Bowel Considerations with Spinal Cord Injury: Difference between revisions
No edit summary |
m (Protected "Bowel Considerations in Spinal Cord Injury" ([Edit=⧼protect-level-ppadmin⧽] (indefinite) [Move=⧼protect-level-ppadmin⧽] (indefinite))) |
(No difference)
| |
Revision as of 00:10, 21 January 2024
Original Editor - Wendy Oelofse
Top Contributors - Ewa Jaraczewska, Jess Bell and Kim Jackson
Introduction[edit | edit source]
The pattern of bowel dysfunction varies depending on the level of injury. The complications of neurogenic bowel dysfunction include constipation, obstructive defecation, and faecal incontinence.[1] Bowel dysfunction can cause significant restrictions in a person's social activities and quality of life. [2] There is no single program that can work for every patient, but the bladder and bowel dysfunction management program is a fundamental step following the initial spinal cord injury.
This article supplies additional information for the Bladder and Bowel Consideration with Spinal Cord Injury course.
Bowel Dysfunction in Spinal Cord Injury[edit | edit source]
Patient's symptoms in neurogenic bowel dysfunction vary depending on the injury level. One author defines three neuropathological patterns in patient with a complete spinal cord injury:[3]
- Patter A: Patients with spinal cord injury above T7
- Loss of voluntary control of abdominal muscles
- Preserved spinal sacral reflexes
- Pattern B: Patients with spinal cord injury below T7
- Voluntary control of abdominal muscles
- Preserved sacral reflexes
- Pattern C: Patients with spinal cord injury below T7
- Voluntary control of abdominal muscles
- Absent sacral reflexes.
Another classification defines two types of neurogenic bowel:[4]
- Spastic bowel
- Flaccid bowel
Spastic Bowel[edit | edit source]
- Observed in people with an SCI above T12 (Upper motor neuron SCI)
- Loss of feeling the need to have a bowel movement
- Loss or impairment of voluntary control of the external anal sphincter
- The reflex that makes the stool move out of the body is intact and can be stimulated
- Complications include constipation, usually with faecal retention, but uncontrolled evacuation of the rectum can occur.
Flaccid Bowel[edit | edit source]
- Observed in people with a SCI below T12 (Lower motor neurone SCI)
- Loss of feeling the need to have a bowel movement
- Loss or impairment of voluntary control of the external anal sphincter
- Loss of the bowel reflex. The rectum cannot easily empty itself, and the sphincter muscles may relax and stay open.
- Complications include constipation and incontinence
Bristol Scale[edit | edit source]
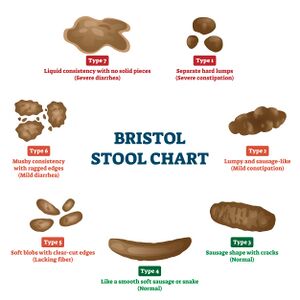
The Bristol scale or Bristol Stool Chart is an assessment tool used by healthcare professionals and designed to classify stools. It helps to diagnose constipation, diarrhoea and irritable bowel syndrome.
Type 1 through 7 indicates the following:
- Type 1-2 indicate constipation
- Type 3-4 indicate ideal stools
- Type 5-7 may indicate diarrhoea and urgency
Management of Bowel Dysfunction[edit | edit source]
"The overall goal of bowel management is to achieve secondary continence with regular and sufficient bowel emptying within an individually acceptable time frame and at the right time according to the patient’s agenda."[5]
The literature does not support one bowel management program for patients with spinal cord injury. A multidisciplinary team should assess each patient and choose the strategy that
Spastic Bowel Management[edit | edit source]
The following strategies are recommended to manage spastic bowel:
- Bowel routine
- Empty every other day or 3x/week
- It should take no longer than 1 hour.
- Suppository
- Bisacodyl and glycerin are the most common active ingredients in suppositories
- Oral laxatives can become a component of bowel management programs
- Digital rectal stimulation
- Gloved finger is inserted into the anorectal canal
- The goal is to enhance contractions of the descending colon and rectum, which helps with bowel evacuation
- Abdominal massage
- It takes about 15 minutes
- The goal is to decrease colonic transit time, reduce abdominal distension and increase the frequency of bowel movements per week
Watch the video demonstrating abdominal massage to manage constipation:
Flaccid Bowel Mangement[edit | edit source]
The following strategies are recommended to manage flaccid bowel:
- Bowel routine
- Digital removal
- Suppositories
- Balanced diet and the use of medication to maintain stool consistency
- Transanal irrigation
- Transanal irrigation system includes a coated rectal balloon catheter, manual pump, and a water container.[7]
- It involves inserting a balloon catheter into the rectum and slowly administering warm tap water in volumes, usually between 500 and 1,000 mL. [1]
- The system makes it possible to handle the irrigation procedure without assistance from another person.[7]
- Immobilized patients and patients with poor hand function can use the system.[7]
- The result includes fewer patients' complaints of constipation, less faecal incontinence, improved symptom-related quality of life, and reduced time consumption on bowel management procedures.[7]
Resources[edit | edit source]
- Kurze I, Geng V, Böthig R. Guideline for the management of neurogenic bowel dysfunction in spinal cord injury/disease. Spinal Cord. 2022 May;60(5):435-443.
References[edit | edit source]
- ↑ 1.0 1.1 Hughes M. Bowel management in spinal cord injury patients. Clin Colon Rectal Surg. 2014 Sep;27(3):113-5
- ↑ Khadour FA, Khadour YA, Xu J, Meng L, Cui L, Xu T. Effect of neurogenic bowel dysfunction symptoms on quality of life after a spinal cord injury. J Orthop Surg Res 2023; 18(458).
- ↑ Vallès M, Terré R, Guevara D, Portell E, Vidal J, Mearin F. Alteraciones de la función intestinal en pacientes con lesión medular: relación con las características neurológicas de la lesión [Bowel dysfunction in patients with spinal cord injury: relation with neurological patterns]. Med Clin (Barc). 2007 Jun 30;129(5):171-3. Spanish.
- ↑ Oelofse W. Bladder and Bowel Dysfunction in Spinal Cord Injury. Plus Course 2024
- ↑ Kurze I, Geng V, Böthig R. Guideline for the management of neurogenic bowel dysfunction in spinal cord injury/disease. Spinal Cord. 2022 May;60(5):435-443.
- ↑ Rehab and Revive. How to Massage Out Your Stuck Poop | FIX CONSTIPATION. Available from: https://www.youtube.com/watch?v=kqWEwOPXfOI [last accessed 20/01/2024]
- ↑ 7.0 7.1 7.2 7.3 Christensen P, Bazzocchi G, Coggrave M, Abel R, Hultling C, Krogh K, Media S, Laurberg S. A randomized, controlled trial of transanal irrigation versus conservative bowel management in spinal cord-injured patients. Gastroenterology. 2006 Sep;131(3):738-47.