Achilles Tendinopathy
1 Search Strategy[edit | edit source]
Databases Searched: Pubmed, Pedro
Keyword Searches: Achilles tendinosis, achilles tendopathy , tendinopathy ankle, tendinopathy lower limb, achilles injury
Library: Vrije Universiteit Brussel
Search Timeline: October 22, 2012 – November 25,2012
2. Definition/ Description[edit | edit source]
Achilles tendinosis, also called as Achillodynia, is a degenerative change of the Achillestendon associated with pain and often with thickening of the tendon. It is common in athletes, but it also occurs in non athletes. Surgical specimens show a range of degenerative changes of the affected tendon, such as changes in tendon fibre structure and arrangement as well as an increase in glycosaminoglycans, which may explain the swelling of the tendon.[1]
Tendinosis of the Achilles tendon is therefore a degeneration process in which no temperature rises occur, as apposed to tendonitis.
Tendinosis is often confused with tendonitis, but it is important to understand the difference between these two pathologies.
Tendonitis is an inflammation of the tendon. This inflammation causes micro-tears in the tendon when the tendon is acutely overloaded.
This diagnosis is often mistakenly used when the patiënt actually has tendinosis.
It is very important to distinguish between these disorders, to discover which treatment is required, and what the expected duration of the treatment will be.
The healing time for tendonitis is generally shorter, and commonly takes several days to 6 weeks. For tendinosis, the expected duration is variable, this can be 6-10 weeks, but it might also take 3-6 months, when the tendinosis has become chronic. [2], [3]
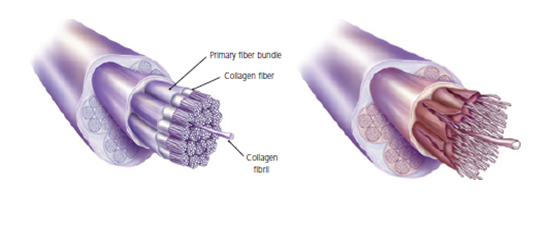
Left: The histology of a healthy tendon.
Right: The histology of a damaged tendon, in which the disorientation of the collagen fibres and the division of the fibres is clearly visible.[4]
Clinically Relevant Anatomy[edit | edit source]
Epidemiology / Etiology [edit | edit source]
The precise cause of tendinosis remains unclear. Even though tendinosis of the achilles tendon is often connected to sport activities, the ailment is also often found with people who do not practice sports. The biggest cause is the excessive overburdening of the tendon. A light degeneration of the achilles tendon can be latently present, but pain only comes into being when the tendon is overburdened. It is also noted that the ailment is usually not preceded by a trauma.[5], [6]
An inflammation is necessary to start a restoration process in the damaged tissue, but the use of certain medication, such as corticosteroids and quinolones counter the inflammation, and as a result also the restoration process. Even when the patient does not take this medication, tendinosis is also a consequence of a disrupted restoration process.[7]
6. Characteristics/Clinical presentation [8],[9],[10][edit | edit source]
Common symptoms are swelling and pain. This pain usually occurs after exercises.
With people who have a tendinopathy of the achilles tendon that has a sensitive zone, combined with intratendinous swelling, that moves along with the tendon and of which sensitivity increases or decreases when the tendon is put under pressure, there will be a high predictive value that in this situation there is a case of tendinosis.[11]
Palpation will show oversensitivity, warmth, swelling and crepitations.
Mechanism of Injury / Pathological Process[edit | edit source]
Clinical Presentation
[edit | edit source]
Diagnostic Procedures[edit | edit source]
Examination of the Achilles tendon is inspection for muscle atrophy, swelling, asymmetry, joint effusions and erythema. Atrophy is an important clue to the duration of the tendinopathy and it is often present with chronic conditions. Swelling, asymmetry and erythema in pathologic tendons are often observed in the examination. Joint effusions are uncommon with tendinopathy and suggest the possibility of intra-articular pathology. Range of motion testing is often limited on the side of the tendinopathy.[12], [13]
Palpation tends to elicit well-localized tenderness that is similar in quality and location to the pain experienced during activity.[14]
Physical examinations of the Achilles tendon often reveals palpable nodules and thickening. Anatomic deformities, such as forefoot and heel varus and excessive pes planus or foot pronation, should receive special attention. These anatomic deformities are often associated with this problem.[15], [16]
In case extra research is wanted, an echography is the first choice of examination when there is a suspicion of tendinosis.[17]
Outcome Measures[edit | edit source]
Management / Interventions[edit | edit source]
The treatment should be conservative. A popular and effective option is the eccentric strength training. Deep friction massage and stretching of the gastrocnemius and soleus are considered helpful for Achilles tedinopathy.[18]
Anatomic deformities can be treated with shoe orthotics. These shoe orthotics correct overpronation or pes planus problems.[19]
Conservative treatment: [20],[21]
In order to treat the symptoms, antiflogistics or other anti-inflammatory therapy are often used. However these forms of therapy usually cannot prevent the injury to live on.
