Colorectal Cancer: Difference between revisions
No edit summary |
No edit summary |
||
| Line 57: | Line 57: | ||
*Diabetes | *Diabetes | ||
[[Image:CoMorbidities.png]] | [[Image:CoMorbidities.png]]<ref name="DeM">De Marco MF, Janssen-Heijnen ML, Van Der Heijden LH, et al. Comorbidity and colorectal cancer according to subsite and stage: a population-based study. Eur J Cancer. 2000 Jan; 36(1): 95-9</ref> | ||
== Medications == | == Medications == | ||
Revision as of 20:06, 14 February 2013
Original Editors - Jacqueline Lopez & Abby Schnur from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Lead Editors - Your name will be added here if you are a lead editor on this page. Read more.
Definition/Description[edit | edit source]
Colorectal cancer (CRC) is a rapid abnormal cell growth that affects the large intestines and/or rectum. These clusters of cells are called adenomatous polyps and develop from the tissue membrane of glandular tissue. Polyps can start as benign and non-cancerous but with time can develop and become cancerous.
Prevalence
[edit | edit source]
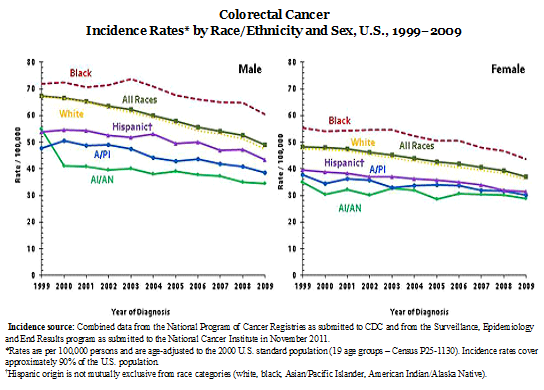
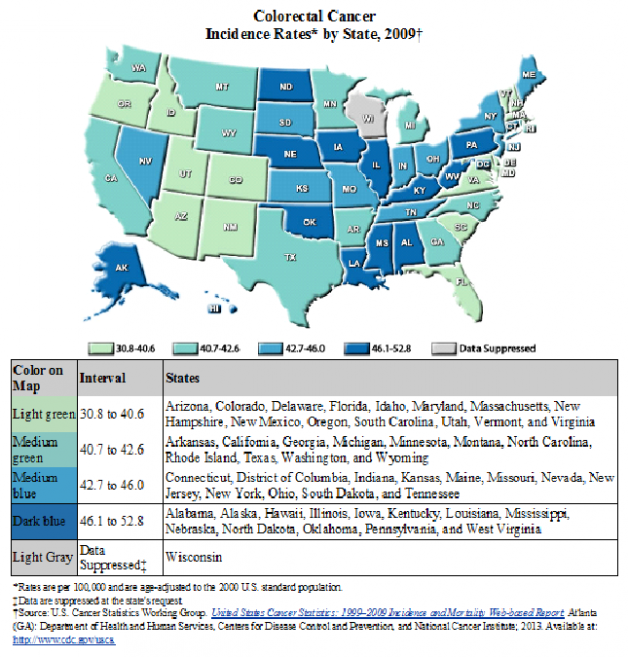
Colorectal cancer is the second leading cause of death from a type of cancer in the United States. It is also the third most common cancer among men and women. The most current statistics report 136,717 people were diagnosed in 2009 with colorectal cancer (51.26% male and 48.63% female) and 51,848 deaths (51.7% male and 48.3% female) according to the Center of Disease Control.
Data from 2009 provided by the National Cancer Institute showed that prior to January 1, 2009 1,140,161 people were living with a diagnosis of CRC in the United States. This number includes people both, currently seeking treatment for their active diagnosis, as well as, individuals who have been in years of remission. 558,648 of these individuals were male and 581,477 were female.
Other statistical facts gathered from various sources include the following:
- The lifetime risk of developing CRC is 1/20 or 4.96%.[1]
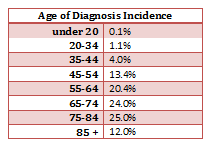
- The mean age of CRC diagnosis is 69 years of age. [2]
- The mean mortality age of CRC is 74 years of age. [2]
- Studies between 1991 and 2005 show that survival rates from CRC have increased by 30%. [3]
- The risk of getting CRC increases with age and is greater in men than women. [4]
- The most common area of diagnosis is the rectum and the rectosigmoid junction, with the sigmoid resulting the most favorable outcome. [5]
Characteristics/Clinical Presentation[edit | edit source]
Colorectal cancer can present as asymptomatic and symptomatic. Asymptomatic patients are diagnosed with a fecal occult blood test are identified at an early stage and most commonly located in the cecum/ascending colon.
