Action Research Arm Test (ARAT): Difference between revisions
No edit summary |
No edit summary |
||
| Line 1: | Line 1: | ||
'''<u>Purpose</u>''' | == '''<u>Purpose</u>''' == | ||
The Action Research Arm Test (ARAT) is a 19 item measure categorized into four subscales - grasp, grip, pinch and gross movement, and is used to assess upper extremity performance in stroke recovery, brain injury and multiple sclerosis. As originally described by Lyle, items are arranged in order of decreasing difficulty, with the most difficult task examined first, followed by the least difficult task. It was proposed by Lyle that this hierarchical ordering would improve efficiency of testing, as normal movement on the most difficult items would be indicative of successful performance on proceeding items (Yozbatiran, Der-Yeghiaian & Cramer, 2008). The ARAT assess an individual's activities of daily living, coordination, dexterity, and upper extremity function (Ability Lab, 2016). | |||
The | == '''<u>Populations</u>''' == | ||
The ARAT has been standardized for individuals with stroke, brain injury, Multiple Sclerosis, and Parkinson’s Disease. This test can be administered to individuals 13 years of age and older (Ability Lab, 2016). | |||
== '''<u>Required Equipment</u>''' == | |||
Lyle outlined the following testing materials as seen in Figure 1 (Heart and Stroke Foundation Canadian Partnership for Stroke Recovery, 2018): | |||
'''<u>Required Equipment</u>''' | |||
Lyle | |||
* Chair without armrests | * Chair without armrests | ||
* Table | * Table | ||
| Line 22: | Line 19: | ||
* Ball bearings | * Ball bearings | ||
* Tin lid | * Tin lid | ||
[[File:ARAT Kit.jpg|thumb|none]] | [[File:ARAT Kit.jpg|thumb|none|285x285px]] | ||
Figure 1: ARAT Kit (Rehab Solutions, 2014). | |||
Standard positioning for the ARAT has the subject seated upright in a chair with a firm back and no armrests. The head should be in a neutral position, with feet contacting the floor. This body posture must be maintained throughout the testing period, with the trunk in contact with the back of the chair. | == '''<u>Positioning</u>''' == | ||
Standard positioning for the ARAT has the subject seated upright in a chair with a firm back and no armrests. The head should be in a neutral position, with feet contacting the floor. This body posture must be maintained throughout the testing period, with the trunk in contact with the back of the chair. Feedback is provided, as required, to prevent the subject from standing up, shifting laterally or leaning forward (Yozbatiran, Der-Yeghiaian & Cramer, 2008). | |||
== '''<u>Instructions</u>''' == | |||
To ensure that test items are performed unilaterally and that the nontest hand remains visible throughout the assessment, the subject is instructed to begin with both hands pronated on the table. The exception to this rule are for tasks within the gross movement category, which require that the subject begins with bilateral forearm pronation and hands resting on the lap (Yozbatiran, Der-Yeghiaian & Cramer, 2008). | To ensure that test items are performed unilaterally and that the nontest hand remains visible throughout the assessment, the subject is instructed to begin with both hands pronated on the table. The exception to this rule are for tasks within the gross movement category, which require that the subject begins with bilateral forearm pronation and hands resting on the lap (Yozbatiran, Der-Yeghiaian & Cramer, 2008). | ||
The administrator asks the | The administrator asks the individual to perform tasks within each subscale; grasp, grip, pinch and gross movement, while scoring the individual based on their performance of that task. The administrator follows instructions provided on the scoring sheet when instructing the subject about the task. For the grasp tasks, the client will lift different materials from the surface of the table to a shelf located 37cm above the starting point. In the grip tasks, the individuals grips different types of materials and moves them from one side of the table to the other side. For the pinch tasks, the client does the same movement as the grip subscale but uses a fine motor pincer grip rather than a gross grip. Finally, for the gross movement tasks, the individual is asked to move their testing arm to different positions including on top of their head, behind their head or to their mouth (Heart and Stroke Foundation Canadian Partnership for Stroke Recovery, 2018). | ||
