NHS[edit | edit source]
There are a number of key issues within neurological physiotherapy in Lothian that have been identified within the NHS Lothian Neurological Care Improvement Plan 2014-2017 <span class="fck_mw_ref" _fck_mw_customtag="true" _fck_mw_tagname="ref" name="Lothian Improvement Plan" />.
• Improvements need to be made with regards to accessibility, including inequality of access, problems of physical access and transport for people with more complex disabilities, lack of clear, identifiable pathways and possible duplication.
• There are currently only eight qualified neurological physiotherapists within Lothian. This service capacity needs to be increased.
• The quality of care needs to be more consistent, improving on the current situation of irregular bouts of excellent practice and expertise.
• Further encouragement needs to be provided to consider a single point of referral for neurological physiotherapy, which would supply information on demand.
A study conducted by <a href="http://europepmc.org/articles/PMC4802692">Verpillat et al 2015 </a> [31] examined the management of ischemic stroke in West Scotland. This study showed that out of 101 patients, 45.5% sought further physical therapy during the 1-year follow-up period. Often, within the NHS, the provision of physiotherapy is based on achieving goals within an expected timeframe. Unfortunately, if progress is limited, the continuation of physiotherapy may be questioned and focus may shift towards self management of the condition with less frequent physiotherapy sessions [32].
Do patients get enough therapy in hospital?[edit | edit source]
Rehabilitation is evidence based medicine utilised “to reach and maintain optimal functioning in physical, intellectual, psychological and/or social domains, according to the World Health Organisation <span class="fck_mw_ref" _fck_mw_customtag="true" _fck_mw_tagname="ref" name="International Classification of Functioning, Disability and Health:" />.
It has been recognised that many patients in stroke units feel they do not receive enough therapy during their hospital stay. The SSNAP <span class="fck_mw_ref" _fck_mw_customtag="true" _fck_mw_tagname="ref" name="How good is stroke care?:first SSNAP annual report" /> reported that physiotherapy is required by 85% of stroke patients. Despite this, patients who need physiotherapy only receive 32 minutes on average on just over 50% of their days in hospital. This is one of the NHS's downfalls as patients should be obtaining the equivalent of 45 minutes of physiotherapy per day for 5 days a week. These arethe opinions of stroke survivors regarding the care they received in the UK by the NHS in 2013-2014, highlighting some key areas of concern <span class="fck_mw_ref" _fck_mw_customtag="true" _fck_mw_tagname="ref" name="How good is stroke care?:first SSNAP annual report" />.
<img src="/images/thumb/a/a6/Quote_4.jpg/225px-Quote_4.jpg" _fck_mw_filename="Quote 4.jpg" _fck_mw_width="225" _fck_mw_height="225" alt="" /><img src="/images/thumb/5/51/Quote_6.jpg/250px-Quote_6.jpg" _fck_mw_filename="Quote 6.jpg" _fck_mw_width="250" _fck_mw_height="250" alt="" /><img src="/images/thumb/5/59/Quote_5.jpg/225px-Quote_5.jpg" _fck_mw_filename="Quote 5.jpg" _fck_mw_width="225" _fck_mw_height="225" alt="" />
<img src="/images/thumb/d/dc/Target_hours_of_physio.jpg/166px-Target_hours_of_physio.jpg" _fck_mw_filename="Target hours of physio.jpg" _fck_mw_location="left" _fck_mw_width="300" _fck_mw_height="300" alt="" class="fck_mw_left" />
The NHS does not have sufficient resources to provide long-term physiotherapy treatment for stroke survivors. Instead, the focus is placed on the initial period following a stroke. Pressure can be felt by patients within the hospital setting to reach targets fast in order to reach their recovery potential within a specified timeframe and some patients are led to believe that after 6 months, recovery stops. It is essential to know that stroke can potentially be a deteriorating condition as patients who do not continue treatment may become stiffer and less mobile. Also due to pressures on hospital beds, patients may get an early supported discharge with continuation of treatment at home <span class="fck_mw_ref" _fck_mw_customtag="true" _fck_mw_tagname="ref" name="Scottish stroke statistics" />, as shown in the illustration below. However, treatment at home may be delayed, reduced in intensity, and hence hinder recovery.
What happens when I transfer home?[edit | edit source]
<img src="/images/thumb/e/e3/What_happens_when_you_go_home.jpg/600px-What_happens_when_you_go_home.jpg" _fck_mw_filename="What happens when you go home.jpg" _fck_mw_width="600" _fck_mw_height="600" alt="" />
Early supported discharge can lead to better outcomes for patients, but <a href="https://www.strokeaudit.org/Documents/Results/National/Apr2014Mar2015/Apr2014Mar2015-AnnualReport.aspx">The Second SSNAP Annual Report[34]</a>, 2015 highlights certain areas in the UK where this service is unavailable, leaving patients isolated with limited therapy at home.
<img src="/images/0/05/Quote_3.jpg" _fck_mw_filename="Quote 3.jpg" _fck_mw_width="400" _fck_mw_height="400" alt="" />
Benefits of using private practice for stroke care[edit | edit source]
For the reasons highlighted above, having the option to go for physiotherapy for stroke care at a private practice can be of benefit to numerous people to eliminate pressures related to timescales and improve accessibility to therapy. Patients can receive a higher volume and frequency of therapy which is critical, especially in the early stages post stroke. Evidence shows that spontaneous recovery tends to occur mostly within the first 3 months [35]. Motor impairment is the focus for stroke rehabilitation of physiotherapists [36]. In the first 30 days following a stroke, the largest improvement in motor recovery occurs. However, significant progress is still seen up to 90 days’ post stroke in patients with more severe deficits [37] [38] [39]
Private neurological physiotherapy services in the UK have experienced significant improvements in the functioning levels of patients with a stroke beyond the first 6 months. Neurological physiotherapists re-educate the brain and body through movement that allow further progression in rehabilitation to be achieved [40]</div></div>
Parkinson's Disease[edit | edit source]
NHS Parkinson's disease care[edit | edit source]
Parkinson’s disease (PD) is the second most common neurological condition in the UK, affecting an estimated 127,000 people [41]. The NHS Lothian Neurological Care Improvement Plan 2014-2017 states that medical care alone is insufficient for this disease. In spite of this, patients with Parkinson’s disease frequently have no access to allied health professionals. The Edinburgh Parkinson’s Assessment Clinic (EPAC) is led by therapists to provide people diagnosed with Parkinson’s access to advice from a physiotherapist. However, the EPAC offers all newly diagnosed patients of parkinsonism a once-off assessment by a physiotherapist to provide education on self management. Following the initial assessment, there is no standardised pathway of care to therapeutic services. It has been highlighted that the NHS Lothian physiotherapist service needs specific PD staff training, an intranet page dedicated to Parkinson’s physiotherapy to improve communication between professionals, a system to review staff competencies in PD regularly, a system to review patient education throughout their journey frequently, and an evaluation of PD community exercise programmes <span class="fck_mw_ref" _fck_mw_customtag="true" _fck_mw_tagname="ref" name="Lothian Improvement Plan" />. Based on this information, the Lothian physiotherapist service for patients with PD is inadequate and requires improvements.
