Cervicogenic dizziness: screening: Difference between revisions
Rachael Lowe (talk | contribs) mNo edit summary |
Rachael Lowe (talk | contribs) mNo edit summary |
||
| Line 1: | Line 1: | ||
== Introduction == | == Introduction == | ||
Patients who suffer from dizziness can be classified into different subgroups based on different characteristics. Cervicogenic dizziness is one of the possible causes of dizziness. It has been defined as an a specific sensation of changed spatial orientation and disequilibrium as a consequence of a proprioceptive disorder of the cervical afferents. It occurs with certain positions and movements of the cervical spine and can be accompanied with a stiff or painful feeling in the neck. At this moment there are no diagnostic tests available to state that the dizziness of the patient has a cervicogenic origin. It's a diagnosis of exclusion which means that other causes of dizziness have to be excluded first. | |||
== Subjective Assessment == | |||
The sensation of dizziness is specific to the person and type of condition. The most common sensations expressed by patients suffering from dizziness and balance disorders are<ref>Otoneurological tests to diagnose vertigo. http://www.lesvertiges.com/en/assessment.html [Accessed on 19 Sep 2017] | |||
</ref>: | |||
* Rotary vertigo: "the room spins, I feel nauseous and am sick.” | |||
* “I feel constantly unsteady.” | |||
* “Feeling lightheaded “but not euphoric” despite the fact that I never drink.” | |||
* “When I lean forward, I feel like everything is spinning and I have to hold onto something.” | |||
* “If I lean my head back I feel like I'm going to faint.” | |||
* “I feel constantly unsteady when I walk.” | |||
* “Suddenly I felt pressure and ringing in my ear and I became dizzy.” | |||
* “When I walk it feels like I’m sinking into the ground.” | |||
* “When I turn my head too fast, my vision blurs.” | |||
* “I suddenly had stomach pain and nausea, I got up and I was sick; the room was spinning. I thought I had a stomach bug.” | |||
* “It's like I am constantly seasick.” | |||
* “It’s like being shoved sideways and I lose my balance.” | |||
* “I stagger when I walk.” | |||
== Objective testing == | |||
== | |||
=== Otoneurological testing === | === Otoneurological testing === | ||
The otoneurological assessment is for patients who suffer from rotary vertigo, loss of balance or light-headedness. Both functions of the inner ear should be explored: the auditory function and the vestibular function. Indeed, in addition to its role in the perception of sounds, the inner ear is essential in balancing and steadying our gaze when we move our head. | |||
==== Romberg test | ==== [[Romberg Test|Romberg test]] ==== | ||
<u>Performance:</u> The patient stands upright with both feet together. First the test is performed with the eyes open, then with the eyes closed.<br><u>Assessment</u>: Check if the patient gets dizzy or looses his | <u>Performance:</u> The patient stands upright with both feet together. First the test is performed with the eyes open, then with the eyes closed.<br><u>Assessment</u>: Check if the patient gets dizzy or looses his equilibrium with the eyes open and/or closed. Look for deviations, direction of deviations and influence of distraction. | ||
==== Finger-pointing test | ==== Finger-pointing test ==== | ||
<u>Performance:</u> The patient sits or stands in front of the therapist. The patient has to follow with his index finger the finger of the therapist as accurately as possible without touching it.<br><u>Assessment:</u> Assess the direction of overshoot and | <u>Performance:</u> The patient sits or stands in front of the therapist. The patient has to follow with his index finger the finger of the therapist as accurately as possible without touching it.<br><u>Assessment:</u> Assess the direction of overshoot and intention tremor. | ||
==== Babinski-Weil test | ==== Babinski-Weil test ==== | ||
<u>Performance</u>: The patient walks 4 or 5 steps forwards and backwards with the eyes closed and both arms stretched forward at shoulder height. This is repeated a couple of times without opening the eyes in the meantime. <br><u>Assessment</u>: Evaluate deviations and the direction of deviations of a straight for- and backwards walking pattern. The consecutive deviations can form a typical pattern assembling a star. Compare the width of the support base (wide vs narrow) between walking with the eyes open and closed. | <u>Performance</u>: The patient walks 4 or 5 steps forwards and backwards with the eyes closed and both arms stretched forward at shoulder height. This is repeated a couple of times without opening the eyes in the meantime. <br><u>Assessment</u>: Evaluate deviations and the direction of deviations of a straight for- and backwards walking pattern. The consecutive deviations can form a typical pattern assembling a star. Compare the width of the support base (wide vs narrow) between walking with the eyes open and closed. | ||
==== Inspection of spontaneous nystagmus | ==== Inspection of spontaneous nystagmus ==== | ||
