Biopsychosocial Considerations for Clinicians when ordering MRI for Low Back Pain
Introduction[edit | edit source]
George Engels Biopsychosocial Model[edit | edit source]
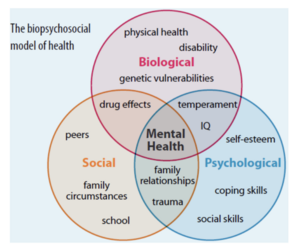
George Engel’s 1977, biopsychosocial model was introduced to negate the previous medical or biological model; it encompasses the social and psychological factors of illness.
- Bio – the physical, how does the condition present?
- Psychological – what are the patient’s beliefs about the pain? What was their psychological state before the illness or injury?
- Social – what does this person do for work? What is their family situation? What is their support network? What are their commitments? What external factors could have caused this condition to present?
MRI Magnetic resonance Imaging (MRI) A map of hydrogen atoms within the body. Hydrogen atoms are perfect for MRI as they only have a single proton with a large magnetic moment.
- In Layman’s terms, an MRI scanner is a large and powerful magnet which gives us an image of the patient.
- There is a magnetic field created by magnets causing resonance from each proton in the hydrogen atom then the machine can obtain the proton’s position.
- 75% of our bodies are made from water molecules, therefore, MR imaging can capture precise and detailed images.
- Each type of cell emits a distinct signal, which allows the identification of bones, joints, muscle, and cartilage.
- The MRI takes a detailed "picture" of all hydrogen molecules in the body and is computed into an accurate representation of that body region.
Chronic Lower Back Pain (CLBP)[edit | edit source]
Low back pain that continues for 12 weeks or more because of an initial injury or an underlying cause of acute back pain.
- Develops in 5-10% of lower back pain cases.
- The second leading cause of disability worldwide.
- Significant influence of psychological factors e.g., anxiety/depression, (Allegri et al., 2016)
- Increased prevalence with age, where individuals over 50 are 3-4 times more likely to have CLBP than those aged 18-30.
- Diagnosis of CLBP is commonly affirmed from a patient's history.
MRI and CLBP[edit | edit source]
Imaging findings, such as disk degeneration, facet arthropathy, and disk herniations, have been attributed as causative factors for LBP. However, in many cases, these findings are asymptomatic, (Rao et al., 2018) . Nevertheless, in some cases, it can be symptomatic andhighly painful, if this is missed in the acute phase it could also become a contributing factor of CLBP Less than 10% of cases are diagnosed with magnetic resonance imaging (MRI).
Literature synthesises that MRI is the optimal imaging choice when detecting spinal pathologies. (REFERENCE WB)
Biological Considerations[edit | edit source]
link to LBP guidelines
The American college of physicians guidelines discourage the routine use of MRI in patients with chronic LBP. They recommend MRI to be reserved for patients with severe or progressive neurological symptoms, or those with signs of radiculopathy or spinal stenosis. (Reference TE). In patients with chronic LBP who undergo MRI, 52-82% will present with degenerative changes. (reference TE).
Abnormalities found on MRI have little prognostic value, for both symptoms and and level if patient disability.(Reference TE). When considering long term outcomes, very few abnormalities or degenerative changes can indicate worse outcomes for patients. (Reference TE). In patients followed up 13 years after their MRI, it has been reported that any changes identified on their MRI were not associated with worse outcomes. (Reference TE).
Symptomatic populations[edit | edit source]
The evidence suggests that in patients with symptomatic lumbar spinal disorders, there is no benefit when comparing early and late MRI. It must be noted that for both study populations, the resulting clinical interventions were very similar between the two groups. A slightly higher Aberdeen LBP score was noted in the group receiving the early MRI, however it must be left up to clinicians in their own healthcare systems to make a judgement as to whether this benefit justifies the additional cost.
When comparing the results of symptomatic patients having an MRI against those who don't go on to have an image, the only difference is the level of diagnostic confidence. As before, there was no difference observed in either diagnostic or therapeutic decision making. It is interesting to note that both groups saw a statistically significant increase in both diagnostic and therapeutic confidence of the participants, when comparing figures from trial entry and follow up. (Reference TE). This evidence highlights the confidence of patients in their treatment, despite the group they were in. In agreement with the previous studies presented, this study reiterates that without the presence of serious pathological indicators, treatment decisions will be very similar with or without the results of an MRI.
