Cushing's Syndrome Case Study
Author/s[edit | edit source]
Chris Hartlage, Braden Hurst, Lee Janasek, Michael Porter and Jordan Thomas from the Bellarmine University Physical Therapy Program's Pathophysiology of Complex Patient Problems Project.
Abstract[edit | edit source]
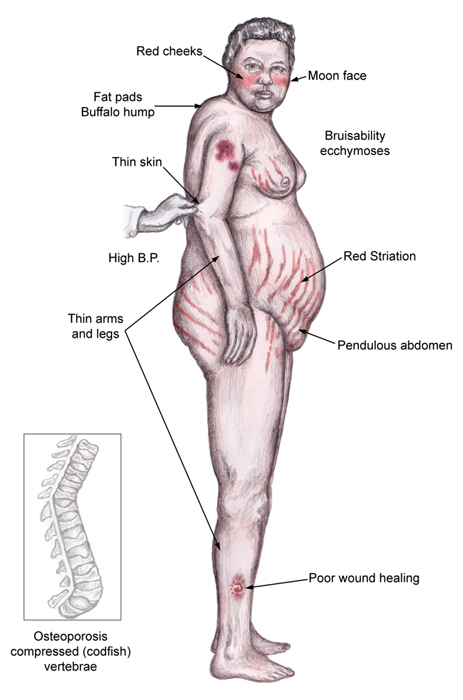
Cushing’s syndrome occurs when your body is exposed to high levels of cortisol for a long period of time.[1][2] It is an extremely rare disease in children, with a peak in adults in the third or fourth decade. The most common cause of Cushing’s syndrome is the use of oral corticosteroid medication.[1][2] Common signs and symptoms include weight gain and fatty tissue deposits in the abdomen, face, and between the shoulders.[1][2] Other signs/symptoms include hypertension, back pain, proximal muscle weakness, fragile skin that bruises easily, and thinning hair. [1][2][3]
Patient Characteristics[edit | edit source]
- Demographics: Patient is a 33 year old Caucasian female who is a middle school teacher.
- Medical diagnoses: Asthma, Bursitis
- Co-morbidities: Obese, Hypertension, Type II Diabetes
- Previous treatments: Insulin pump for Diabetes, Corticosteroid use for the past 7 years for asthma, Hypertension medication, Physical therapy for treatment of hip bursitis
Examination[edit | edit source]
- Subjective: Tracey Smith reports to Function First for general muscle weakness and low back pain. She has been having low back pain for a little over 4 months now. On a scale of 1-10, her pain at best is a 3 and at worst is a 7. The general muscle weakness has been getting progressively worse over the past month and is beginning to concern her. Mrs. Smith also reports having trouble making it through her Zumba class on Tuesday’s and Thursday’s. She says lately she has little interest in her regular activities and has been experiencing fatigue without physical exertion. Patient was diagnosed with type II Diabetes in her late 20’s and has been taking insulin regularly since her diagnosis. Mrs. Smith has also been experiencing headaches more frequently at night over the past few weeks. She was treated at Function First in 2013 for hip pain secondary to bursitis. After 4 weeks of conservative treatment, Mrs. Smith’s pain was still present and she was referred to her back to her primary care physician where he administered multiple corticosteroid injections. Patient also reports she has been taking inhaled corticosteroids for the past 10 years. Lastly, Mrs. Smith reports having irregular menstrual cycles for the past 2 years accompanied by unexplained weight gain in her abdomen.
- Goals: Patient would like to have little to no back pain. Patient also would like to be able to increase her strength and endurance in able to resume her normal Zumba classes twice a week.
- Self Report Outcome Measures: ODI, FABQ, SANE
- Physical Performance Measures: 6 min walk
Clinical Impression[edit | edit source]
Summarization of Examination Findings[edit | edit source]
Patient displays proximal muscle weakness, obesity, low back pain, signs of fatigue, and generalized decrease in thoracic and lumbar ROM. Aerobic exercise will be implemented to address weight loss and muscular endurance. A strengthening program will also be implemented to address the proximal muscle weakness, low back pain and fatigue. Manual therapy will also be added to increase mobility of the lumbar spine and decrease the pain she is experiencing.
Interventions[edit | edit source]
Outcomes[edit | edit source]
Discussion[edit | edit source]
Summary Statement which should include related findings in the literature, potential impact on clinical practices
Related Pages[edit | edit source]
Cushing’s syndrome: http://www.physio-pedia.com/Cushing%27s_Syndrome
Cushing’s syndrome support website: http://www.cushings-help.com/cushing-causes.htm
Society for Endocrinology: http://www.endocrinology.org/
References[edit | edit source]
References will automatically be added here, see adding references tutorial.
- ↑ 1.0 1.1 1.2 1.3 Cushing’s Syndrome: Mayo Clinic Diseases and Conditions. http://www.mayoclinic.org/diseases-conditions/cushing-syndrome/basics/definition/con-20032115. Published 2013. Accessed March 21, 2015.
- ↑ 2.0 2.1 2.2 2.3 Cushing’s Syndrome: MedLine Plus. http://www.nlm.nih.gov/medlineplus/cushingssyndrome.html. Updated September 25, 2014. Accessed March 21, 2015.
- ↑ Ensor, W. Endocrine and Metabolic Disorders. [PowerPoint]. Louisville, KY: Bellarmine University DPT Program; 2015.
- ↑ Cushing’s Syndrome: Medscape. http://emedicine.medscape.com/article/117365-overview. Updated April 4, 2014. Accesse March 21, 2015.