== '''<u>Video Explanation of ARAT</u>''' == | |||
https://www.youtube.com/watch?v=bhkCB0qojZk | https://www.youtube.com/watch?v=bhkCB0qojZk | ||
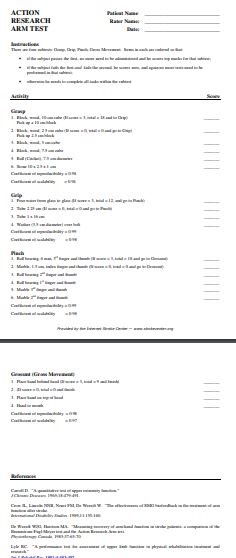
'''<u>Scoring</u>''' | == '''<u>Scoring</u>''' == | ||
The 19 items comprising the ARAT are scored using a 4 point ordinal scale, as follows: | The 19 items comprising the ARAT are scored using a 4 point ordinal scale, as follows: | ||
| Line 50: | Line 43: | ||
2 = movement task is completed but takes abnormally long | 2 = movement task is completed but takes abnormally long | ||
3 = movement is performed normally | 3 = movement is performed normally | ||
As outlined by Lyle: | |||
Subjects achieving a 3 on the (first) most difficult task are scored 3 on all remaining scale items within a subset. A score below 3 on the first item suggests that the second task must be evaluated. Subjects scoring 0 on the second task item are unlikely to be successful on subsequent scale items and are scored 0 for remaining tasks within a category. Otherwise, all test items within a category must be performed. The maximum score on the ARAT is 57 points, with the lowest score being 0 (Heart and Stroke Foundation Canadian Partnership for Stroke Recovery, 2018). | |||
[[File:ARAT scoring.jpg|none|thumb]] | |||
Figure 2: ARAT Scoring Sheet (Internet Stroke Center, 2018). | |||
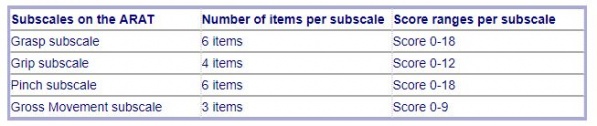
== '''<u>Interpretation</u>''' == | |||
The client first performs the most difficult task within the subscale. If the client is able to perform the test appropriately, scores 3, then all of the tasks within this subscale should be assigned a 3 as well. If the individual is unable to adequately complete the most difficult task, scoring 0-2, then the easiest task within that subscale should be performed. If the individual is unable to complete, scores 0 on the easiest task within that subscales, then the remaining moderate level tasks will not be performed and given a 0 as well. If the client scores a 1-3 on the easiest task then the administrator then gets the individuals to perform the intermediate tasks within that subscale. This is done with all 3 subscale tasks. This means individuals may perform as little as 4 tasks to as much as 19 tasks depending on the scoring and ability of the individual to complete the task. The total score is out of 57 with higher scores indicating better performance. There are no cutoff scores as this assessment scale is continuous and is based on individuals having no movement, movement or normal movement patterns (Heart and Stroke Foundation Canadian Partnership for Stroke Recovery, 2018). | The client first performs the most difficult task within the subscale. If the client is able to perform the test appropriately, scores 3, then all of the tasks within this subscale should be assigned a 3 as well. If the individual is unable to adequately complete the most difficult task, scoring 0-2, then the easiest task within that subscale should be performed. If the individual is unable to complete, scores 0 on the easiest task within that subscales, then the remaining moderate level tasks will not be performed and given a 0 as well. If the client scores a 1-3 on the easiest task then the administrator then gets the individuals to perform the intermediate tasks within that subscale. This is done with all 3 subscale tasks. This means individuals may perform as little as 4 tasks to as much as 19 tasks depending on the scoring and ability of the individual to complete the task. The total score is out of 57 with higher scores indicating better performance. There are no cutoff scores as this assessment scale is continuous and is based on individuals having no movement, movement or normal movement patterns (Heart and Stroke Foundation Canadian Partnership for Stroke Recovery, 2018). | ||
