Ankle and Foot Fractures
Search Strategy[edit | edit source]
We searched scientific articles and information by using PubMed, web of knowledge, Google Scholar, PEDro and Medline. We used keywords such as ankle and foot fractures, Lis franc fracture, malleolar fracture, calcaneus fracture, surgical or operative treatment and nonsurgical or conservative treatment, ankle sprain and ankle fracture. We also used some inclusion criteria as foot and ankle fractures and exclusion criteria as ankle sprain or ankle instability to find relevant articles in French or English.
Definition/Description[edit | edit source]
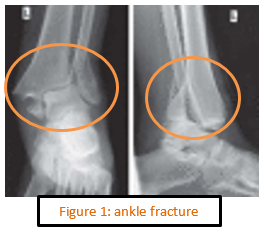
An ankle fracture is a fracture in a bone that shapes the ankle. This can be the superior articular surface of the talus, the end of the fibula (malleolus lateralis), the end of the tibia (malleolus medialis) or both (bimalleolar fracture) (Figure 1). They usually result from an external or internal rotation injury to the ankle.
Ankle fractures can range from the less serious avulsion injuries (small pieces of bone that are pulled off) to severe shattering-type breaks. The ankle ligaments, keeping the ankle in its normal position, could possibly be involved. These fractures are among the most common fractures in adults. (7) Ankle fractures are common musculoskeletal injuries that occur in a bimodal distribution. These fractures are common in younger men and older women, the former related to high-energy trauma and the latter to osteopenia and osteoporosis. (29) Ankle fractures are usually caused by falls, twisting injuries and sports injuries. (4)
A foot fracture can occur in any part of the foot (hindfoot, midfoot and forefoot). These are different types of foot fractures : calcaneal fractures, leg and foot stress fractures, metatarsal fractures (Figure 2), avulsion Fractures of the ankle, Chopart fracture, Lisfranc fracture and Pott’s fracture.

Clinically Relevant Anatomy[edit | edit source]
add text here
Epidemiology /Etiology[edit | edit source]
There are different causes for an ankle fracture:
- A big force that works into the bone. For example a kick or a smack during sport activities or a car accident.
- A little piece of the bone tears off when there is pulled at a ligament. For example when you stumble.
- Twisting or rotating your ankle
- Rolled your ankle
Characteristics/Clinical Presentation[edit | edit source]
- Difficulties or even inability to walk or load the ankle. (it is possible to walk with less severe breaks, so never rely on walking as a test of whether a bone has been fractured.
- Pain
- Swelling, along the length of the leg or more localized
- Blisters (over the fracture site).
- Bruising (soon after the injury).
- Difference in appearance.
When an ankle has been broken, there is not only structural damage to the skeletal structure, but also to the ligament tissue (deltoid ligament and the anterior and posterior tibiofibular ligaments) and possibly nervous and musculoskeletal tissue around the ankle complex.. This can result in impaired balance capacity, reduced joint position sense, slowed nerve conduction, velocity, impaired cutaneous sensation and decreased dorsal extension range of motion[1]
Differential Diagnosis[edit | edit source]
add text here
Diagnostic Procedures[edit | edit source]
To evaluate the ankle in the acute fase, we use the ‘Ottawa ankle rules’. Ottawa_Ankle_Rules
Examination[edit | edit source]
add text here related to physical examination and assessment
Outcomes Measures[edit | edit source]
Medical Management
[edit | edit source]
Most patients with a malleolus fracture require 6 weeks of immobilization. Patients with an initially non-displaced fracture or who were treated surgically will generally require 4 weeks of non-weight bearing in a short-leg cast or removable walking boot, followed by 2 weeks in a walking cast or boot. The removable boot will allow for earlier range-of-motion exercises.