Psychological Considerations[edit | edit source]
link to patient perceptions
Clinician Beliefs[edit | edit source]
- Some clinicians believe clinical presentations from diagnostic imaging are useful in locating sources of low back pain. As so, with patients’ exaggerated behaviours, clinicians can be fearful of missing serious pathologies and thus choosing to utilise diagnostic imaging. Primary care clinicians have stated referring patients for imaging even though it may not be necessary at times, partly to reduce risks of legal repercussions and to manage patient expectations (link).
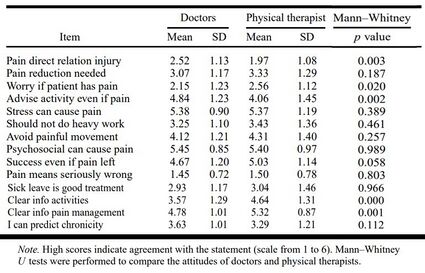
- Fear-avoidance scores of physiotherapists were examined through a modified questionnaire (link)
- Over 33% believed reduced pain to be a prerequisite for returning to activities.
- Over 66% reported that they would advise patients to avoid painful movements
- Over 25% believed sick leaves as a good treatment for low back pain.
- These statistics correlated with relatively high mean statement scores from physiotherapists, suggesting adverse practices of advising to avoid painful movements (mean=4.31), avoiding heavy work (mean=3.43), and believing sick leave to be a good treatment (mean=3.04)
- Moreover, clinicians have also expressed a lack of awareness of the most up-to-date back pain guidelines and knowledge on how to apply them in practice. This in turn dictated many treatment orientations, with clinicians approaching low back pain patients with a biomedical model instead of the biopsychosocial model (link). A SR of quantitative and qualitative studies has shown physiotherapists focusing mainly on physical pathologies and addressing symptoms of impairment during sessions. They reported disliking treating difficult patients and had poor outcome expectancies for these treatments. Physiotherapists generally felt unconfident in treating with a biopsychosocial model, having low self-efficacy and presuming assessment of psychosocial factors were not part of their roles (link).
- This shows a preference for physiotherapists to treat biological issues. Yet, rather than practicing with strong biomedical focuses, physiotherapists should embrace the idea that functional impairments and pain may be influenced by other psychosocial factors (link). SR supports this by reporting a biopsychosocial approach is superior to a biomedically focused approach in chronic low back pain (Link)
Patient Demands[edit | edit source]
- Patients with low back pain believes pathoanatomical findings on diagnostic imaging can provide credible explanations to support their chronic experiences pain to be real. They hope for these realistic evidence to provide a sense of reassurance and relieve to patients who may have felt stigmatised with their symptom presentations. They are shown to deeply value such results and often chooses to use the information in convincing other medical professionals, family, friends, and colleagues. (link). Hence, patients are shown to have strong desires to receive imaging for specific diagnosis, hoping to legitimise their experiences of pain by providing information about the causes, underlying pathologies, and to rule out potential sinister causes.
- Research data suggests that up to half of all LBP patients expected some form of imaging from healthcare providers (Reference), suggesting patients to be persistent in demanding for diagnostic imaging. A 2020 SR also showed numerous qualitative interview studies to have found patients initiating referrals for imaging if it was not suggested by the clinician (link). An account from a patient by Rhodes et al described asking for a referral continuously until it was accepted (link).
- Additionally, with LBP often recurring for prolonged periods (link), some patients also believed that imaging can identify the cause better than physical exams from clinician and in turn facilitate a more tailored approach to treatment. Expectations for tailored approach includes personalised information about self-management strategies and the available support services related to both healthcare and occupational issues (link).
- For clinicians, this provides a challenge as patients will often demand such imaging and are likely to be insistence, potentially swaying clinicians even though they may be aware of optimal approaches. Physiotherapists are shown to be easily influenced, with them likely to make clinical decisions based on therapist-patient relationships and patient characteristics, such as the perceived “passivity of patients” (link).
- As seen, although clinicians are aware of the consequences of unnecessary imaging, patients rarely considered the potential for harm and can often insist on imaging. For which it can contribute towards a clinician’s decision for ordering diagnostic imaging.
Contextual Factors[edit | edit source]
Following on from clinicians not being aware of up-to-date guidelines, if institutional policies regarding imaging are not aligned to the latest evidence, then clinicians may also face confusion when in deciding to order diagnostic imaging. This may be exacerbated in recent times, with many International Consensus Conferences being halted due to the global pandemic and thus potentially not catching up to new research.