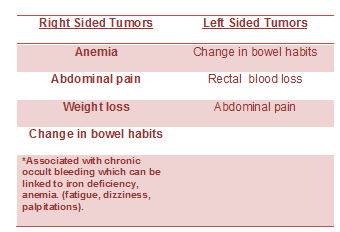
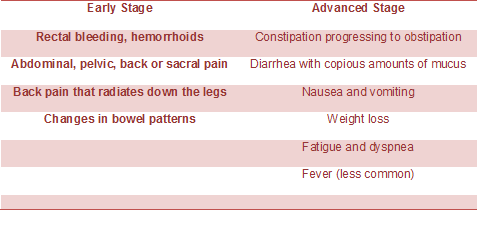
Symptoms differ depending on where the tumor is located.
A diagnosis is made by a Colorectal Cancer screening examination or through an evaluation for an unrelated illness.
Associated Co-morbidities[edit | edit source]
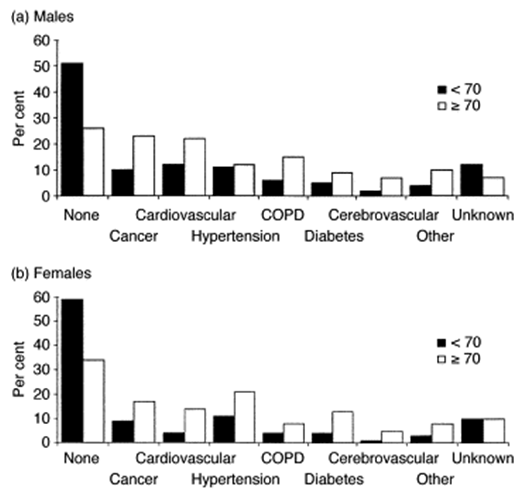
Approximately 51-59% of individuals with a diagnosis of CRC who are under the age of 70 do not also suffer from co-morbidities; however, in the individuals who are greater than 70 years of age, only 26-24% of them do not suffer from co-morbidities. Of this group greater than 70 years of age, the men have the highest prevalence of complicating co-morbid conditions. These conditions can have a marked impact on the treatment of the individual’s CRC diagnosis. The short-term survival is also worsened in the presence of co-morbid conditions, especially cardiovascular co-morbidities.
- Cardiovascular disease
- Previously diagnosed CA
- Male – Large Bowel, Urinary Tract, Lung, and Prostate
- Female – Large Bowel, Breast, and Female Genital System
- Hypertension (F>M)
- Chronic Obstructive Pulmonary Disease
- Diabetes
Medications[edit | edit source]
Chemotherapy
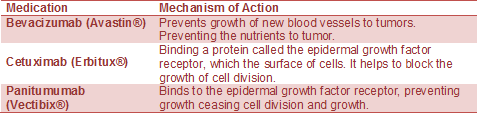
Targeted Drug Therapy
Monoclonal Antibody Therapy: proteins engineered to help the body’s natural immune system to attack and destroy colorectal cancer cells. It can be used independently or with other chemotherapy treatment.
Radiation Therapy: helps to destroy cancer cells and can be used in conjunction with chemotherapy.
Radiation options:
Intensity Modulated Radiation Therapy (IMRT)
Intraoperative Radiation Therapy (IORT)
CyberKnife®
TheraShpere®
TomoTherapy®
Trilogy™
Diagnostic Tests/Lab Tests/Lab Values[edit | edit source]
add text here
Etiology/Causes[edit | edit source]
Colon cancer originates from rapid cell proliferation of the epithelial cells called colonocytes that line the bowel, and somatic mutations in the p53 tumor-suppressor gene. The majority of CRCs are believed to occur sporadically leaving only about 10% to 20% of CRCs to have a known hereditary component
Developing polyps is a potential risk factor for CRC, particularly if they are adenomatous (glandular hyperplasia). The age of when polyps are diagnosed can be an indicator for prognosis and risk for developing cancer. Patients with adenomatous colorectal polyps have an increased risk of 1.78 in developing CRC. The risk increases if the polyps are diagnosed before the age of 60 to 2.59. The larger the polyp the greater probability the polyp is cancerous compared to smaller polyps. Another kind of adenomatous polyp is called familial adenomatous polyposis which is an autosomal-dominant disease. This disease has an occurrence rate of 1:7000 to 1:10,000. The colon is completely covered with polyps and if medical management does not take action approximately 50-75% of patient will develop CRC.