<u>Performance</u>: Evaluate spontaneous nystagmus. First look at the patients eyes while the patient looks at a point in front of him at a distance of more than 2 meters. Then the presence of a spontaneous nystagmus is evaluated while the patient stares from different eye-angles, such as looking upwards or to the left. <br><u>Assessment:</u> Check the presence of a nystagmus. Nystagmus is an involuntary, rhytmic, osscilatory eye movement. A spontaneous nystagmus is a reason for referral for specialistic examination, regardless of direction, frequency or speed. | |||
<u>Performance</u>: | ==== Saccadic eye movements ==== | ||
<u>Performance</u>: The patient quickly changes his gaze from one point to another. <br><u>Assessment</u>: Assess the presence of overshoot or undershoot of the eye movements and aberrant saccadic eye movements. | |||
==== | ==== Smooth pursuit test ==== | ||
<u>Performance</u>: The patient | <u>Performance</u>: The patient keeps the head steady and tries to follow a slowly moving object with his eyes. <br><u>Assessment</u>: Look for influent eye movements or saccades. Other recognisable symptoms can be provoked | ||
==== Gaze stability ==== | |||
<u>Performance</u>: The patient tries to keep his eyes fixed on a stable object while the head is actively moved into different directions.<br><u>Assessment</u>: Evaluate the impossibility to fixate and the presence of saccadic or aberrant neck movements. Other recognisable symptoms such as dizziness, blurred vision and nausea can be provoked. | |||
==== Eye-head coordination ==== | |||
<br> | <u>Performance</u>: First the patient moves his eyes towards a fixed object. While keeping his gaze fixed at the object he turns his head towards the object. This can be performed into different directions: left, right, up, down,... <br><u>Assessment</u>: Check for impossibility to dissociate eye- and head movements. Other recognisable symptoms can be provoked. | ||
==== | ==== Whisper test ==== | ||
<u>Performance</u>: The test can be performed while the patient is sitting or standing. Perform the test at patient's height. The therapist sits or stands behind the patient at arm's length. The patient covers one ear and has to repeat the combinations that are whispered by the therapist. These are six combinations of three numbers or letters. For example: 66F, G8D, 1KL. <br><u>Assessment</u>: The test is aberrant if the patient cannot repeat more than four (out of six) combinations | |||
=== Examination of Benign Paroxysmal Positioning Vertigo (BPPV) === | |||
==== Dix-Hallpike manoeuvre ==== | |||
==== Dix-Hallpike manoeuvre | |||
<u>Performance:</u> The patient takes in a long-sitting position. The head is turned 45° to one side. The therapist assists the patient quickly getting into the supine position with his head over the edge of the table in 30° of extension, maintaining the rotation. This position is maintained for at least 30 seconds. The test is repeated with the head turned to the other side. <br><u>Assessment: </u>Note whether the test is positive for rotation of the head to the right, to the left or both. Check occurence of vertigo, presence and direction of nystagmus, latention time and time before nystagmus/vertigo has disappeared. <br> | <u>Performance:</u> The patient takes in a long-sitting position. The head is turned 45° to one side. The therapist assists the patient quickly getting into the supine position with his head over the edge of the table in 30° of extension, maintaining the rotation. This position is maintained for at least 30 seconds. The test is repeated with the head turned to the other side. <br><u>Assessment: </u>Note whether the test is positive for rotation of the head to the right, to the left or both. Check occurence of vertigo, presence and direction of nystagmus, latention time and time before nystagmus/vertigo has disappeared. <br> | ||
[[Image:Dix-hallpike.jpg]] | [[Image:Dix-hallpike.jpg]]<br> | ||
==== Roll test | ==== Roll test ==== | ||
<u><span>Performance:</span></u><span> This test is only performed if the Dix-Hallpike is negative but there is a strong suspicion of BBPV.</span><span style="line-height: 1.5em;"> The patient lies supine with his head 30° flexed.</span><span style="line-height: 1.5em;"> The therapist assists the patient rolling quickly to one side.</span><span style="line-height: 1.5em;"> The head stays in 30° of flexion.</span><span style="line-height: 1.5em;"> This position is maintained for at least one minute.</span><span style="line-height: 1.5em;"> The test is repeated with rotation to the other side.</span><br><span><u>Assessment:</u> Occurence of vertigo, presence and direction of nystagmus, latention time and time before the nystagmus/vertigo has disappeared.</span><span style="line-height: 1.5em;"> </span> | <u><span>Performance:</span></u><span> This test is only performed if the Dix-Hallpike is negative but there is a strong suspicion of BBPV.</span><span style="line-height: 1.5em;"> The patient lies supine with his head 30° flexed.</span><span style="line-height: 1.5em;"> The therapist assists the patient rolling quickly to one side.</span><span style="line-height: 1.5em;"> The head stays in 30° of flexion.</span><span style="line-height: 1.5em;"> This position is maintained for at least one minute.</span><span style="line-height: 1.5em;"> The test is repeated with rotation to the other side.</span><br><span><u>Assessment:</u> Occurence of vertigo, presence and direction of nystagmus, latention time and time before the nystagmus/vertigo has disappeared.</span><span style="line-height: 1.5em;"> </span> | ||