Nevertheless patients will always have to be encouraged to execute less burdening activities, so that the burden on the tendon decreases as well. Complete immobilisation should however be avoided, since it can cause atrophy.
Passive revalidation:
Mobilisations can be used for dorsiflexion limitation of the talocrural joint and varus- or valgus limitation of the subtalar joint.
Deep cross frictions (15 min). It’s effectiveness is not scientifically proven and gives limited results. [22], [23], [24], [25]
Recently, the use of Extracorporal Shock Wave Therapy was proven.[26], [27], [28]
Besides that, the application of ice can cause a short decrease in pain and in swelling. Even though cryotherapy 2, 5 was not studied very thoroughly, recent research has shown that for injuries of soft tissue, applications of ice through a wet towel for ten minutes are the most effective measures. [29], [30], [31]
Active revalidation:
An active exercise program mostly includes eccentric exercises. This can be explained by the fact that eccentric muscle training will lengthen the muscle fibres, which stimulates the collagen production. This form of therapy appears successful for mid-portion tendinosis, but has less effect with insertion tendinopathy. The sensation of pain sets the beginning burdening of the patient and the progression of the exercises.[32], [33], [34]
Hypotheses:
Stronger/thicker tendon + strengthen pulling power
Stretching component influence on elastic tendon characteristics
↑ Collagen synthesis
↑ tendon perfusion
Sclerosing effect on neovascularisation
Normalise tendon structures [35]
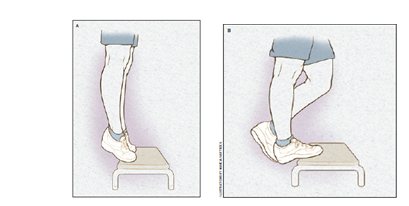
Eccentric exercise program: [36], [37]
12 weeks
perform exercises 1 to 2 times per day (7 days /week)
3 x 15 repeats
Recommended to endure pain during exercises, as long as it does not increase progressively over different days. (Should disappear 1 to 2 hours after the exercise)
Relative rest in between exercise sessions
General warm-up and stretching (for patients with limited dorsiflexion) to be integrated in the exercise sessions.
Heel drops: from toe stance lowering controllably to maximal dorsalflexion. (progression: uni- -> bilateral, with stretched -> bent knee, speed, let patient carry more than 100% of his/her body weight)10
You can also perform this exercise with a slightly bent knee, so that the soleul muscle is activated.
The calfmuscle should only be loaded eccentrically with the injured leg. The patients must use the uninjured leg (and/or) their arms to get back to the start position, so they don’t perform a concentric loading. When the eccentric loading can be performed painless, a backpack with extra weight can be added, to reach another level of painful training. [38], [39], [40], [41], [42], [43], [44]
Differential Diagnosis[edit | edit source]
Key Evidence[edit | edit source]
Resources[edit | edit source]
Case Studies
[edit | edit source]
Recent Related Research[edit | edit source]
References
[edit | edit source]
1. T E O Schubert, C. W. (2005). Achilles tendinosis is associated with sprouting of substance P positive nerve fibres. Ann Rheum Dis , 1083-1086.
Level 3B
2. K M Khan, a. p. (2002). Time to abandon the “tendinitis” myth: Painful, overuse tendon conditions have a non-inflammatory pathology . BMJ , 324:626.
Level 2A
3. Evelyn Bass, L. (2012). Tendinopathy: Why the Difference Between Tendinitis and Tendinosis Matters. Int J Ther Massage Bodywork. , 5(1): 14–17.
Level 2C
4. John J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.
Level 1A
5. MIKA PAAVOLA, M. P. (2002). Current Concepts Review Achilles Tendinopathy . THE JOURNAL OF BONE AND JOINT SURGERY, INCORPORATED , 2062-2076.
6. Dijk, M. N. (2011). Mid-portion Achilles tendinopathy: why painful? An evidence-based philosophy. Knee Surg Sports Traumatol Arthrosc , 19(8): 1367–1375.
Level 5
7. KL. Luscombe, P. S. (2003). Achilles tendinopathy. Trauma , 215-225.
Level 2C
8. Hammer, W. I. (1999). Functional Soft Tissue Examination and Treatment by Manual Methods. Aspen: Jones & Bartlett Learning.
9. Shibuya N, T. J. (2012). Is calcaneal inclination higher in patiënts with insertional achilles tendinosis? A case- controlled, cross-sectional study. The journal of foot and ankle surgery , 757-761.
Level 3B
10. Healy, N. T. (2010). Ultrasound-guided treatments for chronic Achilles tendinopathy: an update and current status . Skeletal Radiol , 39:425–434.