Furthermore, staffing may also be scarce and to avoid backlog of patients, clinicians must keep sessions quick simultaneously in maintaining a satisfactory turnover rate to see all patients assigned. A quote from a clinician in a qualitative study encompasses this perfectly: “Sometime I find myself referring a patient for X-ray in order to clear the waiting room and allow myself two minutes of breathing time. Meanwhile the patient keeps quiet, while I write the referral. Sometimes you find yourself doing this and it goes against any reasoning or logic” (link).
Social Considerations[edit | edit source]
Key Facts
- Currently, for every ten patients presenting to primary care with LBP, one receives advanced imaging. [1]
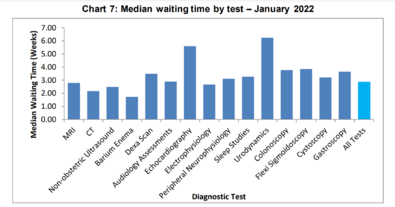
- At the end of January 2022 the NHS estimated nationally there were 280,139 patients awaiting an MRI. (REFERENCE WB)
- Early MRIs (withing the first month) for LBP often result in greater periods of disability for patients when compared to those who receive negative findings or no imaging, leading to increased health care costs. [2]
Waiting Times
In 2023, the current average estimated waiting time is 6-18 weeks for an outpatient MRI scan. It is estimated that 26% of outpatients in 2023 have waited longer thank 6 weeks for an MRI. [3] Waiting lists for outpatient MRI scans have significantly increased in recent years, with the number of patients waiting six weeks plus increasing from 2.5% in August 2019, to 28.1% in August 2020.[4] COVID-19 is one of the route causes of this backlog alongside funding cuts to nationwide healthcare services. The prioritisation of urgent over non-urgent cases post COVID-19 has resulted in further growth of waiting times. (FIND REFERENCE)
Costs & Funding
The cost for a single low back MRI in the UK can cost the NHS around £200 to £500 depending on provider and type of scan. (Reference)
Currently in the NHS there is a lack of funding and deep routed staffing issues [5]. With inadequate funding, clinicians may be faced with less individual patient contact time. Large wait times have resulted in clinicians being required to see a high threshold of patients on a daily basis. This can lead to insufficient time in explaining and justifying non-imaging approaches, as supported by a focus group interviews where clinicians reported lacking time in conversing with patients about diagnoses and why a scan was not needed. [6]
Imaging has direct and in-direct costs. One study found that 80% of patients with LBP would undergo radiography if they had the choice, despite no benefits of routine imaging. [7] Patients often misinterpret positive MRI findings as more severe and specific pathologies, even when these findings are clinically unrelated to the presenting symptoms. This leads to further patients requests of medical interventions resulting in increased healthcare costs. [8]
Conclusion[edit | edit source]
Reference List
- ↑ Beattie PF, Meyers SP. Magnetic Resonance Imaging in low back pain: General principles and clinical issues. Physical Therapy. 1998;78(7):738–53. doi:10.1093/ptj/78.7.738
- ↑ Mahmud MA, Webster BS, Courtney TK, Matz S, Tacci JA, Christiani DC. Clinical management and the duration of disability for work-related low back pain. Journal of Occupational and Environmental Medicine. 2000;42(12):1178–87. doi:10.1097/00043764-200012000-00012
- ↑ Wood J. Your guide to MRI waiting Times - NHS vs private. 2023 [cited 2023 May 17]. Available from: https://practiceplusgroup.com/knowledge-hub/mri-waiting-times/
- ↑ NHS England and NHS Improvement; 2020 [cited 2023 May 17]. Available from: https://www.england.nhs.uk/statistics/wp-content/uploads/sites/2/2020/10/DWTA-Report-August-2020_o1lg9.pdf
- ↑ Buchan J, Charlesworth A, Gershlick B, Seccombe I. The Health Foundation; 2019 [cited 2023 May 17]. Available from: https://www.health.org.uk/sites/default/files/upload/publications/2019/A%20Critical%20Moment_1.pdf
- ↑ Espeland A, Baerheim A. Factors affecting general practitioners’ decisions about plain radiography for back pain: Implications for classification of guideline barriers – a qualitative study. BMC Health Services Research. 2003;3(1). doi:10.1186/1472-6963-3-8
- ↑ Kendrick D. Radiography of the lumbar spine in primary care patients with low back pain: Randomised controlled trial. BMJ. 2001;322(7283):400–5. doi:10.1136/bmj.322.7283.400
- ↑ Mahmud MA, Webster BS, Courtney TK, Matz S, Tacci JA, Christiani DC. Clinical management and the duration of disability for work-related low back pain. Journal of Occupational and Environmental Medicine. 2000;42(12):1178–87. doi:10.1097/00043764-200012000-00012