Physiotherapy aimed at rehabilitating patients with PD focuses on posture, upper limb function, transfers, balance, physical capacity, and gait. Supporting evidence in recent years for the inclusion of physiotherapy in the care of Parkinson’s disease has increased [42]. Management guidelines such as the <a href="https://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0008867/pdf/PubMedHealth_PMH0008867.pdf">National Collaborating Centre for Chronic Conditions: National clinical guidelines for diagnosis and management in primary and secondary care of Parkinson's disease</a> [43] and the <a href="http://onlinelibrary.wiley.com/store/10.1002/mds.21244/asset/21244_ftp.pdf?v=1&t=iv143vsw&s=93baac2479c4103cb2114bcf8151168c0f24ca54">Royal Dutch Society of Physical Therapy's practice recommendations </a>[44] have supported physiotherapy, leading to an increase in the number of referrals to physiotherapy. A systemic review and meta-analysis completed by Tomlinson et al. 2012 [45] showed that physiotherapy resulted in significant outcomes for gait speed, balance, and the unified Parkinson’s disease rating scale.
However, the 2015 UK Parkinson’s Audit [46] showed that only 50% of patients with PD are referred to a physiotherapist within two years of diagnosis, as shown in the table below.
<img src="/images/5/52/Time_between_diagnosis_and_physiotherapy_referral.jpg" _fck_mw_filename="Time between diagnosis and physiotherapy referral.jpg" _fck_mw_width="400" _fck_mw_height="400" alt="" />
This Patient Reported Experience Measure (PREM) collected the views from patients with PD and their carers regarding their PD service. There were a total of 5,835 people with and carers for PD who responded to the questionnaire. The pie chart below represents the quality of physiotherapy service offered <span class="fck_mw_ref" _fck_mw_customtag="true" _fck_mw_tagname="ref" name="Parkinson’s Audit Summary Report" />. The APPG launched an inquiry to examine the availability and quality of health and social care for patients with PD and their carers. This inquiry revealed evidence emphasising the benefits of early and ongoing access to therapy services including physiotherapy, which is less likely considering the two year wait to be referred to physiotherapy following diagnosis. A preventative approach to PD care is cost effective by reducing admissions to hospital and supporting patients in the community for an extended period of time. Unfortunately, evidence showed these interventions in many areas are unavailable until a later stage in the illness, which is too late or not at the frequency needed to be beneficial. For the limited amount of patients who received access to therapy services, some patients highlighted that they were only receiving short periods of therapy before being “signed off”, despite the long term requirement for support associated with the nature of the condition [47].
<img src="/images/1/14/Pie_chart.jpg" _fck_mw_filename="Pie chart.jpg" _fck_mw_location="center" _fck_mw_width="500" _fck_mw_height="500" alt="" class="fck_mw_center" />
Physiotherapist's role in PD care[edit | edit source]
Physiotherapists play a key role in the care of patients with PD. Physiotherapy is the most common non-drug treatment recommended for PD [48] [49] and physiotherapy is recommended by national guidelines as a mainstay of management. Some of the physiotherapists objectives are to improve the patient’s quality of life by increasing or maintaining the patients level of independence, wellbeing, and safety. These aims may be achieved by preventing falls and inactivity, reducing the patient’s activity limitation, and enhancing functional activity.
Parkinson’s disease can be divided into three phases, with the patient requiring physiotherapy in each phase. The early phase is characterised by little or no patient limitations. The physiotherapists goals are to prevent inactivity, prevent the fear to move or fall, and improving exercise capacity by providing information, advice, and exercise. The mid phase is recognised by balance issues, restrictions in performance of activities, and an increase fall risk. The therapeutic intervention is focused on body posture, gait, balance, reaching and grasping, and transfers. The late phase is identifiable by the patient’s confinement to a wheelchair or bed. The physiotherapist treating a patient in this phase is focused on preservation of vital functions and prevention of pressure sores and contractures.
The figure below is the International Classification of Functioning, Disability, and Health [50] associated with PD [51]
<img src="/images/f/f4/ICF_KASMA.jpg" _fck_mw_filename="ICF KASMA.jpg" _fck_mw_location="center" _fck_mw_width="700" _fck_mw_height="700" alt="" class="fck_mw_center" />
The impairments linked with PD that fall within the scope of physiotherapy are [52]
<img src="/images/5/5a/Table_6.jpg" _fck_mw_filename="Table 6.jpg" _fck_mw_width="600" _fck_mw_height="600" alt="" />
The ParkinsonNet model[edit | edit source]
Bloem and Munneke [53] recognised that PD is a condition where patients require long term support to manage, hence described the benefits of a model of integrated care incorporating a network of specialists. ParkinsonNet is a scheme established in the Netherlands to tackle problems such as inadequate interdisciplinary collaboration and communication, lack of specific training and expertise in PD, treatment focus on suppression of symptoms via drugs, and that referrals to allied health professionals such as physiotherapy being arbitrary. This model developed regional networks of inspiring, motivated, specialist health professionals to whom patients are referred for treatment long term <span class="fck_mw_ref" _fck_mw_customtag="true" _fck_mw_tagname="ref" name="Revolutionising management of chronic disease: the ParkinsonNet approach" />. Parkinson’s UK and the Parkinson’s service have been advocating the ParkinsonNet model, however as highlighted by the NHS Lothian Neurological Care Improvement Plan 2014-2017 <span class="fck_mw_ref" _fck_mw_customtag="true" _fck_mw_tagname="ref" name="Lothian Improvement Plan" />, this model has yet to be established in Scotland. In 2014, the Chair of the Lothian Parkinson’s Service Advisory Group, Dr Conor Maguire sought approval for the appointment of a Specialist Parkinson’s Physiotherapist to lead the development of a multidisciplinary model such as ParkinsonNet to help decrease geographical inequalities and standardise the provision of multidisciplinary care within Lothian. This process is ongoing currently <span class="fck_mw_ref" _fck_mw_customtag="true" _fck_mw_tagname="ref" name="Lothian Improvement Plan" />, meaning the patients with PD in Scotland are not receiving the benefits of this model.
