Cervical Spine Fractures in Contact Sports
Introduction[edit | edit source]
The cervical spine is a dynamic structure that protects nervous innervation to the entire body while maintaining the range of motion for the head and neck. It contains seven vertebrae, which provides supports to the head while allowing for side flexion, rotation, flexion and extension [1].
Cervical spine fractures are a primary cause of mobility loss and mortality in trauma patients, with a bone fracture accounting for 56% of cervical spinal cord injuries. Damage to the spinal cord could have serious consequences as it is where the central nervous system connects between the brain and the body. A spinal cord injury at the cervical spine can lead to temporary or permanent paralysis of the entire body from the neck down. Fractures of the cervical spine are classified into three groups based on the level of involvement: C1, C2 and the sub-axial spine (C3 to C7) [2].
The most common causes of cervical fractures are motor vehicle accidents, falls, violence, and sports activities. This Physiopedia page will be focussing on fractures in the cervical vertebral in sports that involve physical contact. Contact sports, e.g. American football, ice hockey, football, rugby, carry a risk of cervical injuries as cervical fracture could occur in actions like spearing an opponent with the head in contact sports.
Pathophysiology[edit | edit source]
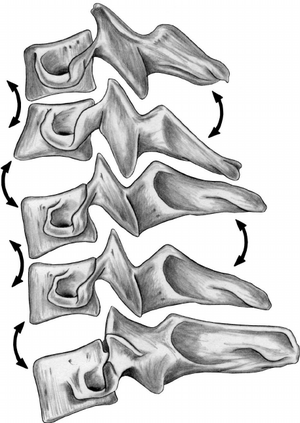
A fracture to the cervical spine could result from compression (frequently caused by minor trauma in people with osteoporosis), burst fractures (vertebrae crushed in all directions) or a fracture-dislocation (from car collisions or falls from heights). C1 fractures typically occur due to axial loading. A combination of compression, hyperflexion, and hyperextension are the most common cause of C2 fractures. High-impact accidents are known to commonly cause sub-axial cervical spine fractures. [3].
Epidemiology[edit | edit source]
The literature suggests that cervical fractures are most commonly seen in association with trauma, often in young males participating in contact sports. However, there is some divide over the prevalence rates and the specificities of certain risk factors. This may be due to the fact that often studies used populations who were already exposed to trauma and were done on spinal injuries as a whole instead of specifically cervical fractures. Much of the literature agrees motor vehicle accidents to be the most common cause, with prevalence ranging from 48%-66% (van Den Hauwe et al 2020) (Khanpara et al 2019). Contact sporting injuries and falling from heights followed ranging from 14%-21% and cases from assault ranging from 10-15% (van Den Hauwe et al 2020). Despite not being as common, the literature also acknowledged the occurrence of specifically atlas fractures in the elderly, with this being primarily alongside other head and neck injuries (Fiedler et al 2020). A study by Khanpara et al (2019) suggested fractures to C1 and C2 to be the most prevalent across all causes and specifically closed fractures to C2 and C7 to be the most frequent. It was also posed that the incidence of cervical fractures has increased between 2005 and 2013 from 62.3% to 67.6%.
Risk factors for sustaining cervical fractures in contact sports
Already participating in contact sports to any level increases the risks of attaining a cervical fracture yet the research suggests that within this, males may be at greater risk than females with a male: female ratio of 2:1 suggested (khanpara et al 2019). Age was probably the most emphasised risk factor across all studies with much of the literature attempting to identify a specific ‘red zone’ although there appeared to be great variability in this. The overall range varied between 15-35 years, with some studies suggesting this to be narrower of 20-29 (Andrew et al 2012). One of the more recent studies suggested an age of 18-25 with 80% of all cervical fractures in the study falling into that age group (Feldman,2018). Osteoporosis and osteoarthritis were also identified as other less common risk factors alongside other chronic conditions such as congenital stenosis (Schroeder et al 2016).
Which sports are cervical fractures the most common in?
Although cervical fractures are particularly common in contact sports, more recent studies are suggesting athletes participating in non-contact sports such as diving, horse riding and cycling to be also at significant risk . A study by DePasse et al (2019) identified cycling to be the most common cause of a cervical fracture after diving and football in males. The peak in prevalence of cervical fractures in cycling between 2000-2015 was said to be partly responsible for the overall incidence of sport related cervical fractures to have increased by 35% during this period. The study identified horse riding to be the most common for females, and then followed by cycling. This more recent evidence suggests a shift in the prevalence of cervical fractures from certain sports.