Level 5
11. Alex Scott, R. P. (2011). Conservative treatment of chronic Achilles tendinopathy. CMAJ , 183(10): 1159–1165.
Level 1A
12. Stasinopoulos D, S. I. (2004). Comparison of effects of exercise programme, pulsed ultrasound and transverse friction in the treatment of chronic patellar tendinopathy. Clin Rehabil , 18(4):347-52.
Level 1B
13. James Henry Cyriax, P. J. (1993). Illustrated manual of orthopaedic medicine. Oxford: Elsevier Health Sciences.
14. Joseph MF, T. K. (2012). Deep friction massage to treat tendinopathy: a systematic review of a classic treatment in the face of a new paradigm of understanding. J Sport Rehabil. , 21(4):343-53.
Level 3A
15. Rompe JD, F. J. (2008). Eccentric loading compared with shock wave treatment for chronic insertional achilles tendinopathy. A randomized, controlled trial. J Bone Joint Surg Am. , (1):52-61.
Level 1B
16. Sten Rasmussen, M. C. (2008). Shockwave therapy for achilles tendinopathy. A double-blind, randomized clinical trail of efficacy. Acta Orthopaedica , 249-256.
Level 1B
17. Bleakley C, M. S. (2004). The use of ice in the treatment of acute soft-tissue injury: a systematic review of randomized controlled trials. Am J Sports Med , (1):251-61.
Level 1A
18. Dykstra JH, H. H. (2009). Comparisons of cubed ice, crushed ice, and wetted ice on intramuscular and surface temperature changes. J Athl Train. , (2):136-41.
Level 2A
19. Brett L Woodley, R. J.‐W. (2007). Chronic tendinopathy: effectiveness of eccentric exercise. Br J Sports Med , 41(4): 188–198.
Level 1A
20. Roos EM, E. M. (2004). Clinical improvement after 6 weeks of eccentric exercise in patients with mid-portion Achilles tendinopathy -- a randomized trial with 1-year follow-up. Scand J Med Sci Sports , (5):286-95.
Level 1B
21. Fahlström M, J. P. (2003). Chronic Achilles tendon pain treated with eccentric calf-muscle training. Knee Surg Sports Traumatol Arthrosc , (5):327-33.
Level 4
22. Silbernagel KG, T. R. (2001). Eccentric overload training for patients with chronic Achilles tendon pain--a randomised controlled study with reliability testing of the evaluation methods. Scand J Med Sci Sports , (4):197-206.
Level 1B
- ↑ T E O Schubert, C. W. (2005). Achilles tendinosis is associated with sprouting of substance P positive nerve fibres. Ann Rheum Dis , 1083-1086.fckLR Level 3B
- ↑ K M Khan, a. p. (2002). Time to abandon the “tendinitis” myth: Painful, overuse tendon conditions have a non-inflammatory pathology . BMJ , 324:626.fckLR Level 2A
- ↑ Evelyn Bass, L. (2012). Tendinopathy: Why the Difference Between Tendinitis and Tendinosis Matters. Int J Ther Massage Bodywork. , 5(1): 14–17.fckLR Level 2C
- ↑ John J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.fckLR Level 1A
- ↑ John J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.fckLR Level 1A
- ↑ MIKA PAAVOLA, M. P. (2002). Current Concepts Review Achilles Tendinopathy . THE JOURNAL OF BONE AND JOINT SURGERY, INCORPORATED , 2062-2076.
- ↑ MIKA PAAVOLA, M. P. (2002). Current Concepts Review Achilles Tendinopathy . THE JOURNAL OF BONE AND JOINT SURGERY, INCORPORATED , 2062-2076.
- ↑ Dijk, M. N. (2011). Mid-portion Achilles tendinopathy: why painful? An evidence-based philosophy. Knee Surg Sports Traumatol Arthrosc , 19(8): 1367–1375.fckLR Level 5
- ↑ John J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.fckLR Level 1A
- ↑ KL. Luscombe, P. S. (2003). Achilles tendinopathy. Trauma , 215-225.fckLR Level 2C
- ↑ KL. Luscombe, P. S. (2003). Achilles tendinopathy. Trauma , 215-225.fckLR Level 2C
- ↑ . Hammer, W. I. (1999). Functional Soft Tissue Examination and Treatment by Manual Methods. Aspen: Jones & Bartlett Learning.