How private physiotherapy can aid in the treatment of PD[edit | edit source]
Due to the long waiting period between diagnosis and referral to physiotherapy as highlighted in table 12 above, private physiotherapy can aid in reducing shortfalls in early therapeutic and preventative interventions.
<img src="/images/7/7f/Speech_bubble.jpg" _fck_mw_filename="Speech bubble.jpg" _fck_mw_location="right" _fck_mw_width="400" _fck_mw_height="400" alt="" class="fck_mw_right" />
Bhanu Ramaswamy, a consultant physiotherapist in Derbyshire, shared the significance of early referral to physiotherapy in the treatment of PD to help avoid complications such as falls. She reiterated the importance of early intervention stating: <span class="fck_mw_ref" _fck_mw_customtag="true" _fck_mw_tagname="ref" name="Please mind the gap:Parkinson’s disease services today" />
<img src="/images/0/0a/Quote_9.jpg" _fck_mw_filename="Quote 9.jpg" _fck_mw_location="left" _fck_mw_width="400" _fck_mw_height="400" alt="" class="fck_mw_left" />
Private physiotherapy can provide early intervention to delay the decline in a patient’s conditions and help maintain or improve a patient’s quality of life, confidence, and mobility. A person with PD responded to the APPG’s inquiry by saying <span class="fck_mw_ref" _fck_mw_customtag="true" _fck_mw_tagname="ref" name="Please mind the gap:Parkinson’s disease services today" />:
This patients experience with poor NHS accessibility highlights significant unmet needs. Private neurological physiotherapy can meet these needs providing early intervention following diagnosis, allowing patients to benefit from a preventative approach to care <span class="fck_mw_ref" _fck_mw_customtag="true" _fck_mw_tagname="ref" name="Please mind the gap:Parkinson’s disease services today" /> .
Overall benefits of private physiotherapy for Neurological Conditions.[edit | edit source]
Private UK neurological physiotherapy clinics such as <a href="http://neurolinkphysio.co.uk">Neurolink</a> [54] in London provide specialist physiotherapy for neurological conditions such as Stroke, Parkinson’s Disease, Traumatic Brain Injury, Multiple Sclerosis, and Spinal Cord Injury.
At Neurolink, the majority of clients attend x3 sessions a week, addressing issues proactively to prevent long term complications from developing. For progressive neurological conditions such as PD, the clinic aims to provide treatment and advice at each stage of the condition. A major benefit to private physiotherapy is on achievement of a client’s short term goals, focus shifts immediately to longer term maintenance and progression through a combination of neurophysiotherapy and the use of FES machines, neuro pilates, personal training, and massage therapy.
Many private clinics purchase state-of-the-art equipment. Neurolink uses a number of large Functional electrical stimulation machines including the RT-600 aimed at increasing the percentage weight bearing capacity of a client’s body through their legs, the RT-300 allowing for leg and/or arm cycling whilst seated, and the RT-200 providing arm and leg therapy and offering high cardiovascular demands. These machines are typically used with the aim of building up to daily 1 hour sessions. Neurolink also houses a five piece Integra wheelchair accessible gym, a five piece pilates equipment system, and a Medimotion leg bike <span class="fck_mw_ref" _fck_mw_customtag="true" _fck_mw_tagname="ref" name="NEUROLINK PHYSIOTHERAPY LTD" />. With longer and more frequent treatment sessions privately, patients can really experience benefits using advanced, up-to-date technology.
Following an interview with a physiotherapist treating neurological conditions in Edinburgh, it is clear that private physiotherapy for neurological conditions plays a pivotal role in helping clients achieve a threshold level of mobility and gain confidence and competence with exercise in order to support the transition to a local leisure club or community-based activity groups. The physiotherapist describes the role of a private physiotherapist, in addition to providing an incredible opportunity for improvement, is to help a client reflect on important outcomes from functional perspective to quality of life using careful documentation and involving family members. He believes this offers the client time to make a decision independently as to whether a change in functional status is possible and help shape their ideas about future management of their long term condition.
To quote an experienced physiotherapist in the field of neurological conditions:
<img src="/images/thumb/0/0d/Seans_quote.jpg/400px-Seans_quote.jpg" _fck_mw_filename="Seans quote.jpg" _fck_mw_location="right" _fck_mw_width="400" _fck_mw_height="400" alt="" class="fck_mw_right" />
This statement highlights the need for private physiotherapy to help neurological patients reach personal aspirations and higher goals, which take more time and effort to achieve.
Receiving regular physiotherapy not only improves patients physically, but also psychologically, building patient and family members confidence, positivity, hope, and belief. A private neurological physiotherapy clinic in California known as the <a href="http://challengecenter.org/about-us">Challenge Center</a>, [55]provides long term physiotherapy for neurological conditions for people who are no longer eligible to receive physiotherapy from the health system as they have reached their insurance coverage limit. For people who had run out of hope, this private physiotherapy clinic raises money through fundraisers to provide scholarships to clients needing continuous therapy. This scholarship is in addition to patients financing therapy independently. The video [56] below describes the physical and psychological benefits private physiotherapy brings to the lives of people with a neurological condition and their family members.