[[Image:Supine roll test.jpg]] | [[Image:Supine roll test.jpg]] | ||
=== Examination of the cervical region === | |||
A normal cervical examination can be performed. Any dizziness reported in the cervical assessment indicates the need for further investigation | |||
=== | ==== [[Vertebral Artery Test]] ==== | ||
The vertebral artery test is used to test the vertebral artery blood flow, searching for symptoms of vertebral artery insufficiency and disease.<br>[[Vertebral Artery Test|Read more here]] | |||
==== | ==== Cervical position sense ==== | ||
<u>Performance:</u> | <u>Performance:</u> The patient sits in front of a wall on a distance of 90cm with a laser attached on a hairband. The starting point of the laser is marked on the wall. The patient performs 1D head motions with the eyes closed and tries to reproduce his neutral head position. <br><u>Assessment:</u> Measure the distance between the starting point and the point where the laser stops after the head movement. The critical distance is 7cm. This is also called the 'joint positioning error' (JPE). | ||
[[Image:JPE.jpg]]<br> | |||
== References == | |||
<references /><br><br><br><br> | |||
[[Category:Cervical Examination]] | [[Category:Cervical Examination]] | ||
Revision as of 14:17, 19 September 2017
Introduction[edit | edit source]
Patients who suffer from dizziness can be classified into different subgroups based on different characteristics. Cervicogenic dizziness is one of the possible causes of dizziness. It has been defined as an a specific sensation of changed spatial orientation and disequilibrium as a consequence of a proprioceptive disorder of the cervical afferents. It occurs with certain positions and movements of the cervical spine and can be accompanied with a stiff or painful feeling in the neck. At this moment there are no diagnostic tests available to state that the dizziness of the patient has a cervicogenic origin. It's a diagnosis of exclusion which means that other causes of dizziness have to be excluded first.
Subjective Assessment[edit | edit source]
The sensation of dizziness is specific to the person and type of condition. The most common sensations expressed by patients suffering from dizziness and balance disorders are[1]:
- Rotary vertigo: "the room spins, I feel nauseous and am sick.”
- “I feel constantly unsteady.”
- “Feeling lightheaded “but not euphoric” despite the fact that I never drink.”
- “When I lean forward, I feel like everything is spinning and I have to hold onto something.”
- “If I lean my head back I feel like I'm going to faint.”
- “I feel constantly unsteady when I walk.”
- “Suddenly I felt pressure and ringing in my ear and I became dizzy.”
- “When I walk it feels like I’m sinking into the ground.”
- “When I turn my head too fast, my vision blurs.”
- “I suddenly had stomach pain and nausea, I got up and I was sick; the room was spinning. I thought I had a stomach bug.”
- “It's like I am constantly seasick.”
- “It’s like being shoved sideways and I lose my balance.”
- “I stagger when I walk.”
Objective testing[edit | edit source]
Otoneurological testing [edit | edit source]
The otoneurological assessment is for patients who suffer from rotary vertigo, loss of balance or light-headedness. Both functions of the inner ear should be explored: the auditory function and the vestibular function. Indeed, in addition to its role in the perception of sounds, the inner ear is essential in balancing and steadying our gaze when we move our head.
Romberg test [edit | edit source]
Performance: The patient stands upright with both feet together. First the test is performed with the eyes open, then with the eyes closed.
Assessment: Check if the patient gets dizzy or looses his equilibrium with the eyes open and/or closed. Look for deviations, direction of deviations and influence of distraction.
Finger-pointing test [edit | edit source]
Performance: The patient sits or stands in front of the therapist. The patient has to follow with his index finger the finger of the therapist as accurately as possible without touching it.
Assessment: Assess the direction of overshoot and intention tremor.
Babinski-Weil test [edit | edit source]
Performance: The patient walks 4 or 5 steps forwards and backwards with the eyes closed and both arms stretched forward at shoulder height. This is repeated a couple of times without opening the eyes in the meantime.
Assessment: Evaluate deviations and the direction of deviations of a straight for- and backwards walking pattern. The consecutive deviations can form a typical pattern assembling a star. Compare the width of the support base (wide vs narrow) between walking with the eyes open and closed.
