Delayed onset muscle soreness (DOMS)
Introduction[edit | edit source]
Delayed onset muscle soreness (DOMS) also known as 'muscle fever', is a sore, aching, painful feeling in the muscles after unfamiliar or unaccustomed intense exercise. This soreness is thought to result from temporary muscle damage and inflammation, commonly triggered by eccentric exercises. Implementing recovery strategies after exercises that cause DOMS may be vital, as preventing and managing DOMS, and subsequently recovering from Exercise induced muscle damage (EIMD), are key for restoring muscular strength and performance levels. DOMS is considered a type 1 muscle strain injury, with a pain-free period of 12 to 24 hours and peak soreness between 24 to 72 hours.[2] When we engage in physical activity, our muscle cells experience minor damage. This is a normal process and isn't as harmful as it might seem. Our bodies then repair the muscle fibres, improving them slightly each time, which is how we progressively become fitter and stronger through exercise.
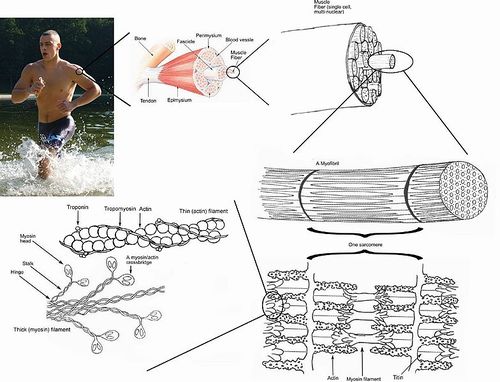
Pathophysiology[edit | edit source]
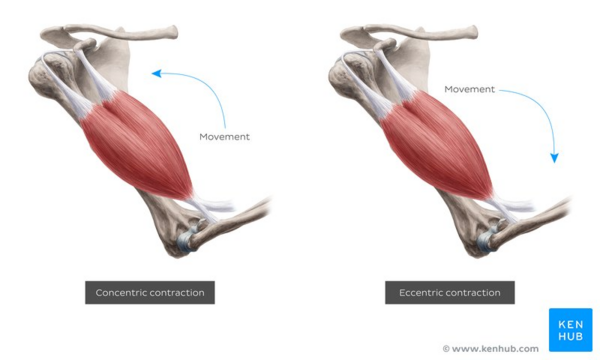
Eccentric muscle contractions result in greater disruption to the structural elements of the muscle and connective tissue than concentric exercise, which is why DOMS is more intense with eccentric than concentric forms of activity.[3] This structural disruption has sufficient evidence by histologic studies, electron microscopic examinations and serum enzyme levels which have been carried out over the years.
Eccentric contractions recruit fewer motor units and thus the force generated is distributed over a smaller cross sectional area of the muscle. This increased tension per unit area causes greater injury to the tissue.However there is still ongoing research to establish a direct causation between the muscle and connective tissue injury to the onset of DOMS.[4]
The onset of muscle soreness following exercise is multifaceted. The pain free period indicates that DOMS isn’t solely due to myofibrillar disruptions but has other underlying causes. The secondary injury model states that after the initial trauma (muscle damage or injury) the inflammatory cascade that follows can induce secondary damage.[5][6]
Neutrophils and proinflammatory macrophages are important in the removal of cell debris through phagocytosis. However, excess production of reactive oxygen species (ROS) by these inflammatory cells can cause collateral damage to healthy cells that were not involved in the initial trauma by means of denaturing the proteins, lipids and nucleic acids that make up those cells.[7][8][9]
Prevention[edit | edit source]
DOMS generally gets better on its own after a few days to a week. However, during that time range of motion and muscle performance can be reduced. Inflammation is crucial for building strength in response to a workout. Research indicates that regularly taking non-steroidal anti-inflammatory drugs (NSAIDs) for DOMS may hinder this process, potentially reducing the muscle strength gains from your training.[10] Interventions that have proven effective in prevention or recovery of DOMS include:
- Heat and cold therapy[11]
- Massage[12]
- Compression garments[13]
- Active recovery with timely rest : low intensity exercise, stretching, foam rolling, flossing[14] [15][16][17]
- Adequate sleep[18]
- Staying hydrated[16]
- Nutrition: Vitamin D, omega-3 fatty acids, branched-chain amino acids (BCAAs), antioxidant supplements[19][17]
Massage has been proven to show significant effects in reducing the intensity of the stiffness and pain felt associated with DOMS. When administered within 2 hours of activity, the mechanical pressure is believed to decrease the neutrophil migration and thus reduce the inflammatory process within the muscle structure. Massage however was shown to have no effect on muscle performance or strength post exercise when compared to a control group who were not administered the therapy[20].