<img class="FCK__MWTemplate" src="http://www.physio-pedia.com/extensions/FCKeditor/fckeditor/editor/images/spacer.gif" _fckfakelement="true" _fckrealelement="6" _fck_mw_template="true">
Occupational Physiotherapy[edit | edit source]
Occupational Rehabilitation[edit | edit source]
Vocational or Occupational rehabilitation refers to the services that help enable an individual with a health problem to remain at or return to work by addressing barriers in psychological, functional, cognitive or emotional areas. The emphasis in this type of rehabilitation is on restoring functional abilities in order to work or to perform other occupation related activities rather than treating a specific clinical condition. There is strong evidence that sick absences and disability management services are cost effective with reduction in sick absence by 20-60% (Waddell et al 2008). Musculoskeletal disorders are a huge contributor to work related illness and absence from the work place. Musculoskeletal disorders make up one in eight approved absences from work and the average time on leave being 10 weeks (Addley et al, 2010). The estimated number of individuals within the UK who are impacted each year is 2 million with an estimated total of 40 million days of work missed (Addley et al, 2010). This equates to roughly 12 billion dollars per year in sickness and absence costs to the UK economy.
The Role of Physiotherapy
[edit | edit source]
Physiotherapists are particularly useful to employers and companies because of their skills and experience needed to perform workplace assessments to help identify and treat the potential cause of injury. Not only does this assist with treating an existing patient, but also with identifying the cause can help reduce the likelihood of another staff member in the same role being injured.
Physiotherapists are able to carry out a variety of tasks that can be beneficial for employers and employees, which include:
· Identifying probable cause of injury
· Developing safe and SMART orientated return to work programs including exercises to help with work conditioning
· Developing safe and realistic restrictions to prevent further injury when returning to work
· Reduce the likelihood of further injury by addressing areas such as posture, manual handling techniques, ergonomics and work place practices. (Physis, 2016)
There are also benefits to those who are sick or disabled to stay at work where health status permits which include:
Helps promote recovery within rehabilitation process
· Minimizes the side effects of long-term sickness absence, which can include physical, mental and social effects.
· Reduces long term incapacity
· Helps people feel like they contribute to society, maintain their independence and have autonomy.
· Improves quality of life (Getting vocational rehabilitation working for Scotland: education needs of staff supporting vocational rehabilitation 2008)
Specializing in Occupational Health and Ergonomic Physiotherapy[edit | edit source]
The ACPOHE is the Association of Chartered Physiotherapists in Occupational Health and Ergonomics, which is a professional network of physiotherapists within the CSP. The ACPOHE has physiotherapists who work within a variety of settings including the NHS, service industries, public and private sectors. The ACPOHE also works within retail, healthcare, offices and manufacturing environments. The association originated in 1947. In order to become a member of the ACPOHE a physiotherapist is required to demonstrate specific specialist competency in the area of Occupational health and Ergonomics. To achieve registered membership a physiotherapist must demonstrate development in occupational health by providing:
- Evidence of educational achievements
- Evidence of meeting level B on the ACPOHE OH competency framework
- Two professional references for work in occupational health and ergonomics
Achieving registered membership can be achieved in three different methods.
Educational achievement – completing a UK based masters level course that focuses on knowledge and skills in work and health. The course must be in ergonomics, occupational health and safety, vocational or occupational rehabilitation.
Short course – the ACPOHE offers 7 courses covering competencies in occupational health and ergonomics. Completing 4 of the 7 courses allows a member to apply for registered membership. All members following this route must complete introduction to occupational health and applied ergonomics and additionally two of the following:
- Office workstation ergonomics level 1
- Office workstation ergonomics level 2
- Assessing fitness for work and function
- Occupational rehabilitation and work hardening
- Communication for better outcomes: using a cognitive behavioural approach in occupational health
- Work relevant upper limb disorders; prevention and management
- Moving and handling; preventing injury and ill health at work
Case study assignment – this route is intended for full members of ACPOHE who have knowledge and skills through work and personal development without taking university accredited courses or ACPOHE courses. Two in depth case studies must be submitted with one in field of expertise and one in another area to prove knowledge across specialty.
For further information on obtaining registered membership please see the ACPOHE website.
Treatment Interventions
One of the main therapy tools occupational physiotherapists utilize are work hardening exercises that either simulate or mimic tasks that are functional and would normally be performed within an individual’s work setting. Work hardening exercise protocols utilize graded exercise progression to improve physical, psychological and emotional tolerance to exercise that will translate to improve work feasibility. In order to meet a work hardening exercise protocol, its components must address three key elements, which include:
· Exercises that chosen to help restore deficits in neurological, musculoskeletal or cardiopulmonary function
· Clearly stated intent to improve a patient’s work status
· Clearly stated connection between job demands and the intervention
Work hardening protocols can also include behavioral approaches, pain management and condition education along with return to work advice.
Oncology Physiotherapy[edit | edit source]
Oncology Physiotherapy
Respiratory Physiotherapy[edit | edit source]
Physiotherapists play an important role in relation to respiratory physiotherapy, covering a wide range of conditions. These range from chronic obstructive pulmonary disease (COPD) and cystic fibrosis, to intensive care and high dependency units in hospitals. The services of a respiratory physiotherapist can be utilized at any stage of the disease progression, ranging from early diagnosis through to care at the terminal stage.
Aims of Respiratory Physiotherapy[edit | edit source]
One of the main cornerstones of respiratory physiotherapy has been to aid in the removal of secretions. This area of physiotherapy has now developed to include a wide variety of different techniques to help problems associated with respiratory function, including:
• Maintaining/increasing exercise tolerance
• Reducing breathlessness and the work of breathing
• Educating the patient on their condition and improving their knowledge
• Improve their daily functional activities
<img src="/images/9/99/Stop_sign.jpeg" _fck_mw_filename="Stop sign.jpeg" alt="" /><img src="/images/b/bc/Time_2_reflect.png" _fck_mw_filename="Time 2 reflect.png" alt="" />
*** Reflection Questions ***
1. Does the role of a respiratory physiotherapist still interest me?
2. Do I want to further investigate if working in the private sector would interest me?
If you have answered "yes" to the above questions, continue reading below. If not return to the career pathway in the introduction section and select another specialty that may be of interest.