Aetiology/Mechanism of Injury[edit | edit source]
The mechanism of injury for a cervical fracture is complex and much is still unexplored in regards to mechanisms specific to certain sports. The literature seemed to identify axial loading, buckling, the influence of padding and whiplash to be some of the key injury biomechanics involved in cervical fractures in contact sports (Swartz et al 2005). It was also emphasised over the importance of those involved in pitch side work to be able to understand the mechanisms of injury for a cervical fracture to be able to recognise them during play.
Axial loading
The mechanism of axial loading arises when the head and neck are flexed to around 30 degrees which causes the normal lordotic curve to disappear which means that the spine is not able to absorb the impact, resulting in a fracture (Torg et al 1991). A study by Swartz et al (2005) identified axial loading as a mechanism of injury to be the cause of 27% of tackling injuries. A key factor in this was players tackling with their heads down or using the crown of their head as the initial point of contact during a tackle. As a result of the collision the head stops but trunk continues to move. The study suggested perhaps the use of the shoulder for blocking and tackling should be more encouraged instead to reduce the chances of axial loading occurring (Cantu et al 2000). Buckling
Buckling can occur during axial loading due to the compressive forces resulting in angulations within the cervical spine as an attempt to release the energy caused by the axial loading (Swartz et al 2005). During buckling the players head and neck complex may not go through a noticeable observable motion yet during buckling the cervical spine often goes into an extreme position of hyperflexion or hyperextension which suggests that head and neck movement is not always a reliable indication for the severity of the potential injury.
Influence of padded surfaces
Padded surfaces are needed in contact sports for protection against blunt trauma however there is some uncertainty as to whether they provide any protection to the cervical spine itself and could in fact at act as a mechanism of injury for cervical fractures. The padding allows the impact force of the trauma to last longer meaning the head is in axial compression for longer, being depressed further into the padded surface. This phenomenon has been referred to ‘pocketing’ in studies as the padding forms a pocket for the head during the trauma making it near to impossible for the cervical spine to not be put under axial load and increasing the time it is under this load (Nightingale et al 1996).
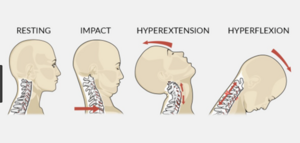
Whiplash
Whiplash can occur in contact sports, most often when a player is tackled from behind when they are not expecting it. In this situation the hips, back and trunk are the first areas to be moved by the force of the tackle. The trunk moves upwards and forwards to compress the cervical spine and causes the neck to extend resulting in tension being created through buckling as the lower cervical vertebrae extend and upper vertebrae flex. It is not the extension which is the ultimate mechanism of injury but the combination of the forward trunk movement, compression and buckling that rotate to force the vertebrae into extension, putting extreme pressure on the facet joints (Swartz et al 2005).
Pitch-side Management[edit | edit source]
Management of cervical spine injuries in sport starts from the moment the player goes down on the pitch. Until a cervical spine injury can be definitively ruled out, players need to be handled with the utmost care to prevent exacerbating the injury and causing permanent harm.
Assessing on the Pitch
As pitch-side practitioners do not have the tools nor time to accurately determine whether a player has a C-Spine injury, the most telling sign is usually the mechanism of injury. Prompt identification of any potentially catastrophic injuries is vital. Crosby et al., estimates that 2-5% of blunt trauma patients have a cervical spine injury.
If the practitioner witnessed trauma to the head or neck, or if their view was restricted and they could not see, then they must immediately perform manual inline stabilisation (MILS) to take control of the head. MILS is a manoeuvre used when a patient has suspected C-Spine trauma to provide a degree of stability to the cervical spine, prior to the application of a cervical collar (Queensland Ambulance Services, 2016). This will help minimise excessive movement and thereby reduce the chance of further injury. To perform MILS the practitioner or assistant should:
- Crouch/kneel/lie beside or behind the player
- The clinician should attempt to stabilise their elbows/arms on the ground, against another stable object or on their knees to prevent swaying as they become fatigued
- Place both hands on the patient’s mastoid processes or cradle the occiput
- Apply equal pressure so not to move the head or let it fall
Primary Survey
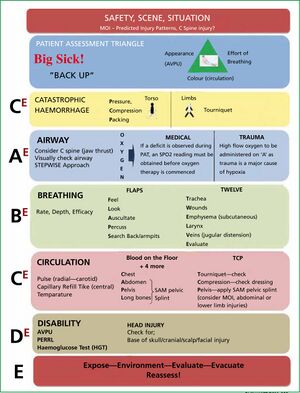
To assess a patient on the field, the clinician must first perform a primary survey. The first part involves assessing the players alertness, and then includes checking the players airways, breathing and circulation to identify any life-threating injuries. This survey will identify immediately if the player is breathing normally. It will ensure that the medical practitioner is fully aware if they have to carry out immediate interventions that could save the players life. If no immediately life-threatening injuries are present, then the clinician should determine a level of consciousness and conduct a neurological screening.