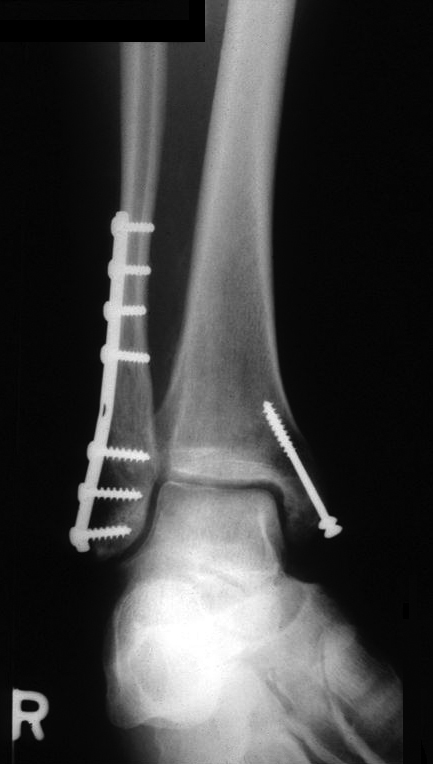
Surgery is needed for many types of ankle fractures. While not always necessary, surgery for ankle fractures is not uncommon. The need for surgery depends on the appearance of the ankle joint on X-ray and the type of ankle fracture.
Adequate reduction with congruency of the joint has been reported as one of the most important indications of a good end result. Inadequate reduction may lead to osteoarthritis.
Physical Therapy Management
[edit | edit source]
After 6 weeks of immobilization, the ankle can be fully loaded. There is no standardized rehabilitation program after cast removal. Each program is individually[1]
Physiotherapists are often involved in the rehabilitation, which starts quickly (1 week) after the period of immobilization. Most people experience pain, swelling, stiffness, muscle atrophy and decreased muscle torque[2], impaired ankle mobility, impaired balance capacity and increased ankle circumference[1] at the ankle after cast removal. Consequently, patients complain of limitation in activities involving the lower limb, such as stair climbing, walking and reduced participation in work and recreation. It has been found that patients with unimalleolar fractures report less activity limitation than those with bimalleolar or trimalleolar fractures[3]
Passive joint mobilization is commonly used to work on the problems of pain and joint stiffness, in order to allow an earlier return to activities. For this technique, the physiotherapist manually glides the articular surfaces of a joint to produce oscillatory movements. It has been proven that manual therapy, such as joint mobilization, produces analgesic effects. It also increases elasticity of joint structures through interactions at the local, central nervous system and psychological levels[4]
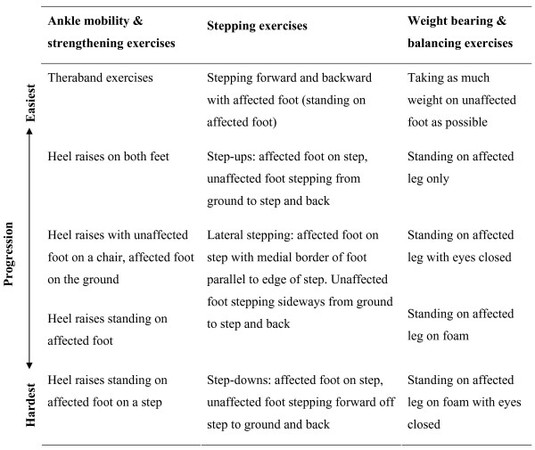
There is evidence that, after a surgical treatment for an ankle fracture, a training program, started within one week after cast removal and continued for 12 weeks (with 2 appointments per week), shows superior results compared to usual care, regarding patient scored function and muscle strength in the plantar flexors and dorsiflexors of patients under the age of 40. The patients had to do home exercises daily, prescribed by the physiotherapist, appropriate to the functional status at the time. Functional goals are loaded ankle dorsiflexion, plantairflexion, on-leg-stance, rising on toes, rising on heels, normalized walking pattern when walking on even ground, on stairs and at comfortable speed[5]
When the cast is removed, many patients have a plantarflexion contracture (http://www.physio-pedia.com/index.php5?title=Plantarflexion_contracture). This contracture is not caused directly by fracture but develops as an adaptive response to immobilization. The addition of a program of passive stretches has no benefit over exercise alone for the treatment of plantarflexion contracture after cast immobilization[6]
Key Research[edit | edit source]
Resources
[edit | edit source]
http://orthopedics.about.com/od/footanklefractures/Information_About_Foot_Ankle_Fractures.htm
http://www.foothealthfacts.org/footankleinfo/ankle-fracture.htm
http://www.invaliditeit.be/enkelbreuk.html
http://www.associatie-orthopedie-lier.be/Generic/servlet/Main.html?p_pageid=37245
http://www.dokterdokter.nl/medisch/folder/view/id/1582/gebroken-enkel
Clinical Bottom Line[edit | edit source]