Whilst heat and cold therapy have been shown to have an effect on the prevention and or recovery of DOMS, it is important to mention that cold therapy; specifically Cold Water Immersion(CWI), immediately after resistance training has been shown to attenuate gains in muscle hypertrophy. These findings are observed when CWI is applied immediately (within 15 minutes) after resistance training. Thus, it is unclear whether similar findings could be observed if CWI was applied several hours post resistance training.[21] Post-exercise Hot Water Immersion(HWI), on the other hand, has been shown to enhance muscular blood flow.[22] This may augment muscle protein synthesis and thus enhance hypertrophy. Unlike CWI which impairs blood flow and hypertrophy. [21]
Implications for Physiotherapy[edit | edit source]
Having DOMS is usually a positive sign post exercise. It indicates that the muscle is healing into a stronger state than it was before the activity and hence it means that the training was indeed effective.
Many physiotherapy clients will be starting a new exercise program or will be adding new exercises to their current exercise program. These exercises may be intense for the client and the client may experience DOMS after starting physiotherapy or exercise program. DOMS is usually weaker following subsequent exercise sessions but the first bout may be so intense that patients often refuse to continue the exercises.
Therefore, it is important for the therapist to reassure the patient that DOMS is a normal part of a new exercise program and to help the client differentiate muscle soreness from other types of pain. It is also important to note that the severity of the soreness is not related to the extent of the exercise-induced muscle damage.[23]
References[edit | edit source]
- ↑ Overview of concentric vs eccentric muscle contraction image - © Kenhub https://www.kenhub.com/en/library/anatomy/eccentric-muscle-contraction
- ↑ Gulick D, Kimura I. Delayed Onset Muscle Soreness: What Is It and How Do We Treat It?. Journal of Sport Rehabilitation. 1996;5(3):234-243.
- ↑ Basham SA, Waldman HS, Krings BM, Lamberth J, Smith JW, McAllister MJ. Effect of Curcumin Supplementation on Exercise-Induced Oxidative Stress, Inflammation, Muscle Damage, and Muscle Soreness. Journal of dietary supplements. 2019 Apr 26:1-4.
- ↑ Postexercise Muscle Soreness [Internet]. Sickle Cell Anemia Differential Diagnoses. 2017 [cited 2019Mar1]. Available from: https://emedicine.medscape.com/article/313267-overview#a5
- ↑ Toumi H. The inflammatory response: friend or enemy for muscle injury?. British Journal of Sports Medicine. 2003;37(4):284-286.
- ↑ Knight K, Brucker J, Stoneman P, Rubley M. Muscle Injury Management with Cryotherapy. Athletic Therapy Today. 2000;5(4):26-30.
- ↑ Bleakley C, Davison G. Cryotherapy and inflammation: evidence beyond the cardinal signs. Physical Therapy Reviews. 2010;15(6):430-435.
- ↑ Nguyen H, Tidball J. Interactions between neutrophils and macrophages promote macrophage killing of rat muscle cells in vitro. The Journal of Physiology. 2002;547(1):125-132.
- ↑ Powers S, Jackson M. Exercise-Induced Oxidative Stress: Cellular Mechanisms and Impact on Muscle Force Production. Physiological Reviews. 2008;88(4):1243-1276.
