Bulimia Nervosa: Difference between revisions
No edit summary |
No edit summary |
||
| Line 1: | Line 1: | ||
<div class="noeditbox">Welcome to [[Pathophysiology of Complex Patient Problems|PT 635 Pathophysiology of Complex Patient Problems]] This is a wiki created by and for the students in the School of Physical Therapy at Bellarmine University in Louisville KY. Please do not edit unless you are involved in this project, but please come back in the near future to check out new information!!</div><div class="editorbox"> | |||
'''Original Editors '''- [[Pathophysiology of Complex Patient Problems| | '''Original Editors '''- Nikki Gee from [[Pathophysiology of Complex Patient Problems|Bellarmine University's Pathophysiology of Complex Patient Problems project.]] | ||
'''Lead Editors''' - Your name will be added here if you are a lead editor on this page. [[Physiopedia:Editors|Read more.]] | '''Lead Editors''' - Your name will be added here if you are a lead editor on this page. [[Physiopedia:Editors|Read more.]] | ||
</div> | </div> | ||
== Definition/Description == | == Definition/Description == | ||
A condition during which a person eats a large amount of food in a short amount of time (binges), then uses some method of purging to avoid weight gain. Methods of purging include self-induced vomiting, use of laxatives or diuretics, and excessive exercise. <ref name="Office on Women's Health">Office on Women's Health in the U.S. Department of Health and Human Services. 2009. Available from: U.S. Department of Health and Human Services, Web site: http://www.womenshealth.gov/faq/bulimia-nervosa.cfm. Accessed February 2010.</ref><br> | A condition during which a person eats a large amount of food in a short amount of time (binges), then uses some method of purging to avoid weight gain. Methods of purging include self-induced vomiting, use of laxatives or diuretics, and excessive exercise. <ref name="Office on Women's Health">Office on Women's Health in the U.S. Department of Health and Human Services. 2009. Available from: U.S. Department of Health and Human Services, Web site: http://www.womenshealth.gov/faq/bulimia-nervosa.cfm. Accessed February 2010.</ref><br> | ||
Two types of bulimia nervosa have been defined. The purging type which involves self-induced vomiting or use of other forms of compensation to avoid weight gain after binge eating; this cycle must be performed on a regular basis to be diagnosed as such. The non-purging type of bulimia involves the use of excessive exercise or dieting/fasting to prevent/avoid weight gain. <ref name="Academy">Academy for Eating Disorders. Web site: http:// www.aedweb.org/eating_disorders/index.cfm. Accessed February 2010.</ref> | Two types of bulimia nervosa have been defined. The purging type which involves self-induced vomiting or use of other forms of compensation to avoid weight gain after binge eating; this cycle must be performed on a regular basis to be diagnosed as such. The non-purging type of bulimia involves the use of excessive exercise or dieting/fasting to prevent/avoid weight gain. <ref name="Academy">Academy for Eating Disorders. Web site: http:// www.aedweb.org/eating_disorders/index.cfm. Accessed February 2010.</ref> | ||
== Prevalence == | == Prevalence == | ||
The incidence of people suffering from bulimia has increased over the last 30-40 years. Around 1 to 2% of females in late adolescence and adult women meet the diagnostic criteria for bulimia nervosa. <ref name="Academy" /> <br> | The incidence of people suffering from bulimia has increased over the last 30-40 years. Around 1 to 2% of females in late adolescence and adult women meet the diagnostic criteria for bulimia nervosa. <ref name="Academy" /><br> | ||
About 80% of people with bulimia nervosa are female. <ref name="National">National Eating Disorders Association. Web site: http://www.nationaleatingdisorders.org/nedaDir/files/documents/handouts/Bulimia.pdf. Accessed February 2010.</ref> | About 80% of people with bulimia nervosa are female. <ref name="National">National Eating Disorders Association. Web site: http://www.nationaleatingdisorders.org/nedaDir/files/documents/handouts/Bulimia.pdf. Accessed February 2010.</ref> | ||
== Characteristics/Clinical Presentation == | == Characteristics/Clinical Presentation == | ||
Bulimia can affect anyone: male, female, young, old, and all races. These patients can present with normal weight or they may be underweight or overweight. The patient may use pills (diet pills, diuretics, or laxitives). They may often take trips to the bathroom after eating (suggested that they use this time to purge after a meal) and may exercise despite weather, injury, or energy levels to control their weight. <ref name="Office on Women's Health" /> | Bulimia can affect anyone: male, female, young, old, and all races. These patients can present with normal weight or they may be underweight or overweight. The patient may use pills (diet pills, diuretics, or laxitives). They may often take trips to the bathroom after eating (suggested that they use this time to purge after a meal) and may exercise despite weather, injury, or energy levels to control their weight. <ref name="Office on Women's Health" /> | ||
Signs of binging include: the disappearance of large amounts of food in a short time period and finding wrappers/containers of consumed food around the person's living environment. <ref name="National" /><br> | Signs of binging include: the disappearance of large amounts of food in a short time period and finding wrappers/containers of consumed food around the person's living environment. <ref name="National" /><br> | ||
