Cervicogenic dizziness: screening
Introduction[edit | edit source]
Patients who suffer from dizziness can be classified into different subgroups based on different characteristics. Cervicogenic dizziness is one of the possible causes of dizziness.1,14 It has been defined as an aspecific sensation of changed spatial orientation and disequilibrum as a consequence of a proprioceptive disorder of the cervical afferents. It occurs with certain positions and movements of the cervical spine and can be accompanied with a stiff or painfull feeling in the neck.2,3,4 At this moment there are no diagnostic tests available to state that the dizziness of the patient has a cervicogenic origin. It's a diagnosis of exclusion which means that other causes of dizziness have to be excluded first.
The user's manual which is presented on this page describes the tests which are used in a screenings tool for cervicogenic dizziness. This tool is part of a master thesis at the University of Brussel for becoming a manual therapist. Therefore the tool is still in development. The goal of this screening tool is to increase the probability of deciding correctly whether dizziness has a cervicogenic origin based on the patient history and clinical examination. In the tool it is indicated which findings can be reason for referral.
Legend[edit | edit source]
| Bold findings | These are findings where you have to consider referral to specialistic care because of a possible serious underlying pathology. Think about pathologies of the central nervous system, vestibular disorders or cardiovascular problems. |
| (pathologies in italic between brackets) | These are a few possible pathologies for each finding which you can keep in mind. |
| BPPV | Benign Paroxysmal Positioning Vertigo |
| CAD | Cervical Arterial Dysfunction |
| CD | Cervicogenic Dizziness |
| CVA | Cerebrovascular Accident |
| TIA | Transient Ischemic Attack |
Practical use
[edit | edit source]
The tool is developed so that the patient history and clinical examination can be taken in a structured way. There is the possibility to tick off one or more characteristics/findings per item. When there are no specific findings, nothing has to be ticked off. Some findings are an indication of different pathologies. A cluster of symptoms give a greater probability for a certain pathology.
Content[edit | edit source]
- General data
Fill in general data such as name, date of birth and the date of taking the tool.
- Diagnosis on doctor's prescription
If applicable: fill in the diagnosis written on the prescription. If present, data about medical imaging can be noted too.
- Patient history
Systematically go through all items.
If no headache and/or neckpain is reported, item 3a and/or 3b don't have to be questionned. When the patient history is finished, look back at the findings and evaluate if there is a pattern pointing at a specific pathology. When presuming a serious pathology or a situation that you cannot treat as a physiotherapist, refer the patient for further examination and/or treatment.
- Clinical examination
Look at the tests below.
1. Otoneurological testing [edit | edit source]
Romberg test: [edit | edit source]
Performance: The patient stands upright with both feet together. First the test is performed with the eyes open, then with the eyes closed.
Assessment: Check if the patient gets dizzy or looses his equilibrum with the eyes open and/or closed. Look for deviations, direction of deviations and influence of distraction.
Finger-pointing test: [edit | edit source]
Performance: The patient sits or stands in front of the therapist. The patient has to follow with his index finger the finger of the therapist as accurately as possible without touching it.
Assessment: Asses the direction of overshoot and intentiontremor.
Babinski-Weil test: [edit | edit source]
Performance: The patient walks 4 or 5 steps forwards and backwards with the eyes closed and both arms stretched forward at shoulder height. This is repeated a couple of times without opening the eyes in the meantime.
Assessment: Evaluate deviations and the direction of deviations of a straight for- and backwards walking pattern. The consecutive deviations can form a typical pattern assembling a star. Compare the width of the support base (wide vs narrow) between walking with the eyes open and closed.
Inspection of spontaneous nystagmus: [edit | edit source]
Performance: Evaluate spontaneous nystagmus. First look at the patients eyes while the patient looks at a point in front of him at a distance of more than 2 meters. Then the presence of a spontaneous nystagmus is evaluated while the patient stares from different eye-angles, such as looking upwards or to the left.
Assessment: Check the presence of a nystagmus. Nystagmus is an involuntary, rhytmic, osscilatory eye movement. A spontaneous nystagmus is a reason for referral for specialistic examination, regardless of direction, frequency or speed.
Saccadic eye movements: [edit | edit source]
Performance: The patient quickly changes his gaze from one point to anothor.
Assessment: Asses the presence of overshoot or undershoot of the eye movements and aberrant saccadic eye movements.
Smooth pursuit test: [edit | edit source]
Performance: The patient keeps the head steady and tries to follow a slowly moving object with his eyes.