Inspection of spontaneous nystagmus[edit | edit source]
Performance: Evaluate spontaneous nystagmus. First look at the patients eyes while the patient looks at a point in front of him at a distance of more than 2 meters. Then the presence of a spontaneous nystagmus is evaluated while the patient stares from different eye-angles, such as looking upwards or to the left.
Assessment: Check the presence of a nystagmus. Nystagmus is an involuntary, rhytmic, osscilatory eye movement. A spontaneous nystagmus is a reason for referral for specialistic examination, regardless of direction, frequency or speed.
Saccadic eye movements [edit | edit source]
Performance: The patient quickly changes his gaze from one point to another.
Assessment: Assess the presence of overshoot or undershoot of the eye movements and aberrant saccadic eye movements.
Smooth pursuit test [edit | edit source]
Performance: The patient keeps the head steady and tries to follow a slowly moving object with his eyes.
Assessment: Look for influent eye movements or saccades. Other recognisable symptoms can be provoked
Gaze stability[edit | edit source]
Performance: The patient tries to keep his eyes fixed on a stable object while the head is actively moved into different directions.
Assessment: Evaluate the impossibility to fixate and the presence of saccadic or aberrant neck movements. Other recognisable symptoms such as dizziness, blurred vision and nausea can be provoked.
Eye-head coordination [edit | edit source]
Performance: First the patient moves his eyes towards a fixed object. While keeping his gaze fixed at the object he turns his head towards the object. This can be performed into different directions: left, right, up, down,...
Assessment: Check for impossibility to dissociate eye- and head movements. Other recognisable symptoms can be provoked.
Whisper test [edit | edit source]
Performance: The test can be performed while the patient is sitting or standing. Perform the test at patient's height. The therapist sits or stands behind the patient at arm's length. The patient covers one ear and has to repeat the combinations that are whispered by the therapist. These are six combinations of three numbers or letters. For example: 66F, G8D, 1KL.
Assessment: The test is aberrant if the patient cannot repeat more than four (out of six) combinations
Examination of Benign Paroxysmal Positioning Vertigo (BPPV)[edit | edit source]
Dix-Hallpike manoeuvre [edit | edit source]
Performance: The patient takes in a long-sitting position. The head is turned 45° to one side. The therapist assists the patient quickly getting into the supine position with his head over the edge of the table in 30° of extension, maintaining the rotation. This position is maintained for at least 30 seconds. The test is repeated with the head turned to the other side.
Assessment: Note whether the test is positive for rotation of the head to the right, to the left or both. Check occurence of vertigo, presence and direction of nystagmus, latention time and time before nystagmus/vertigo has disappeared.
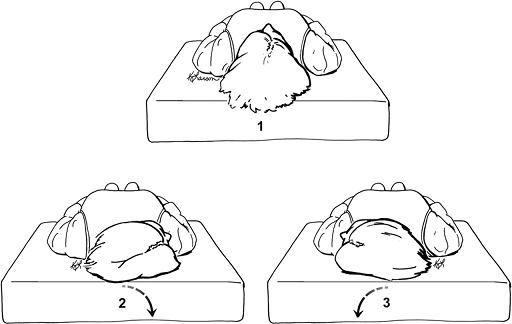
Roll test [edit | edit source]
Performance: This test is only performed if the Dix-Hallpike is negative but there is a strong suspicion of BBPV. The patient lies supine with his head 30° flexed. The therapist assists the patient rolling quickly to one side. The head stays in 30° of flexion. This position is maintained for at least one minute. The test is repeated with rotation to the other side.
Assessment: Occurence of vertigo, presence and direction of nystagmus, latention time and time before the nystagmus/vertigo has disappeared.
Examination of the cervical region[edit | edit source]
A normal cervical examination can be performed. Any dizziness reported in the cervical assessment indicates the need for further investigation
Vertebral Artery Test[edit | edit source]
The vertebral artery test is used to test the vertebral artery blood flow, searching for symptoms of vertebral artery insufficiency and disease.
Read more here
Cervical position sense [edit | edit source]
Performance: The patient sits in front of a wall on a distance of 90cm with a laser attached on a hairband. The starting point of the laser is marked on the wall. The patient performs 1D head motions with the eyes closed and tries to reproduce his neutral head position.
Assessment: Measure the distance between the starting point and the point where the laser stops after the head movement. The critical distance is 7cm. This is also called the 'joint positioning error' (JPE).
References[edit | edit source]
- ↑ Otoneurological tests to diagnose vertigo. http://www.lesvertiges.com/en/assessment.html [Accessed on 19 Sep 2017]