[[File:Interpretation.jpg|thumb|none|597x597px]] | [[File:Interpretation.jpg|thumb|none|597x597px]] | ||
'''<u>Reliability</u>''' | == '''<u>Reliability</u>''' == | ||
The ARAT has been shown by literature to have strong psychometric values (Song, 2012). Many domains of reliability have been tested for the ARAT with the studies unanimously showing a high reliability rating. The test retest reliability for ARAT ranges from 0.965-0.968 and the interrater reliability for ARAT ranges from 0.996-0.998 indicating high reliability for this assessment tool (Ability Lab, 2016; McDonnell, 2008). The reliability of ARAT use in Parkinson patient population has also been thoroughly tested. The test-retest reliability was found to be 0.99 as well as grip reliability to be 0.93, and gross movement reliability to be 0.99 (Song, 2012). | The ARAT has been shown by literature to have strong psychometric values (Song, 2012). Many domains of reliability have been tested for the ARAT with the studies unanimously showing a high reliability rating. The test retest reliability for ARAT ranges from 0.965-0.968 and the interrater reliability for ARAT ranges from 0.996-0.998 indicating high reliability for this assessment tool (Ability Lab, 2016; McDonnell, 2008). The reliability of ARAT use in Parkinson patient population has also been thoroughly tested. The test-retest reliability was found to be 0.99 as well as grip reliability to be 0.93, and gross movement reliability to be 0.99 (Song, 2012). | ||
'''<u>Validity</u>''' | == '''<u>Validity</u>''' == | ||
Studies have also proven ARAT to have strong validity when compared with other upper extremity function scales. Concurrent validity was shown to be high for ARAT when the assessment was compared with the upper extremity component of the Fugl-Meyer Assessment (FMA) and the Motor Assessment Scale (MAS) (McDonnell, 2008). In a comparative study, the results of ARAT in the stoke population was compared with scores on the Wolf Motor Function Test, Motor Activity Log, and the Stroke Impact Scale. The results showed good to moderate correlations between the results indicating a good predictive validity (Chen, 2012). | Studies have also proven ARAT to have strong validity when compared with other upper extremity function scales. Concurrent validity was shown to be high for ARAT when the assessment was compared with the upper extremity component of the Fugl-Meyer Assessment (FMA) and the Motor Assessment Scale (MAS) (McDonnell, 2008). In a comparative study, the results of ARAT in the stoke population was compared with scores on the Wolf Motor Function Test, Motor Activity Log, and the Stroke Impact Scale. The results showed good to moderate correlations between the results indicating a good predictive validity (Chen, 2012). | ||
'''<u>Responsiveness</u>''' | == '''<u>Responsiveness</u>''' == | ||
The ARAT has high responsiveness with this assessment tool having great ability to detect clinically significant changes in individuals upper arm motor ability in both acute and chronic phases of stroke (McDonnell, 2008). | The ARAT has high responsiveness with this assessment tool having great ability to detect clinically significant changes in individuals upper arm motor ability in both acute and chronic phases of stroke (McDonnell, 2008). | ||
'''<u>Limitations</u>''' | == '''<u>Limitations</u>''' == | ||
While ARAT has many strengths it is also plagued with some limitations that can be improved upon in the future to render the tool more trustworthy and applicable to a larger population. One limitation of ARAT is that scoring is subjective and based on the administers’ interpretation of the client's ability to do the task (Carpinella, Cattaneo & Ferrarin, 2014 & McDonnell, 2008). Also, while ARAT is known for accurately measuring moderate to high degrees of motor impairments, it has shown to have poor sensitivity for measuring mild impairment (Carpinella et al., 2014). It is also pertinent to mention that any factors the decrease the comprehension of the instructions, such as cognitive impairment or Wernicke’s aphasia, might also affect the quality of the results. | While ARAT has many strengths it is also plagued with