Risks
Genetic influence of relatives who have been diagnosed with any type of cancer can increase the risk for CRC. A first-degree relative with CRC has a 2-4 times the risk. Cancer family syndrome is an autosomal-dominant dis
order that puts the patient at 33% risk of developing cancer by the age of 50.
Genetic changes are responsible and have an important role for hyperproliferation of carcinogenic cells which due to ulcerative colitis, acromegaly, family history of colonic neoplasia, certain professions, smoking & drinking, consumption of red or processed meat, etc.
Inflammation of the colon and rectum are associated with an increased risk of colorectal cancer. The large intestines have an increase amount of bacteria present compared to the small intestines. This is can become problematic as it relates to an increase in proliferation of colonic carcinogens. Bile acids secreted in the intestines can act as tumor promoters and has shown to contribute to colon cancer.
Twenty-five percent of patients who have inflammatory bowel disease, ulcerative colitis, have an increased risk if they’ve had the disease for over 25 years. At a lesser degree, Crohn’s disease may also have an influence of risk.
Systemic Involvement[edit | edit source]
add text here
Medical Management (current best evidence)[edit | edit source]
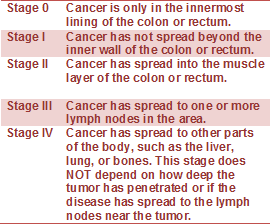
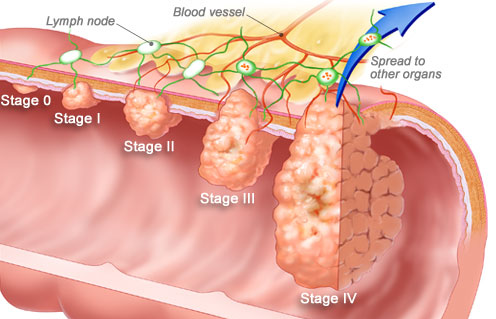
Staging of Colorectal Cancer
If cancer is detected, it will be "staged," a process of finding out how far the cancer has spread. Tumor size may not correlate with the stage of cancer. Staging also enables your doctor to determine what type of treatment you will receive.
Physical Therapy Management (current best evidence)[edit | edit source]
add text here
Alternative/Holistic Management (current best evidence)[edit | edit source]
Nutrition Therapy
Preventing Colorectal Cancer: Diet
There are steps you can take to dramatically reduce your odds of developing colorectal cancer. Researchers estimate that eating a nutritious diet, getting enough exercise, and controlling body fat could prevent 45% of colorectal cancers. The National Cancer Institute recommends a low-fat diet that includes plenty of fiber and at least five servings of fruits and vegetables per day.
-solid food may not be an option, depending on the stage and treatment
Pain management
Naturopathic therapy
Mind Body Medicine
Differential Diagnosis[edit | edit source]
add text here
Case Reports/ Case Studies[edit | edit source]
add links to case studies here (case studies should be added on new pages using the case study template)
Resources
[edit | edit source]
Recent Related Research (from Pubmed)[edit | edit source]
see tutorial on Adding PubMed Feed
Failed to load RSS feed from http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1NGmwZeh8JwVIzrKgHG1LrDm0izTr7ViJiDkSYAY2BW5hiXsx0|charset=UTF-8|short|max=10: Error parsing XML for RSS
References[edit | edit source]
- ↑ Colorectal Cancer Overview [Internet]. American Cancer Society. 2013 [updated 2013 Jan 17]. Available from: http://www.cancer.org/cancer/colonandrectumcancer/overviewguide/colorectal-cancer-overview-key-statistics.
- ↑ 2.0 2.1 Seer Stat Facts Sheets: Colon and Rectum [Internet]. National Cancer Institute. 2012 [updated 2011 Nov]. Available from: http://seer.cancer.gov/statfacts/html/colorect.html.
- ↑ Enzinger PC, Benson AB, Mitchell EP, et al. Medical Update on Colorectal Cancer Understanding KRAS [pamphlet]. New York: Elsevier Oncology; 2010.
- ↑ Colorectal (Colon) Cancer [Internet]. Center for Disease Control. 2012 [updated 2012 Oct 22]. Available from: http://www.cdc.gov/cancer/colorectal/index.htm.
- ↑ Tidy, Colin MD. Colorectal Cancer [Internet]. Patient.co.uk; 2012 [updated 2012 July 19]. Available from: http://www.patient.co.uk/doctor/colorectal-adenocarcinoma.htm.
- ↑ De Marco MF, Janssen-Heijnen ML, Van Der Heijden LH, et al. Comorbidity and colorectal cancer according to subsite and stage: a population-based study. Eur J Cancer. 2000 Jan; 36(1): 95-9