Signs of purging include: frequent trips to the bathroom after meals, signs or smells of vomiting, evidence of use of laxatives/diuretics (wrappers, containers, etc.), excessive and rigid exercise routines (continued despite weather, illness, injury, energy levels), rigid schedules that allow time for binge/purge cycles, withdrawal from normal activities, main focus and concern on weight loss, dieting, and controlling their food (intake/outtake). <ref name="National" /> | Signs of purging include: frequent trips to the bathroom after meals, signs or smells of vomiting, evidence of use of laxatives/diuretics (wrappers, containers, etc.), excessive and rigid exercise routines (continued despite weather, illness, injury, energy levels), rigid schedules that allow time for binge/purge cycles, withdrawal from normal activities, main focus and concern on weight loss, dieting, and controlling their food (intake/outtake). <ref name="National" /> | ||
Signs of self-induced vomiting include: swelling of the patient's cheeks/jaws, calluses or scrapes on the knuckles, clear-looking teeth, broken blood vessels in the eyes. Patients with bulimia nervosa may also present with other mental health problems such as depression, anxiety, substance abuse, distorted body image (thoughts and verbal expressions of hating body, image of being fat despite thin appearance, and fear of gaining weight), and reports from family and friends on activity not "normal" for the person (i.e. moody, sad, unsocialable). <ref name="Office on Women's Health" /> | Signs of self-induced vomiting include: swelling of the patient's cheeks/jaws, calluses or scrapes on the knuckles, clear-looking teeth, broken blood vessels in the eyes. Patients with bulimia nervosa may also present with other mental health problems such as depression, anxiety, substance abuse, distorted body image (thoughts and verbal expressions of hating body, image of being fat despite thin appearance, and fear of gaining weight), and reports from family and friends on activity not "normal" for the person (i.e. moody, sad, unsocialable). <ref name="Office on Women's Health" /> | ||
Physical signs and symptoms can include: weight loss/gain; muscle weakness and/or myopathy; chronic fatigue; dehydration or rebound water retention, pitting edema; discoloration of teeth, broken blood vessels in eyes, enlarged salivary glands, scrapes/calluses on dorsums of hands/fingers; inability to tolerate cold; irregular or absent menstrual cycles, delay in menses in young girls; dry skin and hair, hair loss, lanugo growth over entire body, brittle nails; reports of heartburn, gas, constipation, or diarrhea; slow heart rate and low blood pressure.<ref name="Differential ">Goodman CC & Snyder TE Differential Diagnosis for Physical Therapists: Screening for Referral. 4th ed. St. Louis, Missouri: Saunders Elsevier; 2007.</ref><br> | Physical signs and symptoms can include: weight loss/gain; muscle weakness and/or myopathy; chronic fatigue; dehydration or rebound water retention, pitting edema; discoloration of teeth, broken blood vessels in eyes, enlarged salivary glands, scrapes/calluses on dorsums of hands/fingers; inability to tolerate cold; irregular or absent menstrual cycles, delay in menses in young girls; dry skin and hair, hair loss, lanugo growth over entire body, brittle nails; reports of heartburn, gas, constipation, or diarrhea; slow heart rate and low blood pressure.<ref name="Differential">Goodman CC &amp; Snyder TE Differential Diagnosis for Physical Therapists: Screening for Referral. 4th ed. St. Louis, Missouri: Saunders Elsevier; 2007.</ref><br> | ||
Behavioral signs and symptoms can include: preoccupation with weight, food, calories, fat grams, dieting, clothing size, and body shape; personality changes (i.e. mood swings and irritability that may not have been present before); binging and purging behavoirs or food restriction behaviors; frequent trips to the bathroom after meals; distored body images (both thoughts and verbal expressions of dissatisfaction, despite thin body); excessive and rigid exercise routine; use of pills or other drugs to control weight (i.e. diuretics, laxatives, enemas, etc.). <ref name="Differential" /> | Behavioral signs and symptoms can include: preoccupation with weight, food, calories, fat grams, dieting, clothing size, and body shape; personality changes (i.e. mood swings and irritability that may not have been present before); binging and purging behavoirs or food restriction behaviors; frequent trips to the bathroom after meals; distored body images (both thoughts and verbal expressions of dissatisfaction, despite thin body); excessive and rigid exercise routine; use of pills or other drugs to control weight (i.e. diuretics, laxatives, enemas, etc.). <ref name="Differential" /> | ||
| Line 38: | Line 38: | ||
== Medications == | == Medications == | ||
add text here <br> | add text here <br> | ||
== Diagnostic Tests/Lab Tests/Lab Values == | == Diagnostic Tests/Lab Tests/Lab Values == | ||
In diagnosing bulimia nervosa, patients must meet specific criteria. Patients can NOT simultaneously meet the diagnostic criteria for anorexia nervosa. To meet the bulimia nervosa criteria, a patient binges and then engages in "inappropriate compensatory behavior at least twice weekly for at least three months." <ref name="Academy" /> | In diagnosing bulimia nervosa, patients must meet specific criteria. Patients can NOT simultaneously meet the diagnostic criteria for anorexia nervosa. To meet the bulimia nervosa criteria, a patient binges and then engages in "inappropriate compensatory behavior at least twice weekly for at least three months." <ref name="Academy" /> | ||
