Thoracentesis
Description[edit | edit source]
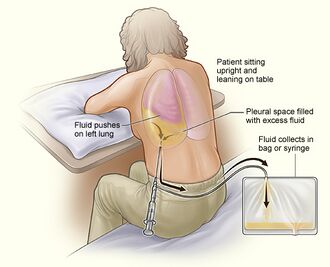
Thoracentesis is a minimally invasive procedure that involves removing excessive fluid or air from the lungs by injecting a hollow needle through the chest wall and into the pleural space after the administration of local anesthesia. This procedure can be done in either a sitting or supine position depending on the patient's comfort and his underlying condition[1].
Indication[edit | edit source]
Thoracentesis is done whenever there is excessive fluid in the space between the lungs and the chest wall. It is considered a diagnostic procedure when the presence of excessive fluid is of unknown etiology where the healthcare professional collects a small volume of the fluid, typically using a single 20cc to 30cc syringe, for laboratory and pathological analysis[2]. In addition to that, it is also considered a therapeutic procedure when the present excessive fluid is causing significant clinical symptoms and after the failure of initial medical management such as the use of diuresis and treatment of the underlying cause which can be congestive heart failure, cancer, pneumonia, autoimmune diseases such as lupus, tuberculosis or pulmonary hypertension[3].
Clinical Presentation[edit | edit source]
Resources[edit | edit source]
References[edit | edit source]
- ↑ LeVasseur RA. Thoracentesis. In: Richardson JD, Bland KI, editors. The Mont Reid Surgical Handbook. 6th ed. Philadelphia, PA: Saunders/Elsevier; 2008. p. 835-838.
- ↑ Terra RM, Vega AJ. Treatment of malignant pleural effusion. Journal of Visualized Surgery. 2018;4.
- ↑ Leo F, Makowska M. Thoracentesis-Step by Step. Deutsche Medizinische Wochenschrift (1946). 2018 Aug 7;143(16):1186-92.