Prevalence of Lung Disease[edit | edit source]
Lung disease is believed to affect approximately 12.7 million people in the UK (British Lung Foundation) ranging from asthma, COPD and other long-term respiratory illnesses. COPD is the fifth leading cause of death in the UK, beaten only by cardiovascular disease and cancer [57]
<img src="/images/6/6c/British_Lung_Foundation_.jpeg" _fck_mw_filename="British Lung Foundation .jpeg" alt="" />
Figure 1: British Lung Foundation, viewed October 2016
Each year, lung diseases are responsible for a large number of hospital admissions. In 2011, 694,000 patients were admitted, with 6,120,400 bed-days due to lung disease (British Lung Foundation). Figure 1 demonstrates the different number of people diagnosed with lung disease compared to cardiovascular disease and cancer.
Research has suggested that the prevalence of lung disease in the UK is growing. For example, the diagnosis of COPD has increased by approximately 27% in the last 10 years, from under 1600 to 2000 people per 100,000 (British Lung Foundation). These figures demonstrate that lung disease is a potentially massive burden on the NHS, with interventions needed to address the treatment plans for these patients.
To read more on these figures, follow this link: https://statistics.blf.org.uk/
Pulmonary Rehabilitation[edit | edit source]
Pulmonary rehabilitation is a non-pharmacological program designed to help patients with chronic respiratory disease. There are numerous different components of this rehabilitation, such as exercise training, disease education and behavioral interventions [58]. It has been shown to significantly improve symptoms associated with chronic respiratory diseases, such as dyspnea, as well as increasing exercise capacity [59]
Pulmonary rehabilitation classes generally last from between 6-8 weeks, with 1-2 sessions a week. People
<img src="/images/thumb/5/51/Pulmonary_Rehab.jpg/180px-Pulmonary_Rehab.jpg" _fck_mw_filename="Pulmonary Rehab.jpg" _fck_mw_location="right" _fck_mw_type="thumb" alt="" class="fck_mw_frame fck_mw_right" />
Hospitalisation due to exacerbations of COPD cause the NHS a huge economic burden, with an annual cost of £810 to £930 million (British Thoracic Society, 2006). It results in 1.4 million GP visits a year, as well as 1 million bed days a year [60]. Pulmonary rehabilitation has been proven to help prevent flare ups of COPD, thus helping reduce the burden of these illnesses on the NHS.
Potential Barriers to Pulmonary Rehabilitation:[edit | edit source]
However, although there are obvious benefits associated with pulmonary rehabilitation, it is not without its downside. Due to the need to be referred to these classes, it increases the waiting time for the attendance of classes. Issues with patient compliance have also been documented. Attendance is as low as 50% [61], with 23-31% of patients failing to complete the course. Due to patients not showing up for classes, this prevents other patients from accessing this service, hindering them in their rehabilitation and increasing waiting list times for the classes.
<img src="/images/0/0d/Barriers_Image.jpg" _fck_mw_filename="Barriers Image.jpg" _fck_mw_location="left" _fck_mw_type="border" alt="" class="fck_mw_border fck_mw_left" />
A recent study highlighted a few problems associated with pulmonary rehabilitation classes provided by the NHS. Patient interviews drew attention to a number of different issues with these rehabilitation classes. Some found transport and parking to be an issue, whilst others found the timing of the classes and the day of the week to not suit them [62]. Accessing physiotherapy privately would offer them the opportunity to discuss other options with the physiotherapist, allowing patients more autonomy with the timing and location of their classes. As people may be working full time, this gives them the choice to obtain physiotherapy outside of their working hours, helping progress their rehabilitation.
Another possible barrier for attendance of these classes was the environment in which they were held, which can potentially be intimidating to patients. A study carried out by Hogg et al. discovered that being surrounded by fit and healthy people was disconcerting to people suffering from respiratory disease, with one patient quoted as saying:
<img src="/images/e/e7/Quote_1.jpg" _fck_mw_filename="Quote 1.jpg" _fck_mw_location="center" _fck_mw_type="border" alt="" class="fck_mw_border fck_mw_center" />If people were offered their own rehabilitation classes in a more private discreet setting, offering them the opportunity to feel comfortable in their surroundings, patient compliance with the programme could potentially increase.
As pulmonary rehabilitation classes generally only last between 6-8 weeks, patients aren’t able to avail of these services after the program has finished, instead relying on themselves to continue their exercises. It can be argued that if patients have enough motivation to proceed with these classes, thus increasing their quality of life and ability to carry out functional activities, they will be willing to pay the extra cost of the rehabilitation.
Another point of interest highlighted in the study by Hogg et al. showed that some participants were worried about carrying out their rehabilitation without the comforting presence of medical staff.
<img src="/images/1/1b/Quote_2.jpg" _fck_mw_filename="Quote 2.jpg" _fck_mw_location="center" _fck_mw_type="border" alt="" class="fck_mw_border fck_mw_center" />Without a doubt pulmonary rehabilitation classes provided by the NHS are an invaluable resource, but this extra comfort provided by physiotherapists after their course has concluded would encourage patients to continue in their rehabilitation and to not halt their progess.
What services are available at the moment?[edit | edit source]
The cost of private respiratory physiotherapy consultations and treatments range from £50 - £80 per treatment. There are a range of different respiratory physiotherapy services available in the private sector. For example, BUPA offer coverage for respiratory conditions ranging from pulmonary rehabilitation classes, hydrotherapy and pilates for breathing disorders.
By registering with the CSP website on the Physio2u page, respiratory physiotherapists can advertise their services to the public: http://www.csp.org.uk/your-health/find-physio/list-your-practice-physio2u
Health Considerations for Patients[edit | edit source]
As patients suffering from respiratory disease, they may have a wide range of different delibitating symptoms. It is important for physiotherapists to keep this in mind when treating their own patients. A service specification carried out by the NHS outlined a few recommendations for pulmonary rehabilitation. The healthcare provider running the classes must have knowledge of the diagnosis, recent spirometry results, relevent medical history, MRC dysponea score, oxygen saturation if possible, recent relevent clinical tests and drug management (Department of Health, 2012).