Other exams, such as dental exams, can help with identifying signs of excessive vomiting. Dental exams may reveal decrease enamel, cavities, and gum infection. Metabolic panels can show electrolyte imbalances and help identify dehydration. <ref name="Van">Van Voorhees BW, Zieve D. Bulimia: MedlinePlus Medical Encyclopedia. Last Updated Jan. 25, 2010. Available from: U.S. National Library of Medicine and the National Institutes of Health, Web site: http://www.nlm.nih.gov/medlineplus/ency/article/000341.htm. Accessed February 2010.</ref> | Other exams, such as dental exams, can help with identifying signs of excessive vomiting. Dental exams may reveal decrease enamel, cavities, and gum infection. Metabolic panels can show electrolyte imbalances and help identify dehydration. <ref name="Van">Van Voorhees BW, Zieve D. Bulimia: MedlinePlus Medical Encyclopedia. Last Updated Jan. 25, 2010. Available from: U.S. National Library of Medicine and the National Institutes of Health, Web site: http://www.nlm.nih.gov/medlineplus/ency/article/000341.htm. Accessed February 2010.</ref> | ||
== Causes == | == Causes == | ||
There have been no specific things proven to cause bulimia. Triggers to bulimia nervosa have been suggested, including dieting, stress, emotions, and the need for control (to ease stress or anxiety in a person's life). Factors that are suggested to contribute to bulimia include culture, family history, stressful life event, personality, and biology. <ref name="Office on Women's Health" /><br> | There have been no specific things proven to cause bulimia. Triggers to bulimia nervosa have been suggested, including dieting, stress, emotions, and the need for control (to ease stress or anxiety in a person's life). Factors that are suggested to contribute to bulimia include culture, family history, stressful life event, personality, and biology. <ref name="Office on Women's Health" /><br> | ||
Rarely it is one factor in causing bulimia, often it is found that genetics, psychological factors, family and societal pressures, and/or cultural influences. <ref name="Van" /> | Rarely it is one factor in causing bulimia, often it is found that genetics, psychological factors, family and societal pressures, and/or cultural influences. <ref name="Van" /> | ||
| Line 56: | Line 56: | ||
Complications from bulimia can include tears in the esophagus, inflammation of the throat, englarged glands near cheeks; pancreatitis,peptic ulcers, stomach damage; constipation and hemorrhoids; dental cavities and gum infections; dehydration and electrolyte imbalances; irregular heartbeat, heart failure, and death can occur secondary to the imbalances due to loss of essential nutrients and electrolyte imbalances. <ref name="Van" /><ref name="US Dept">United States Department of Health and Human Services- Substance Abuse and Mental Health Services Administration, Available at: http://mentalhealth.samhsa.gov/publications/allpubs/ken98-0047/default.asp#4. Accessed February 2010.</ref> | Complications from bulimia can include tears in the esophagus, inflammation of the throat, englarged glands near cheeks; pancreatitis,peptic ulcers, stomach damage; constipation and hemorrhoids; dental cavities and gum infections; dehydration and electrolyte imbalances; irregular heartbeat, heart failure, and death can occur secondary to the imbalances due to loss of essential nutrients and electrolyte imbalances. <ref name="Van" /><ref name="US Dept">United States Department of Health and Human Services- Substance Abuse and Mental Health Services Administration, Available at: http://mentalhealth.samhsa.gov/publications/allpubs/ken98-0047/default.asp#4. Accessed February 2010.</ref> | ||
<br> | |||
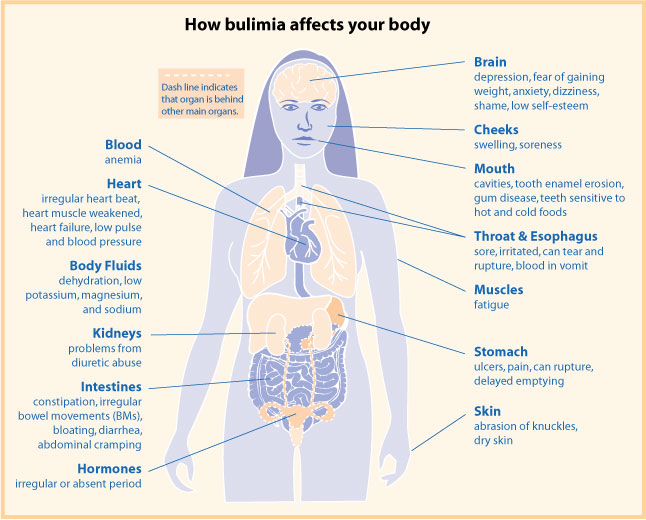
A diagram from womenshealth.gov, showing how builimia can result in complications throughout your body: | |||
[[Image:Bulimiafaqdia.jpg]] | |||
[[Image:Bulimiafaqdia.jpg]] | |||
== Medical Management (current best evidence) == | == Medical Management (current best evidence) == | ||
Typical treatment for people with bulimia nervosa includes a multi-disciplinary approach; a treatment team usually involves a primary care physician, a dietician/nutritionist, a mental health professional, as well as nurses and other supportive medical personnel. <ref name="Academy " /> | Typical treatment for people with bulimia nervosa includes a multi-disciplinary approach; a treatment team usually involves a primary care physician, a dietician/nutritionist, a mental health professional, as well as nurses and other supportive medical personnel. <ref name="Academy" /> | ||
The treatment process: the initial assessment addresses the patient's past medical history, current symptoms, current physical and mental status, the way the patient controls their weight, and any psychiatric issues/disorders (i.e. depression, anxiety, etc.). A physician and dietician are consulted, developing a diagnosis and place of care for the patient. Most people with bulimia are treated on an outpatient basis; however their treatment is coordinated between their physician, psychotherapist, and dietician. <ref name="Academy " /> | The treatment process: the initial assessment addresses the patient's past medical history, current symptoms, current physical and mental status, the way the patient controls their weight, and any psychiatric issues/disorders (i.e. depression, anxiety, etc.). A physician and dietician are consulted, developing a diagnosis and place of care for the patient. Most people with bulimia are treated on an outpatient basis; however their treatment is coordinated between their physician, psychotherapist, and dietician. <ref name="Academy" /> | ||