- ↑ Cornu C, Grange C, Regalin A, Munier J, Ounissi S, Reynaud N, Kassai-Koupai B, Sallet P, Nony P. Effect of non-steroidal anti-inflammatory drugs on sport performance indices in healthy people: a meta-analysis of randomized controlled trials. Sports Medicine-Open. 2020 Dec;6:1-1.
- ↑ Wang Y, Li S, Zhang Y, Chen Y, Yan F, Han L, Ma Y. Heat and cold therapy reduce pain in patients with delayed onset muscle soreness: A systematic review and meta-analysis of 32 randomized controlled trials. Physical Therapy in Sport. 2021 Mar 1;48:177-87.
- ↑ Guo J, Li L, Gong Y, Zhu R, Xu J, Zou J, Chen X. Massage alleviates delayed onset muscle soreness after strenuous exercise: a systematic review and meta-analysis. Frontiers in physiology. 2017 Sep 27;8:747.
- ↑ Kim J, Kim J, Lee J. Effect of compression garments on delayed-onset muscle soreness and blood inflammatory markers after eccentric exercise: a randomized controlled trial. Journal of exercise rehabilitation. 2017 Oct;13(5):541.
- ↑ La Shier SV. Effect of Therapeutic Treatment on Delayed Onset Muscle Soreness (DOMS).
- ↑ Song SH. Effects of rest interval following eccentric muscle contraction exercise on circulating substance, parameters related to damage and regeneration in skeletal muscle. The Official Journal of the Korean Academy of Kinesiology. 2013 Oct 31;15(4):107-15.
- ↑ 16.0 16.1 Zeng C, Luo G, Xu S, Li Y. The application of DOMS mechanism and prevention in physical education and training. Journal of Healthcare Engineering. 2022 Jan 7;2022.
- ↑ 17.0 17.1 Heiss R, Lutter C, Freiwald J, Hoppe MW, Grim C, Poettgen K, Forst R, Bloch W, Hüttel M, Hotfiel T. Advances in delayed-onset muscle soreness (DOMS)–part II: treatment and prevention. Sportverletzung· Sportschaden. 2019 Mar;33(01):21-9.
- ↑ Palsson TS, Rubio-Peirotén A, Doménech-García V. Sleep deprivation increases pain sensitivity following acute muscle soreness. Sleep Medicine. 2023 Sep 1;109:75-81.
- ↑ Basham SA, Waldman HS, Krings BM, Lamberth J, Smith JW, McAllister MJ. Effect of Curcumin Supplementation on Exercise-Induced Oxidative Stress, Inflammation, Muscle Damage, and Muscle Soreness. Journal of dietary supplements. 2019 Apr 26:1-4.
- ↑ 2. J E Hilbert, G A Sforzo, T Swensen. The effects of massage on delayed onset muscle soreness. Br J Sports Med 2003;37:72–75 ; (): . (accessed 18 February 2018).
- ↑ 21.0 21.1 Piñero A, Burke R, Augustin F, Mohan AE, DeJesus K, Sapuppo M, et al. Throwing cold water on muscle growth: A systematic review with meta‐analysis of the effects of postexercise cold water immersion on resistance training‐induced hypertrophy. EJSS/European Journal of Sport Science [Internet]. 2024 Feb 5;
- ↑ Steward CJ, Hill M, Menzies C, Bailey SJ, Rahman M, Thake CD, et al. Post exercise hot water immersion and hot water immersion in isolation enhance vascular, blood marker, and perceptual responses when compared to exercise alone. Scandinavian Journal of Medicine & Science in Sports [Internet]. 2024 Mar 1;34(3).
- ↑ Nosaka K, Newton M, Sacco P. Delayed‐onset muscle soreness does not reflect the magnitude of eccentric exercise‐induced muscle damage. Scandinavian journal of medicine & science in sports. 2002 Dec 1;12(6):337-46.