For more information regarding this service, including more comprehensive examinations, staffing and equipment, follow this link: /https://www.brit-thoracic.org.uk/document-library/clinical-information/pulmonary-rehabilitation/bts-guideline-for-pulmonary-rehabilitation/.
References[edit | edit source]
<span class="fck_mw_references" _fck_mw_customtag="true" _fck_mw_tagname="references" />
</div></div>
- ↑ Chartered Society of Physiotherapy. Physiotherapy Framework: putting physiotherapy behaviours, values, knowledge &amp; skills into practice. Chartered Society of Physiotherapy:2013. 40p. Available from: https://v3.pebblepad.co.uk/v3portfolio/csp/Asset/View/6jqbh3GzhGWrrcGqpknwmZzh8Z
- ↑ Higgs, J.,Refshauge, K., Ellis, E.. Portrait of the Physiotherapy Profession. Journal of Interprofessional Care. 2001; 15(1):79-89.
- ↑ World Confederation for Physical Therapy. Policy statement: Description of physical therapy. World Confederation for Physical Therapy: 2001. 12p. Available from: http://www.wcpt.org/policy/ps-descriptionPT
- ↑ World Confederation for Physical Therapy. Policy statement: Description of physical therapy. World Confederation for Physical Therapy: 2001. 12p. Available from: http://www.wcpt.org/policy/ps-descriptionPT
- ↑ World Confederation for Physical Therapy. Policy statement: Description of physical therapy. World Confederation for Physical Therapy: 2001. 12p. Available from: http://www.wcpt.org/policy/ps-descriptionPT
- ↑ JJ Consulting, Chartered Society of Physiotherapy. A survey of NHS Physiotherapy waiting times, workforce and caseloads in UK 2010-2011. London(UK): Chartered Society of Physiotherapy; 2011. 74p. Available from: http://www.csp.org.uk/publications/survey-nhs-physiotherapy-waiting-times-workforce-caseloads-uk-2010-2011
- ↑ JJ Consulting, Chartered Society of Physiotherapy. A survey of NHS Physiotherapy waiting times, workforce and caseloads in UK 2010-2011. London(UK): Chartered Society of Physiotherapy; 2011. 74p. Available from: http://www.csp.org.uk/publications/survey-nhs-physiotherapy-waiting-times-workforce-caseloads-uk-2010-2011
- ↑ JJ Consulting, Chartered Society of Physiotherapy. A survey of NHS Physiotherapy waiting times, workforce and caseloads in UK 2010-2011. London(UK): Chartered Society of Physiotherapy; 2011. 74p. Available from: http://www.csp.org.uk/publications/survey-nhs-physiotherapy-waiting-times-workforce-caseloads-uk-2010-2011
- ↑ JJ Consulting, Chartered Society of Physiotherapy. A survey of NHS Physiotherapy waiting times, workforce and caseloads in UK 2010-2011. London(UK): Chartered Society of Physiotherapy; 2011. 74p. Available from: http://www.csp.org.uk/publications/survey-nhs-physiotherapy-waiting-times-workforce-caseloads-uk-2010-2011
- ↑ JJ Consulting, Chartered Society of Physiotherapy. A survey of NHS Physiotherapy waiting times, workforce and caseloads in UK 2010-2011. London(UK): Chartered Society of Physiotherapy; 2011. 74p. Available from: http://www.csp.org.uk/publications/survey-nhs-physiotherapy-waiting-times-workforce-caseloads-uk-2010-2011
- ↑ Higgs, J.,Refshauge, K., Ellis, E.. Portrait of the Physiotherapy Profession. Journal of Interprofessional Care. 2001; 15(1):79-89.
- ↑ Canadian Physiotherapy Association. Description of Physiotherapy in Canada. Ottawa (CA): Canadian Physiotherapy Association; 2012. 17p. Available from: https://physiotherapy.ca/description-physiotherapy
- ↑ Canadian Physiotherapy Association. Description of Physiotherapy in Canada. Ottawa (CA): Canadian Physiotherapy Association; 2012. 17p. Available from: https://physiotherapy.ca/description-physiotherapy
- ↑ Neurological Alliance of Scotland. Neurological conditions factsheet. Available from: http://www.scottishneurological.org.uk/content/res/Neurological_Conditions_Factsheet.pdf (Accessed 31st October 2016).
- ↑ Neurological Physiotherapy Information Guide and Resource Centre. Neurological physiotherapy. Available from:http://neurologicalphysiotherapy.comfckLR(Accessed 31st October 2016).
- ↑ Neurological Physiotherapy Information Guide and Resource Centre. Neurological physiotherapy. Available from:http://neurologicalphysiotherapy.comfckLR(Accessed 31st October 2016).
- ↑ The Neurological Alliance. Neurological alliance neuro numbers. Available from: http://www.neural.org.uk/store/assets/files/381/original/Final_-_Neuro_Numbers_30_April_2014_.pdf (Accessed 23rd November 2016).
- ↑ National Health Service Quality Improvement Scotland. Neurological health services: Clinical standards. Available from: http://www.scottishneurological.org.uk/content/res/final_qis_standards.pdf (Accessed 23rd November 2016).
- ↑ The Neurological Alliance. The invisible patients: revealing the state of neurology services. Available from: http://www.neural.org.uk/store/assets/files/495/original/Invisible_patients_-_revealing_the_state_of_neurology_services_final_14_January_2015_.pdf (Accessed 31st October 2016).
- ↑ National Health Service Lothian. Lothian neurological care improvement plan 2014 to 2017. 2015. Available from: http://www.nhslothian.scot.nhs.uk/OurOrganisation/Strategies/Documents/NHS%20Lothian%20Neurological%20Care%20Improvement%20Plan%202014-2017%20-%20Final.pdf (Accessed 31st October 2016).
- ↑ National Health Service Lothian. Lothian neurological care improvement plan 2014 to 2017. 2015. Available from: http://www.nhslothian.scot.nhs.uk/OurOrganisation/Strategies/Documents/NHS%20Lothian%20Neurological%20Care%20Improvement%20Plan%202014-2017%20-%20Final.pdf (Accessed 31st October 2016).
- ↑ Sue Ryder. Public fear getting a neurological condition. Available from: http://www.sueryder.org/media-centre/news/2016/june/public%20fear%20getting%20a%20neurological%20disorder (Accessed 28th October 2016).
