Critical Illness Polyneuropathy (CIP): Difference between revisions
No edit summary |
No edit summary |
||
| Line 58: | Line 58: | ||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
Medical Research Council (MRC) | |||
Electromyography | |||
Biopsy | |||
<br> | <br> | ||
Revision as of 12:04, 13 June 2018
Original Editor - Your name will be added here if you created the original content for this page.
Lead Editors
Definition
[edit | edit source]
Critical Illness Polyneuropathy (CIP) is one of three classifications of Intensive care -unit acquired weakness (ICUAW), the others being Critical Illness Myopathy (CIM) and Critical Illness Neuromyopathy (CINM)[1]. ICUAW is defined as 'a clinically detected weakness in critically ill patients in whom there is no plausable aetiology other than critical illness' [2]
Clinically Relevant Anatomy
[edit | edit source]
Pathological Process[edit | edit source]
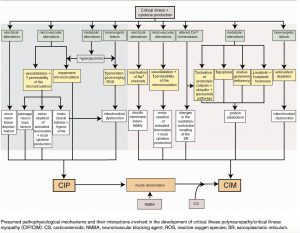
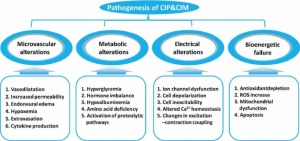
The pathophysiology for CIP remains unclear and complex, with human studies highlighting axonal degeneration [3].It has been thought that the mechanism may involve:
- Microvascular alterations: Increase in E- Selectin expression, vasodilation, increased capillary permeability, extravasation and endoneural oedema which results in hypoxia.
- Metabolic alterations: Production of toxic factors such as cytokines, hyperglycaemia, hormone imbalance, hypoalbuminemia, amina acid deficiency and activation of proteolytic pathways.
- Electrical alterations: Ion channel dysfunction, cell depolarisation, inexcitability, altered calcium homeostasis and changes in excitation-contraction coupling.
- Bionenergetic failure: Anti-oxident depletion, an increase in reactive oxygen species, mitochrondial dysfunction and apoptosis.
Risk Factors
- Sepsis
- SIRS
- Multi Organ Failure (MOF)
- Female Gender
- Duration of Organ Dysfunction
- Duration of ICU Stay
- Ionotropic Support
- Renal Failure
- Low Serum Albumin
- Hyperglycemia
- Neuromuscular Blockades
- Corticosteroids
Clinical Presentation[edit | edit source]
Visser (2006) [4] reports that the clinical features of CIP typically include:
- Muscle Weakness: Predominantly in the lower extremities. This should be suspected if there is reduced limb movement following a painful stimulus to the distal limb. Flaccid weakness can be observed symmetrically.
- Absent Facial Weakness: Cranial nerves are rarely affected.
- Muscle Wasting: Observed in one third of patients
- Reduced Muscle Reflexes: Reflexes are usually present at the start of the disease, but decrease over time.
- Difficulty in Weaning from Ventillator
- Sensory Loss: Although difficult to assess with a sedated or intubated patient.
- Impaired Consciousness: Suggested of an encephalopathy is also usually present
Diagnostic Procedures[edit | edit source]
Medical Research Council (MRC)
Electromyography
Biopsy
Outcome Measures[edit | edit source]
add links to outcome measures here (see Outcome Measures Database)
Management / Interventions
[edit | edit source]
add text here relating to management approaches to the condition
Differential Diagnosis
[edit | edit source]
add text here relating to the differential diagnosis of this condition
Resources
[edit | edit source]
add appropriate resources here
References[edit | edit source]
- ↑ Appleton, R. and Kinsella, J., 2012. Intensive care unit-acquired weakness. Continuing Education in Anaesthesia, Critical Care and Pain, 12(2), pp.62-66.
- ↑ Stevens, R.D., Marshall, S.A., Cornblath, D.R., Hoke, A., Needham, D.M., de Jonghe, B., Ali, N.A. and Sharshar, T., 2009. A framework for diagnosing and classifying intensive care unit-acquired weakness. Critical care medicine, 37(10), pp.S299-S308.
- ↑ Zhou, C., Wu, L., Ni, F., Ji, W., Wu, J. and Zhang, H., 2014. Critical illness polyneuropathy and myopathy: a systematic review. Neural regeneration research, 9(1), p.101.
- ↑ Visser, L.H., 2006. Critical illness polyneuropathy and myopathy: clinical features, risk factors and prognosis. European journal of neurology, 13(11), pp.1203-1212.