Assessment: Look for influent eye movements or saccades. Other recognizable symptoms can be provoked.
Gaze stability:[edit | edit source]
Performance: The patient tries to keep his eyes fixed on a stable object while the head is actively moved into different directions.
Assessment: Evaluate the impossibility to fixate and saccadic or aberrant neck movements. Other recognizable symptoms such as dizziness, blurred vision and nausea can be provoked.
Eye-head coordination: [edit | edit source]
Performance: First the patient moves his eyes towards a fixed object. While keeping his gaze fixed at the object he turns his head towards the object. This can be performed into different directions: left, right, up, down,...
Assessment: Check for impossibility to dissociate eye- and head movements. Other recognizable symptoms can be provoked.
Whisper test: [edit | edit source]
Performance: The test can be performed while the patient is sitting or standing. Perform the test at patient's height. The therapist sits or stands behind the patient at arm's length. The patient covers one ear and has to repeat the combinations that are whispered by the therapist. These are six combinations of three numbers or letters. For example: 66F, G8D, 1KL.
Assessment: The test is aberrant if the patient cannot repeat more than four (out of six) combinations
2. Examination BPPV[edit | edit source]
Dix-Hallpike manoeuvre: [edit | edit source]
Performance: The patient takes in a long-sitting position. The head is turned 45° to one side. The therapist assists the patient quickly getting into the supine position with his head over the edge of the table in 30° of extension, maintaining the rotation. This position is maintained for at least 30 seconds. The test is repeated with the head turned to the other side.
Assessment: Note whether the test is positive for rotation of the head to the right, to the left or both. Check occurence of vertigo, presence and direction of nystagmus, latention time and time before nystagmus/vertigo has disappeared.
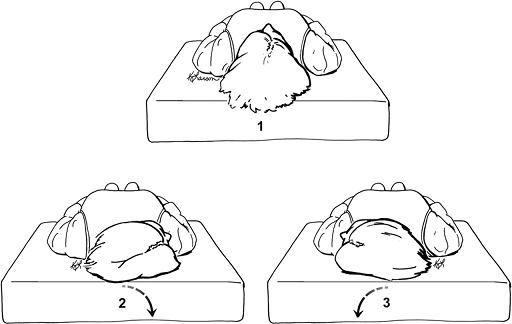
Roll test: [edit | edit source]
Performance: This test is only performed if the Dix-Hallpike is negative but there is a strong suspicion of BBPV. The patient lies supine with his head 30° flexed. The therapist assists the patient rolling quickly to one side. The head stays in 30° of flexion. This position is maintained for at least one minute. The test is repeated with rotating to the other side.
Assessment: Occurence of vertigo, presence and direction of nystagmus, latention time and time before the nystagmus/vertigo has disappeared.
3. Examination of the cervical region[edit | edit source]
Inspection: [edit | edit source]
Performance: Inspect the patient in sitting or standing position
Assessment: Check for an aberrant position such as lateral flexion of the head or forward head posture.
Palpate muscle pain: [edit | edit source]
Performance: The therapist palpates the muscles with finger II and III with the amount of pressure that makes the fingertip turns white.
Assessment: Scoring pain reaction 0-3:
0. no pain or visible reaction
1. light tenderness and no visible reaction
2. painfull touch and visible reaction
3. serious pain and significant visible reaction, jump sign
Functional examination: [edit | edit source]
Performance: The test is performed with the patient lying or sitting. The functional examination can be performed according to the guidelines of Aad van der El.
Assessment: During the examination the therapist controls functional disorders, pain and dizziness. In the corresponding table the findings can be noted as follows:
Functional disorder: fill in the motion(s) and direction(s) (left/right) that are disturbed.
Pain: fill in the motion(s) and direction(s) (left/right) that are painfull.
Dizziness: fill in which motion(s) and direction(s) (left/right) provoke dizziness.
When there are no aberrant findings, a '/' can be filled in.
For example:
| Regional: actively assisted | Functional disorder | Pain | Dizziness |
| C0-3 | Rot left, 3D flex left | Rot left | / |
Cervical position sense: [edit | edit source]
Performance: The patient sits in front of a wall on a distance of 90cm with a laser attached on a hairband. The starting point of the laser is marked on the wall. The patient performs 1D head motions with the eyes closed and tries to reproduce his neutral head position.
Assessment: Measure the distance between the starting point and the point where the laser stops after the head movement. The critical distance is 7cm. This is also called the 'joint positioning error' (JPE).