- ↑ Department of Health. The national service framework for longterm conditions. 2005. Leeds: NSF. Available from: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/198114/National_Service_Framework_for_Long_Term_Conditions.pdf (Accessed 23rd November 2016).
- ↑ JJ Consulting. A survey of NHS Physiotherapy waiting times, workforce and caseloads in the UK 2010-2011. London: CSP; 2011 Available from: http://www.csp.org.uk/publications/survey-nhs-physiotherapy-waiting-times-workforce-caseloads-uk-2010-2011 (Accessed 11th November 2016).
- ↑ Department of Health. Liberating the NHS:No decision about me, without me. London:NHS; 2012. Available from: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/216980/Liberating-the-NHS-No-decision-about-me-without-me-Government-response.pdf (Accessed 1st November 2016).
- ↑ Stroke Association. State of the nation: stroke statistics; 2016. Available from: https://www.stroke.org.uk/sites/default/files/stroke_statistics_2015.pdf (viewed 1st November 2016)
- ↑ National Health Service Scotland. Scottish stroke statistics. 2016. Available from: https://www.isdscotland.org/Health-Topics/Stroke/Publications/2016-01-26/2016-01-26-Stroke-Report.pdf (viewed 1st November 2016)
- ↑ STROKE ASSOCIATION., 2016. State of the nation: stroke statistics [online]. [viewed 1 November 2016]. Available from: https://www.stroke.org.uk/sites/default/files/stroke_statistics_2015.pdf
- ↑ National Health Service Scotland. Scottish stroke care audit: public summary of 2015 national report. Edinburgh: ISD Scotland Publications; 2015. Available from: http://www.strokeaudit.scot.nhs.uk/Downloads/2015_report/SSCA-summary-2015-web.pdf (Accessed 1st November 2016)
- ↑ Scottish Intercollegiate Guidelines Network. Management of patients with stroke: Rehabilitation, prevention and management of complications, and discharge planning. Edinburgh:SIGN; 2010. Available from: http://www.sign.ac.uk/pdf/sign118.pdf ( Accessed 24th November 2016).
- ↑ Verpillat, P., Dorey, J., Guilhaume-Goulant, C., Dabbous, F., and Aballea, S. Ischemic stroke management in West Scotland a chart review. Journal of market access and health policy [Internet]. 2015 September, vol. 3. Available from: http://europepmc.org/articles/PMC4802692 (Accessed 1st November 2016).
- ↑ Ashford and St Peter's hospitals NHS foundation trust. Physiotherapy for stroke patients. Available from: http://www.ashfordstpeters.nhs.uk/physiotherapy-for-stroke-patients. (Accessed 2nd November 2016).
- ↑ ROYAL COLLEGE OF PHYSICIANS., 2014. How good is stroke care?:first SSNAP annual report [online]. London: SSNAP. pp. 1-39. [viewed 2 November 2016]. Available from: https://www.strokeaudit.org/Documents/Newspress/SSNAP-Annual-Report-(April-2013-March-2014).pdf
- ↑ ROYAL COLLEGE OF PHYSICIANS., 2015. The second SSNAP annual report: Is stroke care improving?[online]. London: SSNAP.pp. 1-30. [viewed 2 November 2016]. Available from: https://www.strokeaudit.org/Documents/Results/National/Apr2014Mar2015/Apr2014Mar2015-AnnualReport.aspx
- ↑ KRAKAUER, JW.,CARMICHAEL, ST., CORBETT,D. and WITTENBERG, GF., 2012. Getting neurorehabilitation right: what can be learned from animal models? Neurorehabilitation and Neural Repair. vol. 26, pp. 923–931.
- ↑ LANGHORNE, P., COUPAR, F. and POLLOCK, A., 2009. Motor recovery after stroke: a systematic review. The Lancet Neurology. vol. 8, pp. 741–754.
- ↑ DUNCAN, PW., GOLDSTEIN, LB., MATCHAR, D., DIVINE, GW. and FEUSSNER, J., 1992. Measurement of motor recovery after stroke. Outcome assessment and sample size requirements. Stroke [online]. August, vol. 23, no. 8, pp. 1084–1089. [viewed 3 November 2016]. Available from: http://stroke.ahajournals.org/content/23/8/1084.long
- ↑ DUNCAN, PW., GOLDSTEIN, LB., HORNER, RD., LANDSMAN, PB., SAMSA, GP. and MATCHAR, D., 1994. Similar motor recovery of upper and lower extremities after stroke. Stroke [online]. June, vol. 25, no. 6, pp. 1181–1188. [viewed 3 November 2016]. Available from: http://stroke.ahajournals.org/content/25/6/1181
- ↑ DUNCAN, PW., ZOROWITZ, R., BATES, B., CHOI, JY., GLASBERG, JJ., GRAHAM, GD., KATZ, RC., LAMBERTY, K. and REKER, D., 2005. Management of adult stroke rehabilitation care: a clinical practice guideline. Stroke [online]. September, vol. 36, no. 9, pp. 100-143. [viewed 3 November 2016] Available from: http://stroke.ahajournals.org/content/36/9/e100.full
- ↑ HEADS UP NEURO REHAB LTD., 2016. Neurological physiotherapy for long term strokes [online].[viewed 2 November 2016] Available from: http://headsup.co.uk/neurological-physiotherapy-for-long-term-strokes/
- ↑ NHS CHOICES., 2016. Parkinson's disease [online]. [viewed 2 November 2016]. Available from: https://www.parkinsons.org.uk/sites/default/files/appg_report_please_mind_the_gap.pdf
- ↑ KEUS, SH., MUNNEKE, M., NIJKRAKE, MJ., KWAKKEL, G.and BLOEM, BR., 2009. Physical therapy in Parkinson's disease: evolution and future challenges. Movement Disorders. vol. 24, no. 1, pp. 1-14.
