Psychosocial Considerations in Patellofemoral Pain
Top Contributors - Carin Hunter, Jess Bell, Ewa Jaraczewska, Kim Jackson and Wanda van Niekerk
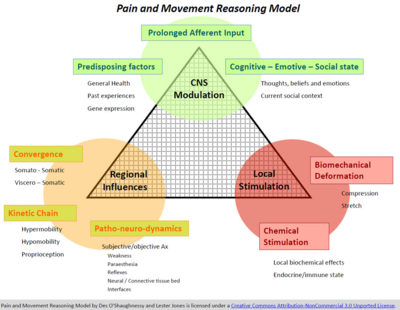
Pain and Movement Reasoning Model , (Jones & O’Shaughnessy,2014)[edit | edit source]
When considering the psychosocial factors affecting the patellofemoral joint, even though the pain and movement reasoning model was not designed for patellofemoral pain, the theory can be effectively applied.
Factors in the Pain and Reasoning Model[edit | edit source]
- Local Stimulation
- Biomechanical Stimulation - Bone oedema, fat pad swelling, effusion, retinacular ischaemic changes, bone bruising, or anything local at the knee.
- Chemical Stimulation
- Regional Influences
- Kinetic Chain - Excessively pronating foot, anteverted femoral neck or poor control of their hip abduction
- Patho-neuro-dynamics
- Convergence
- Central Nervous System Modulation - Minimal research on this area
- Prolonged Afferent Input
- Predisposing Factors
- Cognitive - Emotive - Social state
Pain Experience[edit | edit source]
Mindfulness[edit | edit source]
- Wride's work shows that the prevalence of anxiety and/or depression is way higher in the patellofemoral population than the normal population. Now, we do know that anxiety and depression is higher in young females anyway, and we know that a lot of patellofemoral pain is in females, but given that still, the rates are much, much higher.
- people felt a sense of loss of identity and, in line with that, a loss of social interactions. And a lot of that is because, for some patients, this comes on through their sport. And even actually, if it doesn't come on because of the sport, it may well stop them doing their sport. So, if you go to a running club or you play football in a team, and then suddenly you can't do that, you don't just lose the sport, you lose everything that, that brings to you and that can be a sense of wellbeing and social interactions, absolutely, as well.
- patients were voicing that they were even changing their career aspirations because of their patellofemoral pain. That's really big when you stop and think about it. And then he also found that there was an overarching belief that exercise was bad because exercise had caused it in a lot of the patients and, therefore, they couldn't understand why physiotherapy and physiotherapists prescribing exercise could possibly help them because they believed that exercise was harmful. And that's an interesting one, isn't it? When you stop thinking about it, you think, well, of course, so we need to take time don't we, to educate around this, educate the understanding just because it came on through exercise doesn't mean that all exercise is bad? And in fact, it's not just about is an exercise good or bad? It's about load, repetitive volume, warm up, cool down, footwear, there were so many other facets to understanding exercise
- But we need to understand that if a patient comes to us with patellofemoral pain with the belief that exercise has caused their pain, they're quite rightly, perhaps, going to be a bit dubious about doing exercise-based treatments and, rather sadly, in line with that, the treatments that the patients felt were most likely to be helpful were very passive, were painkillers, knee supports, and rest. And we know, certainly, that even though people might feel temporarily better from rest and painkillers, it's not the way to sort out patellofemoral pain.
- insidious onset, it's the same issue. People want to make sense of it and they can't.
- in line with that, my talk on my course on adolescent patellofemoral pain looks at Selhorst's work, working with a psychologist to help their patients understand what patellofemoral pain is, what are the likely consequences, are they are able to impact on it, what are the likely timelines? And their eight-minute video showed a reduction in kinesiophobia, catastrophisation, pain scores, immediately and at two weeks. So, there's no physical treatment that would give those results. So, again, showing the power of education and we need to particularly do this with this insidious onset condition, it's incredibly important.
- sleep's another really interesting area, very much now, emerging literature coming through, looking at the fact that you're more likely to sustain a musculoskeletal injury and struggle to recover from it if you have poor quality sleep. And more sensitive assessments of sleep don't just look at volume, they look at quality. How many times does someone wake up in the night? How long does it take to get to sleep? So that we get a true reflection of sleep. And we know that when you sleep well, you are more likely to produce your natural painkillers.
- Tampa Score of Kinesiophobia
- Bagheri's work showing that physical treatment, sort of standardised typical patellofemoral treatments, with mindfulness was more effective at pain reduction, catastrophisation, kinesiophobia than the same physical treatment. Mindfulness, that's great to see that paper. That's the first paper I've ever seen on, and I'm sure it is, on mindfulness and patellofemoral pain, but why not? It's all around stress reduction, being able to take control of the situation, stay in control, and not be overly alarmed by it
- And, you know, the irony is if we do great physical treatments, maybe someone is more flexible or stronger, their foot sorted out with an orthotic or whatever it may be, we may think - and even their pain might be less - we might feel oh, you know, I've done a good job there. But if they leave your room and they still avoid the stairs because their belief is that it's harmful to them if their knee is noisy on the stairs, or if they still feel highly anxious about doing their sport, or they still avoid going back to their running club because they feel that running bought it on in the first place and that pain meant damage, we have not addressed those psychosocial considerations that really are absolutely as big an issue as any physical thing around the knee.
- Ben Smith's fantastic qualitative work and Wride's work in 2018
- Bagheri et al., 2021. PFP exs vs exs+mindfulness.
- Mindfulness aimed at increasing awareness of thoughts, sensations, emotions all with an attitude of acceptance, curiosity and openness.
- Better pain, less catastrophizing, less kinesiophobia w mindfulness.
- There is little written about anxiety and depression in PFP but Wride et al., 2019 work in the UK reveals the following key facts regarding the prevalence of anxiety and depression in the PFP population, (n=400):
- 49.5% demonstrated anxiety.
- 20.8% indicated depressive symptoms.
- When combined, 53% were living with anxiety +/or depression.
- Patients with a high anxiety score were significantly younger.
- Patients with a high anxiety score were more likely to be female.
Key Questions to ask and why[edit | edit source]
| Question | Reason | Treatment Implication |
| Duration of symptoms | The longer the duration the more likely there will be central pain changes. | Assess for central changes |
| Alteration in sleep quality? | Serotonin (natural painkiller) production suppressed with poor sleep | Recommend re-establishing routine. Non-painful exercise.
Decrease anxiety through education |
| Change in exercise profile? | Can affect sleep, mood, self-esteem, social interactions and conditioning. | Consider exercise programmes for non-painful body parts initially.
Education to minimise fear-avoidance. |
| Can they tolerate the sense of clothing on their knee, eg skinny jeans/tights? | Some patients cannot bear the feeling of material on their knee. Highly suggestive of non-mechanical pain. | Graduated exposure. May need medical management to de-sensitise. |
References[edit | edit source]
- Jones & O’Shaughnessy,2014
- Bagheri et al., 2021
- Wride et al., 2019