Abducens Nerve
Original Editor - Innocent Abugu
Top Contributors - Innocent Abugu, Joseph Ayotunde Aderonmu, Kim Jackson and Wendy Snyders
Description[edit | edit source]
The abducens nerve is the sixth cranial nerve (CN VI). It is, along with the oculomotor nerve (CN III) and the trochlear nerve (CN IV), responsible for the extraocular motor functions of the eye. It has a purely somatic motor function, which is innervation of the lateral rectus muscle, an extraocular muscle.
Course[edit | edit source]
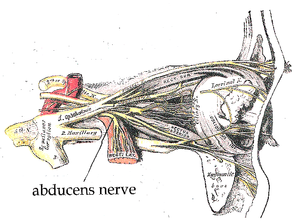
The abducens nerve emerges from the brainstem at the pontomedullary junction to enter the subarachnoid space, coursing upward between the pons and clivus to enter the Dorello canal. At the petrous apex, it angulates to enter the cavernous sinus and travels in close proximity to the internal carotid artery. The abducens nerve then proceeds through the superior orbital fissure and innervates the lateral rectus muscle.[1] It has the longest intracranial course of all the cranial nerves.
Function[edit | edit source]
The abducens nerve is a purely somatic motor nerve, It has no sensory function. It innervates the lateral rectus muscle, an extraocular muscles of the eye, which is responsible for the abduction of the eyes on the same (ipsilateral) side.
The abducens nerve is also secondarily involved in innervation of the contralateral rectus muscle by way of the longitudinal fasciculus so that both eyes move laterally in a coordinated manner.[3]
Clinical relevance[edit | edit source]
Abducens nerve palsy is the most common acquired ocular motor nerve palsy (OMNP). Patients usually present with binocular horizontal diplopia (double vision producing a side-by-side image with both eyes open), worse in the distance, an esotropia in primary gaze. Patients also may present with a head-turn to maintain binocularity and binocular fusion to minimize diplopia.[1]
Damage to the abducens nerve can be caused by anything that compresses or stretches the nerve, such as tumors, aneurysms, fractures, or increased intracranial pressure (ICP).[3]
Assessment[edit | edit source]
The abducens nerve is examined in conjunction with the oculomotor and trochlear nerves by testing the movements of the eye. The patient is asked to follow a point with their eyes (commonly the tip of a pen) without moving their head. The target is moved in an ‘H-shape’ and the patient is asked to report any blurring of vision or diplopia (double vision).[5]
Treatment[edit | edit source]
Neuromuscular re-education of the affected muscles can be an effective treatment of choice for abducens nerve palsy. It has many theoretical advantages, including noninvasiveness and avoidance of first-pass metabolism of drugs administered systemically.[6]
Other treatment of abducens nerve palsy include eye muscle exercises, prism therapy, injection of botulinium toxin, strabismus surgery.
References[edit | edit source]
- ↑ 1.0 1.1 Hajee ME, MP E. Abducens nerve palsy. E_Medicine.
- ↑ Abducens Nerve - Anatomy Tutorial. Available from: https://youtu.be/qbrv5EcQDic [last accessed 20/11/2020]
- ↑ 3.0 3.1 Nguyen V, Reddy V, Varacallo M. Neuroanatomy, cranial nerve 6 (abducens). StatPearls [Internet]. 2020 Aug 11.
- ↑ U-M Kellogg Eye Center in Ann Arbor. Sixth (6th) Cranial Nerve Palsy. Available from:https://youtu.be/Pl2ozPSWfHs [last accessed 20/11/2020]
- ↑ Radhakrishnan A. The Abducens Nerve (CN VI). Available from:https://teachmeanatomy.info/head/cranial-nerves/abducens-nerve/.
- ↑ Rongies W, Bojakowski J, Koktysz L, Dolecki W, Lewinska AO, Krzeski A. Physiotherapy in Postinfection Injury to Cranial Nerves III, IV, and VI: A Case Study. American journal of physical medicine & rehabilitation. 2019 Jun 1;98(6):e57-9.