Secondary Survey
The secondary survey is a detailed head-to-toe examination with the purpose of determining whether the player has suffered any other injuries. This on-field evaluation should include an examination of level of consciousness, cognitive and memory processes, and cranial nerve function, with awareness that significant brain injury is possible. This is determined with the help of an A-E assessment. Maddocks questions are also used to investigate the suspicion of a head injury. They’re 5 questions that are utilised to evaluate orientation as well as assessing short- and long-term memory function. The following is taken from the Sports Concussion Assessment Tool (SCAT). The SCAT is a standardised concussion screening tool used by medical practitioners as an effective pitch-side assessment mechanism:
The neurological evaluation of a conscious player can be used to further investigate potential C-Spine trauma and begins with questions about extremity numbness, painful dysesthesias or paraesthesia, weakness, and neck pain. A physical examination is limited to asking if the patient can move all of their limbs. If there is any gross weakness, numbness, or significant pain to the cervical region, then this could be indicative of a serious neurological deficit. If the athlete is unconscious or presents with any of the below symptoms, then they will need to be extracted off the pitch using a spinal motion-restriction device, such as a spinal board or cervical collar (Fischer et al., 2018).
- Blunt trauma and altered level of consciousness
- Spinal pain or tenderness
- Loss of cervical range of motion
- Neurologic complaint or findings (e.g., numbness or motor weakness in more than 1 limb)
- Anatomic deformity of the spine
Neck Immobilisation and Spinal Board Extraction
The gold standard for neck immobilization is the combined use of a hardboard, collar, sandbags, and tape or straps. This is used primarily during the prehospital transfers and can limit movement to 5% of the normal range (Crosby and Lui, 1990). It should be noted that this type of immobilisation carries a high risk of pressure injury.
Once the collar is secured, the player can be moved onto a spinal board using the log roll technique. The use of the log roll will be applied in 2 scenarios. This will be at matchday or training where there may be a number of experienced and relevantly trained helpers. The other scenario could be where there are no trained helpers, and the medical practitioner will be required to ‘coach’ any assistance. As a note of caution, the best practice could be to not attempt a log roll and to manage the player where they are (Conrad et al., 2012). It may be the case that the initial care given is to keep them warm and to apply oxygen to the player using a non-rebreathe mask with high flow oxygen (15L/ Min).
- To perform a log roll safely, a minimum of 5 people is required
- The leader will be in charge of the head, keeping it MILS and preventing excessive rotation of the neck. The leader will also be the one giving commands to the rest of the group
- Three assistants should be kneeling beside the player, and one will be in charge of moving the spinal board
- The three assistants will place their hands on the opposite side of the player’s body, interlocking their arms.
- On the leader’s command, the assistants will roll the injured player to 90degrees and the spinal board will be slid underneath them
- Once the spinal board is in place, the player will be rolled back down on, again on the leader’s command
- From here, the leader remains in place and another assistant will help place head blocks and straps on.
Whilst waiting for an ambulance, the Canadian C-Spine Rule can be used to determine whether a patient will need a scan. It is applicable to patients who are alert (Glasgow Coma Scale score of 15) and stable condition following trauma where cervical spine injury is a concern.
Management and Treatment[edit | edit source]
Text
References[edit | edit source]
- ↑ Frost, B., Camarero-Espinosa, S. and Foster, E., 2019. Materials for the Spine: Anatomy, Problems, and Solutions. Materials, [online] 12(2), p.253. Available at: <https://dx.doi.org/10.3390%2Fma12020253>.
- ↑ van Eck, C., Fourman, M., Abtahi, A., Alarcon, L., Donaldson, W. and Lee, J., 2017. Risk Factors for Failure of Nonoperative Treatment for Unilateral Cervical Facet Fractures. Asian Spine Journal, [online] 11(3), pp.356-364. Available at: <https://dx.doi.org/10.4184%2Fasj.2017.11.3.356>.
- ↑ Fehlings, M., Tetreault, L., Nater, A., Choma, T., Harrop, J., Mroz, T., Santaguida, C. and Smith, J., 2015. The Aging of the Global Population. Neurosurgery, [online] 77, pp.S1-S5. Available at: <https://doi.org/10.1227/neu.0000000000000953>.