Some patients choose to be treated without mental health professionals, while others only recieve treatment from mental health professionals. Psychotherapy includes cognitive-behavoiral therapy, behavior therapy, family therapy, and interpersonal psychotherapy. Some patients are successful with short-term treatments such as these, others require long-term.<ref name="Academy" /> | Some patients choose to be treated without mental health professionals, while others only recieve treatment from mental health professionals. Psychotherapy includes cognitive-behavoiral therapy, behavior therapy, family therapy, and interpersonal psychotherapy. Some patients are successful with short-term treatments such as these, others require long-term.<ref name="Academy" /> | ||
Some patients are treated with psychopharmacology. Psychiatric medications have been found to be successful in treating patients with bulimia; these medications often include anti-depressants. <ref name="Academy " /> | Some patients are treated with psychopharmacology. Psychiatric medications have been found to be successful in treating patients with bulimia; these medications often include anti-depressants. <ref name="Academy" /> | ||
Nutritional counseling is also a treatment option and a vital component for patients diagnosed with an eating disorder. Dieticians serves as educatiors to both the patient and their families. Dieticians help patients with bulimia to normalize their eating behaviors. <ref name="Academy " /> | Nutritional counseling is also a treatment option and a vital component for patients diagnosed with an eating disorder. Dieticians serves as educatiors to both the patient and their families. Dieticians help patients with bulimia to normalize their eating behaviors. <ref name="Academy" /> | ||
Some patients diagnosed with bulimia have complications secondary to their disorder, thus requiring treatment beyond that for their eating disorder. These treatments vary according to the severity of systemic involvement and complications. <ref name="Academy " /> | Some patients diagnosed with bulimia have complications secondary to their disorder, thus requiring treatment beyond that for their eating disorder. These treatments vary according to the severity of systemic involvement and complications. <ref name="Academy" /> | ||
In more severe cases of bulimia, patients require in-patient treatment. This treatment provides the patient with a more structured environment, providing treatment and monitoring twenty-four hours a day, every day of the week. These programs are often arranged in a "step up" and "step down" levels allowing patients to progress (or for some, regress) in their treatment accordingly. For patients that need it, long-term in-patient programs are also available (i.e. residential treatment programs). <ref name="Academy " /> | In more severe cases of bulimia, patients require in-patient treatment. This treatment provides the patient with a more structured environment, providing treatment and monitoring twenty-four hours a day, every day of the week. These programs are often arranged in a "step up" and "step down" levels allowing patients to progress (or for some, regress) in their treatment accordingly. For patients that need it, long-term in-patient programs are also available (i.e. residential treatment programs). <ref name="Academy" /> | ||
== Physical Therapy Management (current best evidence) == | == Physical Therapy Management (current best evidence) == | ||
Physical therapists working under the practice patterns of "4A Primary Prevention/Risk Reduction for Skeletal Demineralization, 4B Impaired Posture, 4C Impaired Muscle Performance (especially with malnutrition and fluid/electrolyte disturbances), 6A Primary Prevention/Risk Reduction for Cardiovascular/Pulmonary Disorders, 6B Impaired Aerobic Capacity/Endurance Associated with De-conditioning, 7A Primary Prevention/Risk Reduction for Integumentary Disorders (malnutrition)" can help in the treatment of patients with bulimia nervosa. <ref name="APTA">American Physical Therapy Association. Guide to Physical Therapist Practice. 2nd ed. Alexandria, Virginia: American Physical Therapy Association; 2003.</ref><br> | Physical therapists working under the practice patterns of "4A Primary Prevention/Risk Reduction for Skeletal Demineralization, 4B Impaired Posture, 4C Impaired Muscle Performance (especially with malnutrition and fluid/electrolyte disturbances), 6A Primary Prevention/Risk Reduction for Cardiovascular/Pulmonary Disorders, 6B Impaired Aerobic Capacity/Endurance Associated with De-conditioning, 7A Primary Prevention/Risk Reduction for Integumentary Disorders (malnutrition)" can help in the treatment of patients with bulimia nervosa. <ref name="APTA">American Physical Therapy Association. Guide to Physical Therapist Practice. 2nd ed. Alexandria, Virginia: American Physical Therapy Association; 2003.</ref><br> | ||
According to the Guide for Physical Therapist Practice, physical therapists work preventatively or retrospectively with patients suffering from complications secondary to eating disorders. Some physical therapists may treat a person, who in addition to having an orthopedic problem for example, also has an eating disorder (whether known to the therapist or not). <ref name="Pathology">Goodman CC &amp; Fuller KS Pathology: Implications for the Physical Therapist. 3rd ed. St. Louis, Missouri: Saunders Elsevier; 2009.</ref><br> | According to the Guide for Physical Therapist Practice, physical therapists work preventatively or retrospectively with patients suffering from complications secondary to eating disorders. Some physical therapists may treat a person, who in addition to having an orthopedic problem for example, also has an eating disorder (whether known to the therapist or not). <ref name="Pathology">Goodman CC &amp;amp; Fuller KS Pathology: Implications for the Physical Therapist. 3rd ed. St. Louis, Missouri: Saunders Elsevier; 2009.</ref><br> | ||