The evaluation of ankle injuries is a common challenge for family physicians. Diagnosis is made by using knowledge of the anatomy and function of the ankle joint to aid in taking an adequate history and performing an appropriate physical examination. The patient should be questioned about the mechanism of injury, previous injury, disability, treatment and pain. The ankle should be evaluated for ecchymosis, swelling, areas of tenderness and laxity. These measures help to determine what, if any, additional diagnostic procedures may be needed. Most ankle sprains are lateral, affecting the anterior talofibular, calcaneofibular and posterior talofibular ligaments. Other injuries include medial ankle sprains affecting the deltoid ligament, trauma to the Achilles and peroneal tendons, tarsal tunnel syndrome, fractures, syndesmotic sprains, synovial impingement and chronic instability. Criteria for radiographic evaluation include inability to bear weight initially or when examined, and tenderness over the medial or lateral malleolus. Accurate diagnosis is critical for appropriate treatment and minimizing functional disability. (26)
Suspected injury is based on the details from the medical history, general physical examination and orthopaedic physical examination. It is important to establish the relationship between the start of painful symptoms and physical activity, generally performed repetitively, abrupt changes in the amount of training and the presence of risk factors.
Initially, pain emerges at the end of the exercises and intensifies over some weeks; it may occur during the entire activity, and be constant during walking. Pain worsens and transforms training into suffering. Training becomes increasingly painful and difficult to continue. Even after some days of rest, returning to activities too early leads to recurrence of the pain. (30)
Recent Related Research (from Pubmed)[edit | edit source]
see tutorial on Adding PubMed Feed
Extension:RSS -- Error: Not a valid URL: Feed goes here!!|charset=UTF-8|short|max=10
References [edit | edit source]
- ↑ 1.0 1.1 1.2 Nilsson G, Nyberg P, Ekdahl CH, Eneroth M. Performance after surgical treatment of patients with ankle fractures – 14-month follow-up. Physiotherapy Research International 2003, 8(2) 69-82
- ↑ Nilsson G, Jonsson K, Ekdahl CH, Eneroth M. Outcome and quality of life after surgically treated ankle fractures in patients 65 years or older. BMC Musculoskeletal Disorders 2007;8:127
- ↑ Lin CC, Moseley AM, Herbert RD, Refshauge KM. Pain and dorsiflexion range of motion predict short-and medium-term activity limitation in people receiving physiotherapy intervention after ankle fracture: an observational study. Australian Journal of Physiotherapy 2009, 55;31-37
- ↑ Lin C CH, Moseley AM, Refshauge KM, Haas M, Herbert RD. Effectiveness of joint mobilisation after cast immobilisation for ankle fracture: a protocol for a randomised controlled trial. BMC Musculoskeletal Disorders 2006;7:46
- ↑ Nilsson G, Jonsson K, Ekdahl CH, Eneroth M. Effects of a training program after surgically treated ankle fracture : a prospective randomised controlled trial. BMC Musculoskeletal Disorders 2009;10:118
- ↑ Moseley AM, Herbert RD, Nightingale EJ, Taylor DA, Evans TM, Robertson GJ, Gupta SK, Penn J. Passive stretching does not enhance outcomes in patients with plantarflexion contracture after cast immobilization for ankle fracture : a randomized controlled trial. Arch Phys Med Rehabil 2005;86 :1118-26