some limitations that can be improved upon in the future to render the tool more trustworthy and applicable to a larger population. One limitation of ARAT is that scoring is subjective and based on the administers’ interpretation of the client's ability to do the task (Carpinella, Cattaneo & Ferrarin, 2014 & McDonnell, 2008). Also, while ARAT is known for accurately measuring moderate to high degrees of motor impairments, it has shown to have poor sensitivity for measuring mild impairment (Carpinella et al., 2014). It is also pertinent to mention that any factors the decrease the comprehension of the instructions, such as cognitive impairment or Wernicke’s aphasia, might also affect the quality of the results. | ||
'''<u>References</u>''' | == '''<u>References</u>''' == | ||
Ability Lab. (2016). Action research Arm Test. Retrieved on May 1st, 2018 from https://www.sralab.org/rehabilitation-measures/action-research-arm-test | |||
Ability Lab. (2016). Action research Arm Test. Retrieved from | |||
https://www.sralab.org/rehabilitation-measures/action-research-arm-test | |||
Carpinella, I., Cattaneo D., & Ferrarin, M. (2014). Quantitative assessment of upper motor | Carpinella, I., Cattaneo D., & Ferrarin, M. (2014). Quantitative assessment of upper motor | ||
function in Multiple Sclerosis using an instrumented Action Research Arm Test. Journal | function in Multiple Sclerosis using an instrumented Action Research Arm Test. Journal of Neuroengineering and Rehabilitation, Vol 11:67 | ||
of Neuroengineering and Rehabilitation, Vol 11:67 | |||
Chen, H.F., Lin K.C., Wu, C.Y., & Chen, C.L. (2012). Rasch validation and predictive validity of | Chen, H.F., Lin K.C., Wu, C.Y., & Chen, C.L. (2012). Rasch validation and predictive validity of | ||
the action research arm test in patients receiving stroke rehabilitation. Arch Phys Med | the action research arm test in patients receiving stroke rehabilitation. Arch Phys Med Rehabil, Vol 93(6), pp. 1039-1045 | ||
Rehabil, Vol 93(6), pp. 1039-1045 | |||
Heart and Stroke Foundation Canadian Partnership for Stroke Recovery. (2018). Action Research Research Arm Test (ARAT). Retrieved on May 1st, 2018 from<nowiki/>https://www.strokengine.ca/en/quick/arat_quick/ | |||
McDonnell, M. (2008). Action Research Arm Test. Australian Journal of Physiotherapy, 54. Retrieved on May 1st, 2018 from https://pdfs.semanticscholar.org/313b/7c9e2b59cbd2efc41a225d03600906b50764.pdf | |||
https:// | |||
Rehab Solutions, (2014). ARAT Kits. Retrieved on May 1st, 2018 from http://www.aratkits.com/about/ | |||
Song, CS. (2012). Intrarater Reliability of the Action Research Arm Test for Individuals with | Song, CS. (2012). Intrarater Reliability of the Action Research Arm Test for Individuals with Parkinson’s Disease. J. Phys. Ther. Sci. Vol 24: pp. 1355-1357. | ||
Parkinson’s Disease. J. Phys. Ther. Sci. Vol 24: pp. 1355-1357. | |||
Yozbatiran, N., Der-Yeghiaian, L., & Cramer, S. C. (2008). A standardized approach to | Yozbatiran, N., Der-Yeghiaian, L., & Cramer, S. C. (2008). A standardized approach to performing the action research arm test. Neurorehabilitation and Neural Repair, 22(1), 78-90. doi:10.1177/1545968307305353 | ||
performing the action research arm test. Neurorehabilitation and Neural Repair, 22(1), | |||
78-90. doi:10.1177/1545968307305353 | |||
Revision as of 20:01, 1 May 2018
Purpose[edit | edit source]
The Action Research Arm Test (ARAT) is a 19 item measure categorized into four subscales - grasp, grip, pinch and gross movement, and is used to assess upper extremity performance in stroke recovery, brain injury and multiple sclerosis. As originally described by Lyle, items are arranged in order of decreasing difficulty, with the most difficult task examined first, followed by the least difficult task. It was proposed by Lyle that this hierarchical ordering would improve efficiency of testing, as normal movement on the most difficult items would be indicative of successful performance on proceeding items (Yozbatiran, Der-Yeghiaian & Cramer, 2008). The ARAT assess an individual's activities of daily living, coordination, dexterity, and upper extremity function (Ability Lab, 2016).