Physical therapists can help with early screening and detection of and for eating disorders. The more informed a clinician can be, the more they are able to provide appropriate evaluations and interventions for their patients, helping to decrease the consequences and complications of the eating disorder. Recognizing at risk patient populations can also help with early detection; i.e. young, female athletes are at a higher risk for the female athlete triad. <ref name="Pathology" /><br> | Physical therapists can help with early screening and detection of and for eating disorders. The more informed a clinician can be, the more they are able to provide appropriate evaluations and interventions for their patients, helping to decrease the consequences and complications of the eating disorder. Recognizing at risk patient populations can also help with early detection; i.e. young, female athletes are at a higher risk for the female athlete triad. <ref name="Pathology" /><br> | ||
At risk patient populations can include females, those with a perfectionist personality, Caucasians, personal and/or family history of eating disoders or obesity, athletes, and patients with a history of trauma or sexual abuse. As a physical therapist, recognizing and being aware of patients with a distorted body image or distorted eating habits is also important. Some athletes who compete under weight classes or must build up their bodies for competition can be at risk for developing eating disorders. <ref name="Differential" /><br> | At risk patient populations can include females, those with a perfectionist personality, Caucasians, personal and/or family history of eating disoders or obesity, athletes, and patients with a history of trauma or sexual abuse. As a physical therapist, recognizing and being aware of patients with a distorted body image or distorted eating habits is also important. Some athletes who compete under weight classes or must build up their bodies for competition can be at risk for developing eating disorders. <ref name="Differential" /><br> | ||
Some questions to consider as physical therapists screening for eating disorders include: <br> | Some questions to consider as physical therapists screening for eating disorders include: <br> | ||
"• Area you satisfied with your eating patterns?<br> • Do you force yourself to exercises, even when you don’t feel well? <br> • Do you exercise more when you eat more? <br> • Do you think you will gain weight if you stop exercising for a day or two? <br> • Do you exercise more than once a day? <br> • Do you take laxatives/diuretics/any other pills as a way to control your weight or shape? <br> • Do you ever eat in secret (i.e. in closets or bathrooms to avoid being seen eating)?<br> • Are there days when you don’t eat anything? <br> • Do you ever make yourself throw up after eating as a way to control your weight?"<ref name="Differential" /> | "• Area you satisfied with your eating patterns?<br> • Do you force yourself to exercises, even when you don’t feel well? <br> • Do you exercise more when you eat more? <br> • Do you think you will gain weight if you stop exercising for a day or two? <br> • Do you exercise more than once a day? <br> • Do you take laxatives/diuretics/any other pills as a way to control your weight or shape? <br> • Do you ever eat in secret (i.e. in closets or bathrooms to avoid being seen eating)?<br> • Are there days when you don’t eat anything? <br> • Do you ever make yourself throw up after eating as a way to control your weight?"<ref name="Differential" /> | ||
Bulimia impacts a patient's fluid and electrolyte balance, putting them at risk for fluid depletion and ineffective temperature regulation. These, in addition to the use of self-induced vomiting or laxatives, can put the patient at a very high risk for dehydration and loss of potassium. Patients with these complications may initially present with muscle cramping, fatigue, as well as orthostatic hypotension. A physical therapist may have to hold treatment of their patient until fluid and electrolyte imbalances are normalized. It is important that the physical therapist encourage their patient to drink plenty of fluids and reduce their activity until levels are normalized. Patients with severe dehydration and electrolyte imbalances may present with confusion, disorientation, uncoordinated movements. These patients should be sent for immediate medical attention. <ref name="Pathology" /><br> | Bulimia impacts a patient's fluid and electrolyte balance, putting them at risk for fluid depletion and ineffective temperature regulation. These, in addition to the use of self-induced vomiting or laxatives, can put the patient at a very high risk for dehydration and loss of potassium. Patients with these complications may initially present with muscle cramping, fatigue, as well as orthostatic hypotension. A physical therapist may have to hold treatment of their patient until fluid and electrolyte imbalances are normalized. It is important that the physical therapist encourage their patient to drink plenty of fluids and reduce their activity until levels are normalized. Patients with severe dehydration and electrolyte imbalances may present with confusion, disorientation, uncoordinated movements. These patients should be sent for immediate medical attention. <ref name="Pathology" /><br> | ||
<br> | <br> | ||
| Line 106: | Line 106: | ||