- ↑ KL. Luscombe, P. S. (2003). Achilles tendinopathy. Trauma , 215-225.fckLR Level 2C
- ↑ John J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.fckLR Level 1A
- ↑ John J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.fckLR Level 1A
- ↑ Shibuya N, T. J. (2012). Is calcaneal inclination higher in patiënts with insertional achilles tendinosis? A case- controlled, cross-sectional study. The journal of foot and ankle surgery , 757-761.fckLR Level 3B
- ↑ Healy, N. T. (2010). Ultrasound-guided treatments for chronic Achilles tendinopathy: an update and current status . Skeletal Radiol , 39:425–434.fckLR Level 5
- ↑ John J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.fckLR Level 1A
- ↑ John J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.fckLR Level 1A
- ↑ Alex Scott, R. P. (2011). Conservative treatment of chronic Achilles tendinopathy. CMAJ , 183(10): 1159–1165.fckLR Level 1A
- ↑ John J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.fckLR Level 1A
- ↑ . Hammer, W. I. (1999). Functional Soft Tissue Examination and Treatment by Manual Methods. Aspen: Jones & Bartlett Learning.
- ↑ Stasinopoulos D, S. I. (2004). Comparison of effects of exercise programme, pulsed ultrasound and transverse friction in the treatment of chronic patellar tendinopathy. Clin Rehabil , 18(4):347-52.fckLR Level 1B
- ↑ James Henry Cyriax, P. J. (1993). Illustrated manual of orthopaedic medicine. Oxford: Elsevier Health Sciences.
- ↑ Joseph MF, T. K. (2012). Deep friction massage to treat tendinopathy: a systematic review of a classic treatment in the face of a new paradigm of understanding. J Sport Rehabil. , 21(4):343-53.fckLR Level 3A
- ↑ John J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.fckLR Level 1A
- ↑ Rompe JD, F. J. (2008). Eccentric loading compared with shock wave treatment for chronic insertional achilles tendinopathy. A randomized, controlled trial. J Bone Joint Surg Am. , (1):52-61.fckLR Level 1B
- ↑ Sten Rasmussen, M. C. (2008). Shockwave therapy for achilles tendinopathy. A double-blind, randomized clinical trail of efficacy. Acta Orthopaedica , 249-256.fckLR Level 1B
- ↑ Bleakley C, M. S. (2004). The use of ice in the treatment of acute soft-tissue injury: a systematic review of randomized controlled trials. Am J Sports Med , (1):251-61.fckLR Level 1A
- ↑ Dykstra JH, H. H. (2009). Comparisons of cubed ice, crushed ice, and wetted ice on intramuscular and surface temperature changes. J Athl Train. , (2):136-41.fckLR Level 2A
- ↑ John J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.fckLR Level 1A
- ↑ Bleakley C, M. S. (2004). The use of ice in the treatment of acute soft-tissue injury: a systematic review of randomized controlled trials. Am J Sports Med , (1):251-61.fckLR Level 1A
- ↑ Brett L Woodley, R. J.‐W. (2007). Chronic tendinopathy: effectiveness of eccentric exercise. Br J Sports Med , 41(4): 188–198.fckLR Level 1A
- ↑ John J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.fckLR Level 1A
- ↑ Brett L Woodley, R. J.‐W. (2007). Chronic tendinopathy: effectiveness of eccentric exercise. Br J Sports Med , 41(4): 188–198.
- ↑ Rompe JD, F. J. (2008). Eccentric loading compared with shock wave treatment for chronic insertional achilles tendinopathy. A randomized, controlled trial. J Bone Joint Surg Am. , (1):52-61.fckLR Level 1B
- ↑ Roos EM, E. M. (2004). Clinical improvement after 6 weeks of eccentric exercise in patients with mid-portion Achilles tendinopathy -- a randomized trial with 1-year follow-up. Scand J Med Sci Sports , (5):286-95.fckLR Level 1B
- ↑ Brett L Woodley, R. J.‐W. (2007). Chronic tendinopathy: effectiveness of eccentric exercise. Br J Sports Med , 41(4): 188–198.fckLR Level 1A
- ↑ Fahlström M, J. P. (2003). Chronic Achilles tendon pain treated with eccentric calf-muscle training. Knee Surg Sports Traumatol Arthrosc , (5):327-33.
- ↑ John J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.fckLR Level 1A
- ↑ MIKA PAAVOLA, M. P. (2002). Current Concepts Review Achilles Tendinopathy . THE JOURNAL OF BONE AND JOINT SURGERY, INCORPORATED , 2062-2076.
- ↑ Rompe JD, F. J. (2008). Eccentric loading compared with shock wave treatment for chronic insertional achilles tendinopathy. A randomized, controlled trial. J Bone Joint Surg Am. , (1):52-61.fckLR Level 1B
- ↑ Silbernagel KG, T. R. (2001). Eccentric overload training for patients with chronic Achilles tendon pain--a randomised controlled study with reliability testing of the evaluation methods. Scand J Med Sci Sports , (4):197-206.fckLR Level 1B
- ↑ Stasinopoulos D, S. I. (2004). Comparison of effects of exercise programme, pulsed ultrasound and transverse friction in the treatment of chronic patellar tendinopathy. Clin Rehabil , 18(4):347-52.fckLR Level 1B






