Bowel Considerations with Spinal Cord Injury: Difference between revisions
No edit summary |
No edit summary |
||
| Line 11: | Line 11: | ||
== Bowel Dysfunction in Spinal Cord Injury == | == Bowel Dysfunction in Spinal Cord Injury == | ||
Patient's symptoms in neurogenic bowel dysfunction vary depending on the injury level. One classification defines three neuropathological patterns in patient with a complete spinal cord injury:<ref>Vallès M, Terré R, Guevara D, Portell E, Vidal J, Mearin F. Alteraciones de la función intestinal en pacientes con lesión medular: relación con las características neurológicas de la lesión [Bowel dysfunction in patients with spinal cord injury: relation with neurological patterns]. Med Clin (Barc). 2007 Jun 30;129(5):171-3. Spanish.</ref> | |||
* Patter A: Patients with spinal cord injury above T7 | |||
** Loss of voluntary control of abdominal muscles | |||
** Preserved spinal sacral reflexes | |||
* Pattern B: Patients with spinal cord injury below T7 | |||
** Voluntary control of abdominal muscles | |||
** Preserved sacral reflexes | |||
* Pattern C: Patients with spinal cord injury below T7 | |||
** Voluntary control of abdominal muscles | |||
** Absent sacral reflexes. | |||
===Spastic Bowel=== | ===Spastic Bowel=== | ||
| Line 31: | Line 42: | ||
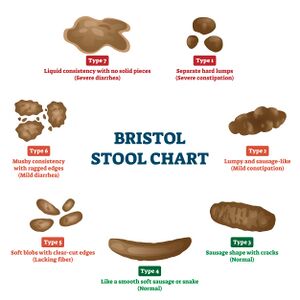
==Bristol Scale== | ==Bristol Scale== | ||
Bristol scale or Bristol Stool Chart is an assessment tool used by healthcare professionals and | Bristol scale or Bristol Stool Chart is an assessment tool used by healthcare professionals and designed to classify stools. It helps to diagnose constipation, diarrhoea and irritable bowel syndrome. | ||
Type 1 through 7 indicates the following: | |||
* Type 1-2 indicate constipation | |||
* Type 3-4 indicate ideal stools | |||
* Type 5-7 may indicate diarrhoea and urgency | |||
==Management of Bowel Dysfunction== | ==Management of Bowel Dysfunction== | ||
| Line 37: | Line 54: | ||
===Spastic Bowel Management=== | ===Spastic Bowel Management=== | ||
The following strategies are recommended to manage spastic bowel: | |||
* Routine | |||
* Suppository | |||
* Digital rectal stimulation | |||
* Abdominal massage | |||
===Flaccid Bowel Mangement=== | ===Flaccid Bowel Mangement=== | ||
== Resources == | == Resources == | ||
| Line 44: | Line 68: | ||
<references /> | <references /> | ||
[[Category:Spinal Cord Injuries]] | |||
[[Category:ADL]] | |||
Revision as of 22:43, 20 January 2024
Original Editor - User Name
Top Contributors - Ewa Jaraczewska, Jess Bell and Kim Jackson
Introduction[edit | edit source]
The pattern of bowel dysfunction varies depending on the level of injury. The complications of neurogenic bowel dysfunction include constipation, obstructive defecation, and fecal incontinence.[1] Bowel dysfunction can cause major restrictions in person's social activities and quality of life. [2] There is no single program that can work for every patient, but bladder and bowel dysfunction management program is a fundamental step following the initial spinal cord injury.
This article supplies additional information for the Bladder and Bowel Consideration with Spinal Cord Injury course.
Bowel Dysfunction in Spinal Cord Injury[edit | edit source]
Patient's symptoms in neurogenic bowel dysfunction vary depending on the injury level. One classification defines three neuropathological patterns in patient with a complete spinal cord injury:[3]
- Patter A: Patients with spinal cord injury above T7
- Loss of voluntary control of abdominal muscles
- Preserved spinal sacral reflexes
- Pattern B: Patients with spinal cord injury below T7
- Voluntary control of abdominal muscles
- Preserved sacral reflexes
- Pattern C: Patients with spinal cord injury below T7
- Voluntary control of abdominal muscles
- Absent sacral reflexes.
Spastic Bowel[edit | edit source]
- Observed in people with a SCI above T12 (Upper motor neuron SCI)
- Loss of feel the need to have a bowel movement
- Loss or impairment of voluntary control of the external anal sphincter
- The reflex that makes stool move out of the body is intact and can be stimulated
- Complications include constipation usually with faecal retention but uncontrolled evacuation of the rectum can occur.
Flaccid Bowel[edit | edit source]
- Observed in people with a SCI below T12 (Lower motor neurone SCI)
- Loss of feel the need to have a bowel movement
- Loss or impairment of voluntary control of the external anal sphincter
- Loss of the bowel reflex . The rectum cannot easily empty by itself and the sphincter muscles may relax and stay open.
- Complications include constipation and incontinence
Bristol Scale[edit | edit source]
Bristol scale or Bristol Stool Chart is an assessment tool used by healthcare professionals and designed to classify stools. It helps to diagnose constipation, diarrhoea and irritable bowel syndrome.
Type 1 through 7 indicates the following:
- Type 1-2 indicate constipation
- Type 3-4 indicate ideal stools
- Type 5-7 may indicate diarrhoea and urgency
Management of Bowel Dysfunction[edit | edit source]
"The overall goal of bowel management is to achieve secondary continence with regular and sufficient bowel emptying within an individually acceptable time frame and at the right time according to the patient’s agenda."[4]
Spastic Bowel Management[edit | edit source]
The following strategies are recommended to manage spastic bowel:
- Routine
- Suppository
- Digital rectal stimulation
- Abdominal massage
Flaccid Bowel Mangement[edit | edit source]
Resources[edit | edit source]
- Kurze I, Geng V, Böthig R. Guideline for the management of neurogenic bowel dysfunction in spinal cord injury/disease. Spinal Cord. 2022 May;60(5):435-443.
References[edit | edit source]
- ↑ Hughes M. Bowel management in spinal cord injury patients. Clin Colon Rectal Surg. 2014 Sep;27(3):113-5
- ↑ Khadour FA, Khadour YA, Xu J, Meng L, Cui L, Xu T. Effect of neurogenic bowel dysfunction symptoms on quality of life after a spinal cord injury. J Orthop Surg Res 2023; 18(458).
- ↑ Vallès M, Terré R, Guevara D, Portell E, Vidal J, Mearin F. Alteraciones de la función intestinal en pacientes con lesión medular: relación con las características neurológicas de la lesión [Bowel dysfunction in patients with spinal cord injury: relation with neurological patterns]. Med Clin (Barc). 2007 Jun 30;129(5):171-3. Spanish.
- ↑ Kurze I, Geng V, Böthig R. Guideline for the management of neurogenic bowel dysfunction in spinal cord injury/disease. Spinal Cord. 2022 May;60(5):435-443.