== Case Reports == | == Case Reports == | ||
add links to case studies here (case studies should be added on new pages using the [[Template:Case Study|case study template]])<br> | add links to case studies here (case studies should be added on new pages using the [[Template:Case Study|case study template]])<br> | ||
== Resources <br> | == Resources <br> == | ||
add appropriate resources here | add appropriate resources here | ||
| Line 116: | Line 116: | ||
see tutorial on [[Adding PubMed Feed|Adding PubMed Feed]] | see tutorial on [[Adding PubMed Feed|Adding PubMed Feed]] | ||
<div class="researchbox"> | <div class="researchbox"> | ||
<rss>Feed goes here!!|charset=UTF-8|short|max=10</rss> | <rss>Feed goes here!!|charset=UTF-8|short|max=10</rss> | ||
</div> | </div> | ||
== References == | == References == | ||
| Line 123: | Line 123: | ||
<references /> | <references /> | ||
[[Category:Bellarmine_Student_Project]] | |||
Revision as of 02:57, 17 March 2010
Original Editors - Nikki Gee from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Lead Editors - Your name will be added here if you are a lead editor on this page. Read more.
Definition/Description[edit | edit source]
A condition during which a person eats a large amount of food in a short amount of time (binges), then uses some method of purging to avoid weight gain. Methods of purging include self-induced vomiting, use of laxatives or diuretics, and excessive exercise. [1]
Two types of bulimia nervosa have been defined. The purging type which involves self-induced vomiting or use of other forms of compensation to avoid weight gain after binge eating; this cycle must be performed on a regular basis to be diagnosed as such. The non-purging type of bulimia involves the use of excessive exercise or dieting/fasting to prevent/avoid weight gain. [2]
Prevalence[edit | edit source]
The incidence of people suffering from bulimia has increased over the last 30-40 years. Around 1 to 2% of females in late adolescence and adult women meet the diagnostic criteria for bulimia nervosa. [2]
About 80% of people with bulimia nervosa are female. [3]
Characteristics/Clinical Presentation[edit | edit source]
Bulimia can affect anyone: male, female, young, old, and all races. These patients can present with normal weight or they may be underweight or overweight. The patient may use pills (diet pills, diuretics, or laxitives). They may often take trips to the bathroom after eating (suggested that they use this time to purge after a meal) and may exercise despite weather, injury, or energy levels to control their weight. [1]
Signs of binging include: the disappearance of large amounts of food in a short time period and finding wrappers/containers of consumed food around the person's living environment. [3]
Signs of purging include: frequent trips to the bathroom after meals, signs or smells of vomiting, evidence of use of laxatives/diuretics (wrappers, containers, etc.), excessive and rigid exercise routines (continued despite weather, illness, injury, energy levels), rigid schedules that allow time for binge/purge cycles, withdrawal from normal activities, main focus and concern on weight loss, dieting, and controlling their food (intake/outtake). [3]
Signs of self-induced vomiting include: swelling of the patient's cheeks/jaws, calluses or scrapes on the knuckles, clear-looking teeth, broken blood vessels in the eyes. Patients with bulimia nervosa may also present with other mental health problems such as depression, anxiety, substance abuse, distorted body image (thoughts and verbal expressions of hating body, image of being fat despite thin appearance, and fear of gaining weight), and reports from family and friends on activity not "normal" for the person (i.e. moody, sad, unsocialable). [1]
Physical signs and symptoms can include: weight loss/gain; muscle weakness and/or myopathy; chronic fatigue; dehydration or rebound water retention, pitting edema; discoloration of teeth, broken blood vessels in eyes, enlarged salivary glands, scrapes/calluses on dorsums of hands/fingers; inability to tolerate cold; irregular or absent menstrual cycles, delay in menses in young girls; dry skin and hair, hair loss, lanugo growth over entire body, brittle nails; reports of heartburn, gas, constipation, or diarrhea; slow heart rate and low blood pressure.[4]
Behavioral signs and symptoms can include: preoccupation with weight, food, calories, fat grams, dieting, clothing size, and body shape; personality changes (i.e. mood swings and irritability that may not have been present before); binging and purging behavoirs or food restriction behaviors; frequent trips to the bathroom after meals; distored body images (both thoughts and verbal expressions of dissatisfaction, despite thin body); excessive and rigid exercise routine; use of pills or other drugs to control weight (i.e. diuretics, laxatives, enemas, etc.). [4]
Associated Co-morbidities[edit | edit source]
Often times bulimia nervosa is also associated with mental health disorders such as depression, anxiety, and substance abuse. [1]
Medications[edit | edit source]
add text here
Diagnostic Tests/Lab Tests/Lab Values[edit | edit source]
In diagnosing bulimia nervosa, patients must meet specific criteria. Patients can NOT simultaneously meet the diagnostic criteria for anorexia nervosa. To meet the bulimia nervosa criteria, a patient binges and then engages in "inappropriate compensatory behavior at least twice weekly for at least three months." [2]
Other exams, such as dental exams, can help with identifying signs of excessive vomiting. Dental exams may reveal decrease enamel, cavities, and gum infection. Metabolic panels can show electrolyte imbalances and help identify dehydration. [5]