Populations[edit | edit source]
The ARAT has been standardized for individuals with stroke, brain injury, Multiple Sclerosis, and Parkinson’s Disease. This test can be administered to individuals 13 years of age and older (Ability Lab, 2016).
Required Equipment[edit | edit source]
Lyle outlined the following testing materials as seen in Figure 1 (Heart and Stroke Foundation Canadian Partnership for Stroke Recovery, 2018):
- Chair without armrests
- Table
- Wooden blocks of various sizes
- Cricket ball
- Sharpening stone
- Alloy tubes
- Washer and bolt
- 2 glasses
- Sharpening stone
- Marbles
- Ball bearings
- Tin lid
Figure 1: ARAT Kit (Rehab Solutions, 2014).
Positioning[edit | edit source]
Standard positioning for the ARAT has the subject seated upright in a chair with a firm back and no armrests. The head should be in a neutral position, with feet contacting the floor. This body posture must be maintained throughout the testing period, with the trunk in contact with the back of the chair. Feedback is provided, as required, to prevent the subject from standing up, shifting laterally or leaning forward (Yozbatiran, Der-Yeghiaian & Cramer, 2008).
Instructions[edit | edit source]
To ensure that test items are performed unilaterally and that the nontest hand remains visible throughout the assessment, the subject is instructed to begin with both hands pronated on the table. The exception to this rule are for tasks within the gross movement category, which require that the subject begins with bilateral forearm pronation and hands resting on the lap (Yozbatiran, Der-Yeghiaian & Cramer, 2008).
The administrator asks the individual to perform tasks within each subscale; grasp, grip, pinch and gross movement, while scoring the individual based on their performance of that task. The administrator follows instructions provided on the scoring sheet when instructing the subject about the task. For the grasp tasks, the client will lift different materials from the surface of the table to a shelf located 37cm above the starting point. In the grip tasks, the individuals grips different types of materials and moves them from one side of the table to the other side. For the pinch tasks, the client does the same movement as the grip subscale but uses a fine motor pincer grip rather than a gross grip. Finally, for the gross movement tasks, the individual is asked to move their testing arm to different positions including on top of their head, behind their head or to their mouth (Heart and Stroke Foundation Canadian Partnership for Stroke Recovery, 2018).
Video Explanation of ARAT[edit | edit source]
https://www.youtube.com/watch?v=bhkCB0qojZk
Scoring[edit | edit source]
The 19 items comprising the ARAT are scored using a 4 point ordinal scale, as follows:
0 = no movement
1= movement task is partially performed
2 = movement task is completed but takes abnormally long
3 = movement is performed normally
As outlined by Lyle:
Subjects achieving a 3 on the (first) most difficult task are scored 3 on all remaining scale items within a subset. A score below 3 on the first item suggests that the second task must be evaluated. Subjects scoring 0 on the second task item are unlikely to be successful on subsequent scale items and are scored 0 for remaining tasks within a category. Otherwise, all test items within a category must be performed. The maximum score on the ARAT is 57 points, with the lowest score being 0 (Heart and Stroke Foundation Canadian Partnership for Stroke Recovery, 2018).
Figure 2: ARAT Scoring Sheet (Internet Stroke Center, 2018).
Interpretation[edit | edit source]
The client first performs the most difficult task within the subscale. If the client is able to perform the test appropriately, scores 3, then all of the tasks within this subscale should be assigned a 3 as well. If the individual is unable to adequately complete the most difficult task, scoring 0-2, then the easiest task within that subscale should be performed. If the individual is unable to complete, scores 0 on the easiest task within that subscales, then the remaining moderate level tasks will not be performed and given a 0 as well. If the client scores a 1-3 on the easiest task then the administrator then gets the individuals to perform the intermediate tasks within that subscale. This is done with all 3 subscale tasks. This means individuals may perform as little as 4 tasks to as much as 19 tasks depending on the scoring and ability of the individual to complete the task. The total score is out of 57 with higher scores indicating better performance. There are no cutoff scores as this assessment scale is continuous and is based on individuals having no movement, movement or normal movement patterns (Heart and Stroke Foundation Canadian Partnership for Stroke Recovery, 2018).