- ↑ THE NATIONAL COLLABORATING CENTRE FOR CHRONIC CONDITIONS., 2006. Parkinson’s disease: national clinical guideline for diagnosis and management in primary and secondary care [online]. London: Royal College of Physicians. pp. 1-534. [viewed 2 November 2016]. Available from: https://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0008867/pdf/PubMedHealth_PMH0008867.pdf
- ↑ KEUS, SH., BLOEM, BR., HENDRIKS, EJ., BREDERO-COHEN, AB. and MUNNEKE, M., 2007. Evidence-based analysis of physical therapy in Parkinson’s disease with recommendations for practice and research. Movement Disorders [online]. November, vol. 22, no. 4, pp. 451-460. [viewed 2 November 2016]. Available from: http://onlinelibrary.wiley.com/doi/10.1002/mds.21244/epdf
- ↑ TOMLINSON, C., PATEL, S., MEEK, C., HERD, C., CLARKE, C., STOWE, R., SHAH, L., SACKLEY, C., O DEANE, K., WHEATLEY, K. and IVES, N., 2012. Physiotherapy intervention in Parkinson’s disease: systematic review and meta-analysis. BMJ [online]. August, vol. 345, pp. 1-14. [viewed 2 November 2016]. Available from: http://www.bmj.com/content/bmj/345/bmj.e5004.full.pdf
- ↑ UK PARKINSON'S EXCELLENCE NETWORK., 2015. 2015 UK Parkinson’s Audit Summary Report [online]. London:UK Parkinson's. pp. 1-43. [viewed 2 November 2016]. Available from: https://www.parkinsons.org.uk/sites/default/files/audit2015_summaryreport.pdf
- ↑ ALL PARTY PARLIAMENTARY GROUP FOR PARKINSON'S DISEASE., 2009. Please mind the gap:Parkinson’s disease services today [online]. pp. 1-40. [viewed 2 November 2016]. Available from: https://www.parkinsons.org.uk/sites/default/files/appg_report_please_mind_the_gap.pdf
- ↑ KEUS, SH., BLOEM, BR., VERBAAN, D., DE JONGE, PA., HOFMAN, M., VAN HILTEN, BJ. and MUNNEKE, M., 2004. Physiotherapy in Parkinson’s disease: utilisation and patient satisfaction. Journal of Neurology [online]. June, vol. 251, no. 6, pp. 680-687.
- ↑ STOCCHI, F. and BLOEM, BR., 2013. Move for change part II: a European survey evaluating the impact of the EPDA Charter for people with Parkinson’s disease. European Journal of Neurology [online]. March, vol. 20, no. 3, pp. 461-472 [viewed 29 October 2016]. Available from: http://onlinelibrary.wiley.com/doi/10.1111/j.1468-1331.2012.03876.x/epdf
- ↑ World Health Organization, 2001. International Classification of Functioning, Disability and Health: ICF. World Health Organization.
- ↑ KAMSMA, YPT., 2002, Functional reorganisation of basic motor actions in Parkinson's disease: problem analysis, development and evaluation of a compensatory strategy training. Groningen.
- ↑ KNGF., 2004. Guidelines for physical therapy in patients with Parkinson’s disease [online]. Netherlands: Royal Dutch Society for Physiotherapy. pp. 1-86. [viewed 29 October 2016]. Available from: http://www.appde.eu/pdfs/Dutch%20Parkinson's%20Physiotherapy%20Guidelines.pdf
- ↑ BLOEM, B. and MUNNEKE, M., 2014. Revolutionising management of chronic disease: the ParkinsonNet approach. BMJ [online]. vol. 348, pp. 1-8 [viewed 29 October 2016]. Available from: http://www.west-info.eu/files/Revolutionising-management-of-chronic-disease_-the-ParkinsonNet-approach-_-BMJ.pdf
- ↑ NEUROLINK PHYSIOTHERAPY LTD., 2016. Specialist neurological physiotherapy clinic: enable enhance empower-unlock your potential [online]. [viewed 3 November 2016]. Available from: http://neurolinkphysio.co.uk/index.html
- ↑ CHALLENGE CENTER., 2011. About us [online]. [viewed 3 November 2016]. Available from: http://challengecenter.org/about-us
- ↑ CHALLENGE CENTER., 2015. Challenge center video 2014 [online video]. California: Challenge Center. [viewed 3 November 2016]. Available from: https://www.youtube.com/watch?v=TDGETLa4Bm8
- ↑ Masoli, M., Fabian, D., Holt, S. and Beasley, R. (2004). The global burden of asthma: executive summary of the GINA Dissemination Committee Report. Allergy, 59(5), pp.469-478.
- ↑ Hayton, C., Clark, A., Olive, S., Browne, P., Galey, P., Knights, E., Staunton, L., Jones, A., Coombes, E. and Wilson, A. (2013). Barriers to pulmonary rehabilitation: Characteristics that predict patient attendance and adherence. Respiratory Medicine, 107(3), pp.401-407.
- ↑ Nici, L., Donner, C., Wouters, E., Zuwallack, R., Ambrosino, N., Bourbeau, J., Carone, M., Celli, B., Engelen, M., Fahy, B., Garvey, C., Goldstein, R., Gosselink, R., Lareau, S., MacIntyre, N., Maltais, F., Morgan, M., O'Donnell, D., Prefault, C., Reardon, J., Rochester, C., Schols, A., Singh, S. and Troosters, T. (2006). American Thoracic Society/European Respiratory Society Statement on Pulmonary Rehabilitation. American Journal of Respiratory and Critical Care Medicine, 173(12), pp.1390-1413.
- ↑ Hayton, C., Clark, A., Olive, S., Browne, P., Galey, P., Knights, E., Staunton, L., Jones, A., Coombes, E. and Wilson, A. (2013). Barriers to pulmonary rehabilitation: Characteristics that predict patient attendance and adherence. Respiratory Medicine, 107(3), pp.401-407.
- ↑ Keating, A., Lee, A. and Holland, A. (2011). What prevents people with chronic obstructive pulmonary disease from attending pulmonary rehabilitation? A systematic review. Chron Respir Dis, 8(2), pp.89-99.
- ↑ de Sousa Pinto, J., Martin-Nogueras, A., Morano, M., Macedo, T., Arenillas, J. and Troosters, T. (2013). Chronic obstructive pulmonary disease patients' experience with pulmonary rehabilitation: A systematic review of qualitative research. Chronic Respiratory Disease, 10(3), pp.141-157.