Causes[edit | edit source]
There have been no specific things proven to cause bulimia. Triggers to bulimia nervosa have been suggested, including dieting, stress, emotions, and the need for control (to ease stress or anxiety in a person's life). Factors that are suggested to contribute to bulimia include culture, family history, stressful life event, personality, and biology. [1]
Rarely it is one factor in causing bulimia, often it is found that genetics, psychological factors, family and societal pressures, and/or cultural influences. [5]
Systemic Involvement[edit | edit source]
Complications from bulimia can include tears in the esophagus, inflammation of the throat, englarged glands near cheeks; pancreatitis,peptic ulcers, stomach damage; constipation and hemorrhoids; dental cavities and gum infections; dehydration and electrolyte imbalances; irregular heartbeat, heart failure, and death can occur secondary to the imbalances due to loss of essential nutrients and electrolyte imbalances. [5][6]
A diagram from womenshealth.gov, showing how builimia can result in complications throughout your body:
Medical Management (current best evidence)[edit | edit source]
Typical treatment for people with bulimia nervosa includes a multi-disciplinary approach; a treatment team usually involves a primary care physician, a dietician/nutritionist, a mental health professional, as well as nurses and other supportive medical personnel. [2]
The treatment process: the initial assessment addresses the patient's past medical history, current symptoms, current physical and mental status, the way the patient controls their weight, and any psychiatric issues/disorders (i.e. depression, anxiety, etc.). A physician and dietician are consulted, developing a diagnosis and place of care for the patient. Most people with bulimia are treated on an outpatient basis; however their treatment is coordinated between their physician, psychotherapist, and dietician. [2]
Some patients choose to be treated without mental health professionals, while others only recieve treatment from mental health professionals. Psychotherapy includes cognitive-behavoiral therapy, behavior therapy, family therapy, and interpersonal psychotherapy. Some patients are successful with short-term treatments such as these, others require long-term.[2]
Some patients are treated with psychopharmacology. Psychiatric medications have been found to be successful in treating patients with bulimia; these medications often include anti-depressants. [2]
Nutritional counseling is also a treatment option and a vital component for patients diagnosed with an eating disorder. Dieticians serves as educatiors to both the patient and their families. Dieticians help patients with bulimia to normalize their eating behaviors. [2]
Some patients diagnosed with bulimia have complications secondary to their disorder, thus requiring treatment beyond that for their eating disorder. These treatments vary according to the severity of systemic involvement and complications. [2]
In more severe cases of bulimia, patients require in-patient treatment. This treatment provides the patient with a more structured environment, providing treatment and monitoring twenty-four hours a day, every day of the week. These programs are often arranged in a "step up" and "step down" levels allowing patients to progress (or for some, regress) in their treatment accordingly. For patients that need it, long-term in-patient programs are also available (i.e. residential treatment programs). [2]
Physical Therapy Management (current best evidence)[edit | edit source]
Physical therapists working under the practice patterns of "4A Primary Prevention/Risk Reduction for Skeletal Demineralization, 4B Impaired Posture, 4C Impaired Muscle Performance (especially with malnutrition and fluid/electrolyte disturbances), 6A Primary Prevention/Risk Reduction for Cardiovascular/Pulmonary Disorders, 6B Impaired Aerobic Capacity/Endurance Associated with De-conditioning, 7A Primary Prevention/Risk Reduction for Integumentary Disorders (malnutrition)" can help in the treatment of patients with bulimia nervosa. [7]
According to the Guide for Physical Therapist Practice, physical therapists work preventatively or retrospectively with patients suffering from complications secondary to eating disorders. Some physical therapists may treat a person, who in addition to having an orthopedic problem for example, also has an eating disorder (whether known to the therapist or not). [8]
Physical therapists can help with early screening and detection of and for eating disorders. The more informed a clinician can be, the more they are able to provide appropriate evaluations and interventions for their patients, helping to decrease the consequences and complications of the eating disorder. Recognizing at risk patient populations can also help with early detection; i.e. young, female athletes are at a higher risk for the female athlete triad. [8]
At risk patient populations can include females, those with a perfectionist personality, Caucasians, personal and/or family history of eating disoders or obesity, athletes, and patients with a history of trauma or sexual abuse. As a physical therapist, recognizing and being aware of patients with a distorted body image or distorted eating habits is also important. Some athletes who compete under weight classes or must build up their bodies for competition can be at risk for developing eating disorders. [4]
Some questions to consider as physical therapists screening for eating disorders include:
"• Area you satisfied with your eating patterns?