Reliability[edit | edit source]
The ARAT has been shown by literature to have strong psychometric values (Song, 2012). Many domains of reliability have been tested for the ARAT with the studies unanimously showing a high reliability rating. The test retest reliability for ARAT ranges from 0.965-0.968 and the interrater reliability for ARAT ranges from 0.996-0.998 indicating high reliability for this assessment tool (Ability Lab, 2016; McDonnell, 2008). The reliability of ARAT use in Parkinson patient population has also been thoroughly tested. The test-retest reliability was found to be 0.99 as well as grip reliability to be 0.93, and gross movement reliability to be 0.99 (Song, 2012).
Validity[edit | edit source]
Studies have also proven ARAT to have strong validity when compared with other upper extremity function scales. Concurrent validity was shown to be high for ARAT when the assessment was compared with the upper extremity component of the Fugl-Meyer Assessment (FMA) and the Motor Assessment Scale (MAS) (McDonnell, 2008). In a comparative study, the results of ARAT in the stoke population was compared with scores on the Wolf Motor Function Test, Motor Activity Log, and the Stroke Impact Scale. The results showed good to moderate correlations between the results indicating a good predictive validity (Chen, 2012).
Responsiveness[edit | edit source]
The ARAT has high responsiveness with this assessment tool having great ability to detect clinically significant changes in individuals upper arm motor ability in both acute and chronic phases of stroke (McDonnell, 2008).
Limitations[edit | edit source]
While ARAT has many strengths it is also plagued with some limitations that can be improved upon in the future to render the tool more trustworthy and applicable to a larger population. One limitation of ARAT is that scoring is subjective and based on the administers’ interpretation of the client's ability to do the task (Carpinella, Cattaneo & Ferrarin, 2014 & McDonnell, 2008). Also, while ARAT is known for accurately measuring moderate to high degrees of motor impairments, it has shown to have poor sensitivity for measuring mild impairment (Carpinella et al., 2014). It is also pertinent to mention that any factors the decrease the comprehension of the instructions, such as cognitive impairment or Wernicke’s aphasia, might also affect the quality of the results.
References[edit | edit source]
Ability Lab. (2016). Action research Arm Test. Retrieved on May 1st, 2018 from https://www.sralab.org/rehabilitation-measures/action-research-arm-test
Carpinella, I., Cattaneo D., & Ferrarin, M. (2014). Quantitative assessment of upper motor function in Multiple Sclerosis using an instrumented Action Research Arm Test. Journal of Neuroengineering and Rehabilitation, Vol 11:67
Chen, H.F., Lin K.C., Wu, C.Y., & Chen, C.L. (2012). Rasch validation and predictive validity of the action research arm test in patients receiving stroke rehabilitation. Arch Phys Med Rehabil, Vol 93(6), pp. 1039-1045
Heart and Stroke Foundation Canadian Partnership for Stroke Recovery. (2018). Action Research Research Arm Test (ARAT). Retrieved on May 1st, 2018 fromhttps://www.strokengine.ca/en/quick/arat_quick/
McDonnell, M. (2008). Action Research Arm Test. Australian Journal of Physiotherapy, 54. Retrieved on May 1st, 2018 from https://pdfs.semanticscholar.org/313b/7c9e2b59cbd2efc41a225d03600906b50764.pdf
Rehab Solutions, (2014). ARAT Kits. Retrieved on May 1st, 2018 from http://www.aratkits.com/about/
Song, CS. (2012). Intrarater Reliability of the Action Research Arm Test for Individuals with Parkinson’s Disease. J. Phys. Ther. Sci. Vol 24: pp. 1355-1357.
Yozbatiran, N., Der-Yeghiaian, L., & Cramer, S. C. (2008). A standardized approach to performing the action research arm test. Neurorehabilitation and Neural Repair, 22(1), 78-90. doi:10.1177/1545968307305353