Defining the Evidence Based Practice Decision-Making Model
This article or area is currently under construction and may only be partially complete. Please come back soon to see the finished work! (27/10/2023)
Original Editor - Wanda van Niekerk
Top Contributors - Wanda van Niekerk, Jess Bell and Angeliki Chorti
Introduction[edit | edit source]
Evidence-based practice (EBP) was first introduced in the early 1990's as evidence-based medicine (EBM). [1] This “new paradigm” initially involved the practice of clinical medicine with the aim to develop and advance a transparent and rational process for clinical decision-making that did not exclusively rely on intuition and single clinical expertise and can be taught, refined, and applied by all clinicians. [2] Since then, various models and frameworks have been proposed in the healthcare setting that do not apply to the field of medicine only. [3]
Revised Model of Evidence Based Practice[edit | edit source]
Read more about the first models of evidence based practice from Sackett et al. and Haynes et al.: Introduction and Overview of Evidence Based Practice
Satterfield et al. in 2009 [2] further developed the evidence-based practice model and provided it with a transdisciplinary perspective by adding each discipline's efforts towards addressing deficiencies and making advances. The aim was to provide a common language across disciplines. This model had a new external frame that provided environmental and organisational context. The three inner pillars of the model involved the best available research evidence, client or population’s characteristics, state, needs, values and preferences and resources including practitioner’s expertise. At the centre of this evidence-based model was clinical decision-making, giving clinical expertise a key role in the EBP decision-making process. [4]
EBP Steps[edit | edit source]
Step 1: Determining the patient’s needs to formulate a clinical question
Step 2: Locating the knowledge resources
Step 3: Appraising the quality of the knowledge resources
Step 4: Discussing the options with the patient
Step 5: Formulate the treatment plan
Step 6: Implementing the treatment plan
Step 7: Evaluate the effectiveness of the treatment plan and the evidence-based practice process
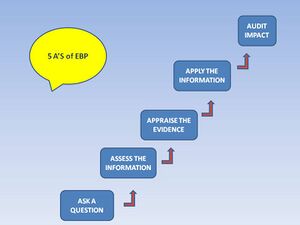
5 A’S of EBP[edit | edit source]
Evidence-based practice is a 5-step process that is commonly refered to as the five ‘A’s: Ask, Access, Appraise, Apply, Audit.
Terminology[edit | edit source]
Evidence-based treatment
Best practice
Research-informed practice
Evidence-based practice applications
And link to page
Challenges of EBP[edit | edit source]
Lack of time to search for and apply the best available evidence – mostly due to heavy patient case loads. [5]
Not enough or not good enough research available on all conditions and scenarios. [6]
Finding the right resources between the masses is difficult H, Tabrizi JS, Azami‐Aghdash S. Barriers to evidence‐based medicine: a systematic review. Journal of evaluation in clinical practice. 2014 Dec;20(6):793-802.
Accessing the resources Ibikunle PO, Onwuakagba IU, Maduka EU, Okoye EC, Umunna JO. Perceived barriers to evidence‐based practice in stroke management among physiotherapists in a developing country. Journal of Evaluation in Clinical Practice. 2021 Apr;27(2):291-306.
Lack of administrative support Naghibi et al
Not skilled in critical appraisal Naghibi
Not enough role models who practice evidence-based practice regularly
Advantages
It offers the surest and most objective way to determine and maintain consistently
high quality and safety standards in medical practice.
It can help speed up the process of transferring clinical research findings into
practice.
It has the potential to reduce healthcare costs significantly.”
Reduce variability of care
Increases healthcare provider empowerment and role satisfaction
Meets expectations of an informed public
Resources[edit | edit source]
- bulleted list
- x
or
- numbered list
- x
References[edit | edit source]
- ↑ Evidence-Based Medicine Working Group. Evidence-based medicine. A new approach to teaching the practice of medicine. JAMA. 1992 Nov 4;268(17):2420-5.
- ↑ 2.0 2.1 Satterfield J, Spring B, Brownson R, Mullen E, Newhouse R, Walker B, Whitlock E. Toward a Transdisciplinary Model of Evidence-Based Practice. Milbank Q. 2009 Jun; 87(2): 368–390.
- ↑ Dusin J, Melanson A, Mische-Lawson L. Evidence-based practice models and frameworks in the healthcare setting: a scoping review. BMJ Open. 2023; 13(5): e071188.
- ↑ Haynes RB, Devereaux PJ, Guyatt GH. Clinical expertise in the era of evidence-based medicine and patient choice. ACP J Club. 2002 Mar-Apr;136(2):A11-4.
- ↑ Naghibi D, Mohammadzadeh S, Azami-Aghdash S. Barriers to evidence-based practice in health system: a systematic review. Evidence Based Care. 2021 Jul 1;11(2):74-82.
- ↑ Sadeghi-Bazargani H, Tabrizi JS, Azami-Aghdash S. Barriers to evidence-based medicine: a systematic review. J Eval Clin Pract. 2014 Dec;20(6):793-802.