• Do you force yourself to exercises, even when you don’t feel well?
• Do you exercise more when you eat more?
• Do you think you will gain weight if you stop exercising for a day or two?
• Do you exercise more than once a day?
• Do you take laxatives/diuretics/any other pills as a way to control your weight or shape?
• Do you ever eat in secret (i.e. in closets or bathrooms to avoid being seen eating)?
• Are there days when you don’t eat anything?
• Do you ever make yourself throw up after eating as a way to control your weight?"[4]
Bulimia impacts a patient's fluid and electrolyte balance, putting them at risk for fluid depletion and ineffective temperature regulation. These, in addition to the use of self-induced vomiting or laxatives, can put the patient at a very high risk for dehydration and loss of potassium. Patients with these complications may initially present with muscle cramping, fatigue, as well as orthostatic hypotension. A physical therapist may have to hold treatment of their patient until fluid and electrolyte imbalances are normalized. It is important that the physical therapist encourage their patient to drink plenty of fluids and reduce their activity until levels are normalized. Patients with severe dehydration and electrolyte imbalances may present with confusion, disorientation, uncoordinated movements. These patients should be sent for immediate medical attention. [8]
Alternative/Holistic Management (current best evidence)[edit | edit source]
add text here
Differential Diagnosis[edit | edit source]
add text here
Case Reports[edit | edit source]
add links to case studies here (case studies should be added on new pages using the case study template)
Resources
[edit | edit source]
add appropriate resources here
Recent Related Research (from Pubmed)[edit | edit source]
see tutorial on Adding PubMed Feed
Extension:RSS -- Error: Not a valid URL: Feed goes here!!|charset=UTF-8|short|max=10
References[edit | edit source]
see adding references tutorial.
- ↑ 1.0 1.1 1.2 1.3 1.4 Office on Women's Health in the U.S. Department of Health and Human Services. 2009. Available from: U.S. Department of Health and Human Services, Web site: http://www.womenshealth.gov/faq/bulimia-nervosa.cfm. Accessed February 2010.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 2.8 2.9 Academy for Eating Disorders. Web site: http:// www.aedweb.org/eating_disorders/index.cfm. Accessed February 2010.
- ↑ 3.0 3.1 3.2 National Eating Disorders Association. Web site: http://www.nationaleatingdisorders.org/nedaDir/files/documents/handouts/Bulimia.pdf. Accessed February 2010.
- ↑ 4.0 4.1 4.2 4.3 Goodman CC & Snyder TE Differential Diagnosis for Physical Therapists: Screening for Referral. 4th ed. St. Louis, Missouri: Saunders Elsevier; 2007.
- ↑ 5.0 5.1 5.2 Van Voorhees BW, Zieve D. Bulimia: MedlinePlus Medical Encyclopedia. Last Updated Jan. 25, 2010. Available from: U.S. National Library of Medicine and the National Institutes of Health, Web site: http://www.nlm.nih.gov/medlineplus/ency/article/000341.htm. Accessed February 2010.
- ↑ United States Department of Health and Human Services- Substance Abuse and Mental Health Services Administration, Available at: http://mentalhealth.samhsa.gov/publications/allpubs/ken98-0047/default.asp#4. Accessed February 2010.
- ↑ American Physical Therapy Association. Guide to Physical Therapist Practice. 2nd ed. Alexandria, Virginia: American Physical Therapy Association; 2003.
- ↑ 8.0 8.1 8.2 Goodman CC &amp; Fuller KS Pathology: Implications for the Physical Therapist. 3rd ed. St. Louis, Missouri: Saunders Elsevier; 2009.